What is the Medicare Coverage Determination process?
· Step 1. Choose Original Medicare or Medicare Advantage. This is the biggest decision when signing up for Medicare. You can get Medicare benefits either through Original Medicare (sometimes called Traditional Medicare) or a Medicare Advantage plan. Which one is right for you depends on your situation and preferences.
Are there different election periods for Medicare?
You have the same rights and protections as all people with Medicare. You also have the right to: Get a written explanation for drug coverage decisions (called a “coverage determination”) from your Medicare drug plan. A coverage determination is the first decision your Medicare drug plan (not the pharmacy) makes about your benefits.
What should I do if I'm turning 65 and want Medicare?
As you near age 65, you need to learn about Medicare coverage choices and make several important enrollment decisions. This fact sheet will give you a list of the steps you should . take and tell you about resources to help you make your Medicare enrollment decisions. There can be penalties if you do not enroll on time, so it is best to complete these tasks at least 3 months …
Can I make changes to my Medicare coverage anytime?
· Learn More To learn about Medicare plans you may be eligible for, you can:. Contact the Medicare plan directly. Call 1-800-MEDICARE (1-800-633-4227), TTY users 1-877-486-2048; 24 hours a day, 7 days a week. Contact a licensed insurance agency such as eHealth, which runs Medicare.com as a non-government website.
What is the deadline for choosing a Medicare plan?
Medicare Advantage Open Enrollment Period. From January 1 – March 31 each year, if you're enrolled in a Medicare Advantage Plan, you can switch to a different Medicare Advantage Plan or switch to Original Medicare (and join a separate Medicare drug plan) once during this time.
How long does it take for approval of Medicare?
It takes about 45 to 90 days to receive your acceptance letter after submitting your Medicare application.
Does Medicare start on the first day of the month you turn 65?
When your coverage starts If you qualify for Premium-free Part A: Your Part A coverage starts the month you turn 65. (If your birthday is on the first of the month, coverage starts the month before you turn 65.)
How do I check the status of my Medicare application?
How to Check Medicare Application StatusLogging into one's “My Social Security” account via the Social Security website.Visiting a local Social Security office. ... Contact Social Security Administration by calling 1-800-772-1213 (TTY 1-800-325-0778) anytime Monday through Friday, 7 a.m. to 7 p.m.More items...•
When does Medicare start?
For most people, Medicare coverage begins the first day of the month they turn age 65 . If your client has already started receiving Social Security benefits, they’ll automatically be signed up for Medicare Part A and Part B. If they haven’t yet made a Social Security benefit claim, they’ll need to submit a Medicare application.
When does Medicare enrollment start?
General enrollment period: Those who missed their IEP and SEP can sign up during Medicare’s General Enrollment Period (Jan. 1 to March 31) with coverage taking effect on July 1.
How long do you have to pay Medicare premiums if you wait two years?
So, if your client waits two years beyond their first eligibility to enroll, they’ll be required to pay the higher premiums for four years. Part D: While typically small, penalties for late enrollment in a Medicare prescription plan are assessed for as long as individuals have coverage.
What is Medicare consists of?
Medicare consists of an alphabet soup of plans, coverage choices, premium levels and enrollment rules. All that said, there are a few key decisions your client will be required to make regarding their Medicare coverage:
What is a Medigap plan?
Medigap is offered by private insurers to help fill any coverage gaps in Part A and Part B such as copayments, coinsurance, deductibles and potentially foreign travel health emergencies. There are 10 different types of Medigap plans—some cover more out-of-pocket costs than others.
How old do you have to be to get Medicare?
Medicare is generally available to anyone age 65 or older (as well as to younger people with qualifying disabilities). Part A is available premium-free if your client paid Medicare taxes for at least 10 years (40 quarters) of their working life.
How long does a SEP last?
In this case, they’ll be required to enroll for Part A and/or Part B during their special enrollment period (SEP) that begins the month after their employment or group coverage ends (whichever comes first) and lasts for eight months.
When is the annual election period for Medicare?
The AEP takes place from October 15 to December 7 every year. During AEP, you may generally:
When do you get your annual notice of change from Medicare?
If you’re already enrolled in Medicare Advantage or a Medicare Prescription Drug Plan, you may want to carefully review your plan’s Evidence of Coverage and Annual Notice of Change documents, which are mailed out every fall before AEP. These documents provide detailed information on your plan’s coverage for the upcoming year, as well as any changes in benefits or costs. If a health service you rely on or a medication you take is no longer covered, your plan will notify you in these documents.
What is the rating of Medicare Advantage?
Ratings — All Medicare Prescription Drug Plans and Medicare Advantage plans are rated on a scale of 1 to 5 stars for quality and customer satisfaction, with a 5-star rating indicating excellence.
What happens if you don't have Medicare?
If you don’t have Medicare prescription drug coverage, but have other prescription drug coverage, verify that your coverage is still considered “creditable”— that is, coverage that’s expected to pay at least as much, on average, as standard Medicare prescription drug coverage.
When does Medicare Part D end?
If you disenroll from a Medicare Advantage plan that included prescription drug coverage, you will also have an opportunity to enroll in a stand-alone Medicare Part D Prescription Drug Plan starting January 1 and ending March 31.
How does Medicare evaluate plans?
Medicare evaluates plans based on a 5-star rating system. Star ratings are calculated each year and may change from one year to the next.
Does Medicare Part A cover dental?
If you’re currently enrolled in Original Medicare, Part A and Part B, you might consider signing up for a Medicare health plan to receive coverage not included in Original Medicare, such as routine vision or dental benefits. Medicare Advantage plans vary in the specific benefits they offer, but all are required to offer at least the same amount of coverage as Original Medicare (except for hospice care, which Medicare Part A covers). Some Medicare Advantage plans offer extra coverage, such as routine vision or dental benefits.
A Reason to Be Cautious
Is the new "Medicare and You 2000" handbook enough to help seniors makethe right choice?
Help Beyond HCFA
Archer recommends that people who are considering changing their healthcare option under Medicare seek advice. Every state has a SHIP, or StateHealth Insurance Program, which provides free health insurance counselingon Medicare.
Rising Costs
Even with Medicare and the new managed care options, older Americans arefinding health care expenses rising.
What is Medicare beneficiary?
The Medicare beneficiary when the beneficiary has obtained a settlement, judgment, award or other payment. The liability insurer (including a self-insured entity), no-fault insurer, or workers’ compensation (WC) entity when that insurer or WC entity has ongoing responsibility for medicals (ORM). For ORM, there may be multiple recoveries ...
What is included in a demand letter for Medicare?
The demand letter also includes information on administrative appeal rights. For demands issued directly to beneficiaries, Medicare will take the beneficiary’s reasonable procurement costs (e.g., attorney fees and expenses) into consideration when determining its demand amount.
How long does interest accrue?
Interest accrues from the date of the demand letter, but is only assessed if the debt is not repaid or otherwise resolved within the time period specified in the recovery demand letter. Interest is due and payable for each full 30-day period the debt remains unresolved; payments are applied to interest first and then to the principal. Interest is assessed on unpaid debts even if a debtor is pursuing an appeal or a beneficiary is requesting a waiver of recovery; the only way to avoid the interest assessment is to repay the demanded amount within the specified time frame. If the waiver of recovery or appeal is granted, the debtor will receive a refund.
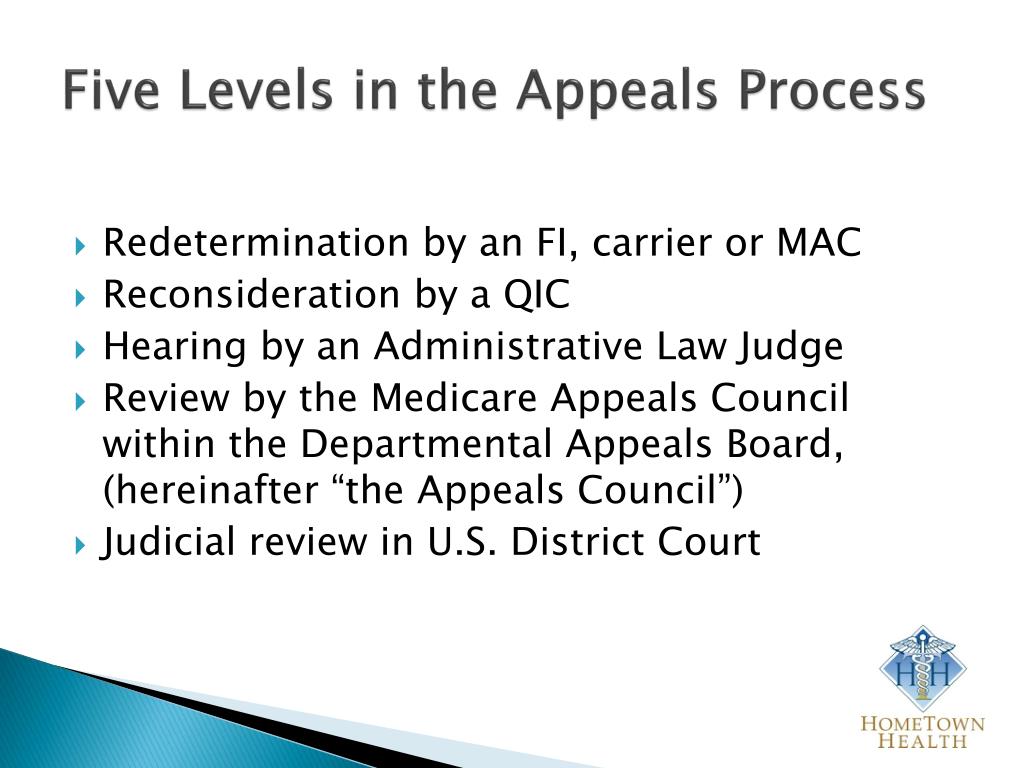
How long does it take to appeal a debt?
The appeal must be filed no later than 120 days from the date the demand letter is received. To file an appeal, send a letter explaining why the amount or existence of the debt is incorrect with applicable supporting documentation.
When can a WC appeal a demand?
Insurer/WC entity debtors may only appeal demands issued on or after April 28, 2015.
Who has the right to appeal a demand letter?
This means that if the demand letter is directed to the beneficiary, the beneficiary has the right to appeal. If the demand letter is directed to the liability insurer, no-fault insurer or WC entity, that entity has the right to appeal.
Can CMS issue more than one demand letter?
For ORM, there may be multiple recoveries to account for the period of ORM, which means that CMS may issue more than one demand letter. When Medicare is notified of a settlement, judgment, award, or other payment, including ORM, the recovery contractor will perform a search of Medicare paid claims history.