Will I be automatically enrolled in Medicare at 65?
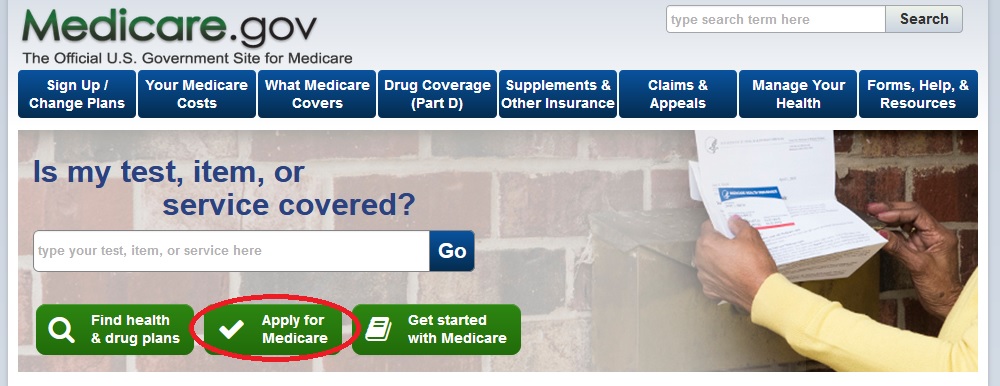
Unless you have already been receiving benefits from Social Security or the Railroad Retirement Board at least four months before you turn 65, you will not be automatically enrolled in Medicare when you turn 65. You will need to sign up for Medicare yourself by applying with Social Security.
How to enroll in Medicare if you are turning 65?
- You have no other health insurance
- You have health insurance that you bought yourself (not provided by an employer)
- You have retiree benefits from a former employer (your own or your spouse’s)
- You have COBRA coverage that extends the insurance you or your spouse received from an employer while working
How does Medicare work when you turn 65?
- Your job-based insurance pays first, and Medicare pays second.
- If you don’t have to pay a premium for Part A, you can choose to sign up when you turn 65 (or anytime later).
- You can wait until you stop working (or lose your health insurance, if that happens first) to sign up for Part B, and you won’t pay a late enrollment penalty.
Is Medicare mandatory when you turn 65?
Technically, it is not mandatory to sign up for Medicare at 65 or at any age, for that matter. But it’s important to consider the situations in which you might decide not to enroll in Medicare at 65 so that you can make sure not to have any lapse in health insurance coverage or face a Medicate late enrollment penalty.
Does Medicare Part A start automatically at age 65?
Yes. If you are receiving benefits, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. (Medicare is operated by the federal Centers for Medicare & Medicaid Services, but Social Security handles enrollment.)
What happens if you don't enroll in Medicare Part A at 65?
The Part A penalty is 10% added to your monthly premium. You generally pay this extra amount for twice the number of years that you were eligible for Part A but not enrolled. For example, suppose that: You were eligible for Medicare in 2020, but you didn't sign up until 2022.
When should I apply for Medicare Part A?
To get Part A (if you have to buy it) and/or Part B the month you turn 65, you must sign up during the first 3 months before the month you turn 65. If you wait until the last 4 months of your Initial Enrollment Period to sign up for Part A (if you have to buy it) and/or Part B, your coverage will be delayed.
Do I have to switch to Medicare when I turn 65?
when you turn 65, you can continue contributing to your HSA. Medicare will not force you to sign up at 65, and you'll get a special enrollment period to sign up later as long as you have a group health plan and work for an employer with 20 or more people.
Can you delay Medicare Part A?
However, if you have to pay a premium for Part A, you can delay Part A until you (or your spouse) stop working or lose that employer coverage. You will NOT pay a penalty for delaying Part A, as long as you enroll within 8 months of losing your coverage or stopping work (whichever happens first).
Can you decline Medicare Part A?
While you can decline Medicare altogether, Part A at the very least is premium-free for most people, and won't cost you anything if you elect not to use it. Declining your Medicare Part A and Part B benefits completely is possible, but you are required to withdraw from all of your monthly benefits to do so.
Is Medicare Part A free?
Most people don't pay a monthly premium for Part A (sometimes called "premium-free Part A"). If you buy Part A, you'll pay up to $499 each month in 2022. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $499.
Do you have to enroll in Medicare Part B every year?
In general, once you're enrolled in Medicare, you don't need to take action to renew your coverage every year. This is true whether you are in Original Medicare, a Medicare Advantage plan, or a Medicare prescription drug plan.
How many months in advance should you apply for Social Security benefits?
four monthsYou can apply up to four months before you want your retirement benefits to start. For example, if you turn 62 on December 2, you can start your benefits as early as December, and apply in August. Even if you are not ready to retire, you still should sign up for Medicare three months before your 65th birthday.
What insurance do you need when you turn 65?
MedicareMedicare: When you turn 65, you are eligible for Medicare, an insurance program operated by the federal government.
What should I do before I turn 65?
11 steps to take if you're turning 65 this yearMake a Social Security plan. ... Get ready for Medicare. ... Medigap or Medicare Advantage? ... Pick the right Medicare Part D plan. ... Consider long-term care insurance. ... Start unlocking new travel deals. ... Get a property tax break. ... Visit the doctor.More items...•
What is included in Medicare Part A?
In general, Part A covers:Inpatient care in a hospital.Skilled nursing facility care.Nursing home care (inpatient care in a skilled nursing facility that's not custodial or long-term care)Hospice care.Home health care.
What happens if you don't sign up for Medicare?
Specifically, if you fail to sign up for Medicare on time, you’ll risk a 10 percent surcharge on your Medicare Part B premiums for each year-long period you go without coverage upon being eligible.
When do you get Medicare if you leave your job?
In that case, you’ll get an eight-month special enrollment period to sign up for Medicare if and when you leave your job or your employer stops offering coverage. It will start the month after you separate from your employer, or the month after your group health coverage ends – whichever happens sooner.
How long does it take to get Medicare?
Learn how to make sure they have health insurance once you’re enrolled. Medicare eligibility starts at age 65. Your initial window to enroll is the seven-month period that begins three months before the month of your 65th birthday and ends three months after it. Seniors are generally advised to sign up on time to avoid penalties ...
How long do you have to sign up for a Part B plan?
Sign up during those eight months, and you won’t have to worry about premium surcharges for being late. And the eight-month special enrollment period is also available if you’re delaying Part B enrollment because you’re covered under your spouse’s employer-sponsored plan, assuming their employer has at least 20 employees.
Do you have to double up on Medicare?
No need to double up on coverage. Many seniors are no longer employed at age 65, and thus rush to sign up for Medicare as soon as they’re able. But if you’re still working at 65, and you have coverage under a group health plan through an employer with 20 employees or more, then you don’t have to enroll in Medicare right now.
Does Medicare pay for Part A?
That said, it often pays to enroll in Medicare Part A on time even if you have health coverage already. It won’t cost you anything, and this way, Medicare can serve as your secondary insurance and potentially pick up the tab for anything your primary insurance (in this case, your work health plan) doesn’t cover.
When do you sign up for Medicare at 65?
When you near your 65th birthday, you will enter what is called your Initial Enrollment Period (IEP). This seven-month period begins three months before you turn 65, includes the month of your birthday and continues for three additional months. This is your first opportunity to sign up for Medicare.
Does Medicare cover health insurance?
Being covered under your employer-provided health insurance plan has no bearing on your Medicare eligibility. Medicare works in conjunction with several other types of health insurance – including health insurance provided by employers or unions – and won’t prevent you from enrolling.
Does Medicare have a late enrollment penalty?
Medicare Part D, which provides coverage for prescription medications, is optional but can also come with a late enrollment penalty if you don’t sign up when you’re supposed to. This penalty is a little more complex to calculate but remains in place for as long as you have Part D coverage. The Part D late enrollment penalty applies if you experience a stretch of at least 63 consecutive days without creditable drug coverage following your IEP and then later enroll in a Part D plan.
Is it mandatory to sign up for Medicare at 65?
Technically, it is not mandatory to sign up for Medicare at 65 or at any age, for that matter. But it’s important to consider the situations in which you might decide not to enroll in Medicare at 65 so that you can make sure not to have any lapse in health insurance coverage or face a Medicate late enrollment penalty.
Do You Have to Sign up For Medicare if You Are Still Working?
The most common reason for people not signing up for Medicare when they turn 65 is because they are still working. Because they’re still working, they’re likely covered under their employer’s health insurance plan and are also unlikely to be collecting Social Security retirement benefits.
When do you need to sign up for Medicare?
If the employer has less than 20 employees: You might need to sign up for Medicare when you turn 65 so you don’t have gaps in your job-based health insurance. Check with the employer.
What happens if you don't sign up for Part A and Part B?
If you don’t sign up for Part A and Part B, your job-based insurance might not cover the costs for services you get.
Do I need to get Medicare drug coverage (Part D)?
You can get Medicare drug coverage once you sign up for either Part A or Part B. You can join a Medicare drug plan or Medicare Advantage Plan with drug coverage anytime while you have job-based health insurance, and up to 2 months after you lose that insurance.
What is a Medicare leave period?
A period of time when you can join or leave a Medicare-approved plan.
Do you have to tell Medicare if you have non-Medicare coverage?
Each year, your plan must tell you if your non-Medicare drug coverage is creditable coverage. Keep this information — you may need it when you’re ready to join a Medicare drug plan.
Does Medicare work if you are still working?
If you (or your spouse) are still working, Medicare works a little differently. Here are some things to know if you’re still working when you turn 65.
Do I need to sign up for Medicare when I turn 65?
It depends on how you get your health insurance now and the number of employees that are in the company where you (or your spouse) work.
What happens if you fail to enroll in Medicare?
If you fail to enroll in Medicare when you become eligible while working for a company that has less than 20 employees, you will incur late enrollment penalties. Medicare is primary when you work for a small company, so you need both Parts A and B.
Is Medicare a secondary plan?
Medicare would be secondary. If you were to have both Medicare and group coverage, your Medicare would supplement your group plan and may reduce some health spending. However, that might only be important to you if you have some health care spending going on and you just want more robust overall coverage.
Can you be penalized for not signing up for Medicare at 65?
Can you be penalized for not signing up for Medicare at 65? Yes, you certainly can if you don’t have creditable employer coverage.
Can you delay Medicare if you retire?
Many people enroll in Part A and delay Parts B and D until they retire. However, you may not want to delay Medicare.
Can you enroll in Medicare if you never enroll?
With that said, if you were to never enroll in Medicare, you wouldn’t end up paying those penalties. However, lasting your entire life without ever needing to sign up for Medicare is unlikely.
Is Medicare primary or secondary?
As we mentioned, when you work for an employer with 20 or more employees, your group health plan is your primary coverage. Medicare would be secondary.
Is Medicare a frustrating process?
Medicare brings up many ifs, ands, and buts. It’s easy to get lost in the chaos of it all. That’s why beginning the Medicare process is so frustrating to most.
How long do you have to work to get Medicare Part A?
If by the time you reach 65 you’ve worked a total of approximately 10 years over your career, you’re entitled to premium-free Medicare Part A, which pays for in-patient hospital charges and more.
What happens if you overlook Medicare enrollment rules?
Medicare processes and rules are complex and rife with exceptions; if you overlook something in the enrollment rules, you may pay a high price in terms of both penalties and gaps in coverage. So you should consult with Medicare and with the benefits administrator for your employer coverage — before you enroll or decide to delay enrollment.
How many employees do you have to have to have Medicare Part B?
If the employer has fewer than 20 employees: If your or your spouse's employer has fewer than 20 employees and the health coverage is not part of a multiemployer group plan, at age 65 you must enroll in Medicare Part B, which will be your primary insurance. If you have an HSA and want to keep contributing: If you have an HSA ...
What is Medicare Part A?
If the employer has fewer than 20 employees: If your or your spouse's employer has fewer than 20 employees and the health coverage is not part of a multiemployer group plan, at age 65 you must enroll in Medicare Part A, which will be your primary insurance. “Primary” means that Medicare pays first, and then the employer insurance kicks in ...
How long do you have to keep HSA contributions?
Stop making contributions to your HSA at least six months before you sign up for Part B. And you’ll want to sign up for Medicare at least a month before you stop work ...
Does Medicare Part A cover my employer?
Because in some cases, Medicare Part A may cover what your employer plan does not. But as with so many aspects of Medicare, there are caveats, exceptions and potential pitfalls. If the employer has 20 or more employees: If your or your spouse's employer has 20 or more employees and a group health plan, you don't have to sign up for Medicare ...
Is Medicare cheaper than group health insurance?
If your employer (or your spouse’s employer) requires you to pay a large portion of the premium on your group health insurance, you may find Medicare cheaper and the coverage adequate. So compare your current coverage and out-of-pocket expenses — including premiums, deductibles, copays and coinsurance — with your costs and benefits under Medicare, which may also pay some expenses not covered by your group plan.
What is the Medicare rate for 2021?
The base rate in 2021 is $148.50 a month. Higher-income individuals pay more depending on the amount of income. You can opt out of Part B — for example, if you already have what Medicare calls “primary coverage” through an employer, spouse or veterans’ benefits and you want to keep it.
Does Social Security automatically sign you up for Medicare?
AARP | Comments: 8. En español | Yes. If you are receiving Social Security, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. (Medicare is operated by the federal Centers for Medicare & Medicaid Services, but Social Security handles enrollment.) Social Security will send you sign-up ...
Does Medicare cover home health?
Medicare Part A covers basic hospital visits and services and some home health care, hospice and skilled-nursing services. If you are receiving or are eligible to receive Social Security retirement benefits, you do not pay premiums for Part A.
What happens if you don't sign up for Medicare?
Therefore, if you fail to sign up for Medicare when required, you will essentially be left with no coverage. It’s therefore extremely important to ask the employer whether you are required to sign up for Medicare when you turn 65 or receive Medicare on the basis of disability.
How many employees do you need to be to receive Medicare?
The law requires a large employer — one with at least 20 employees — to offer you (and your spouse) the same benefits that it offers to younger employees (and their spouses). It is entirely your choice (not the employer’s) whether to: accept the employer health plan and delay Medicare enrollment.
How long can you delay Medicare?
As long as you have group health insurance from an employer for which you or your spouse actively works after you turn 65, you can delay enrolling in Medicare until the employment ends or the coverage stops (whichever happens first), without incurring any late penalties if you enroll later. When the employer-tied coverage ends, you’re entitled to a special enrollment period of up to eight months to sign up for Medicare.
Is Medicare Part B primary or group?
If you enroll in both the group plan and Medicare Part B, be aware of the consequences. In this situation, the employer plan is always primary, meaning that it settles medical bills first and Medicare only pays for services that it covers but the employer plan doesn’t.
Can you delay Medicare enrollment?
You can’t delay Medicare enrollment without penalty if your employer-sponsored coverage comes from retiree benefits or COBRA — by definition, these do not count as active employment. Nor does it count if you work beyond 65 but rely on retiree benefits from a former employer.
Can you sell a Medigap policy?
Insurance companies are prohibited from refusing to sell you a Medigap policy or charge higher premiums based on your health or preexisting medical conditions, if you buy the policy within six months of enrolling in Part B. Outside of that six-month window, except in very limited circumstances, they can do both.