What other benefits can I collect while on SSDI?
Medicare coverage kicks in for most SSDI recipients two years after the first month they are eligible for their monthly disability benefits. However, this doesn’t automatically mean that every person approved for SSDI must wait two years to get their Medicare coverage. The two-year Medicare waiting period generally gets calculated from the date of your SSDI entitlement (the …
What is the waiting period for Medicare disability?
Jul 16, 2020 · However, Medicare isn’t limited to only those 65 and up—Americans of any age are eligible for Medicare if they have a qualifying disability. Most people are automatically enrolled in Medicare Part A and Part B once they’ve been collecting Social Security Disability Insurance (SSDI) payments for 24 months.
What are the top 10 conditions that qualify for disability?
Nov 12, 2020 · Once a disability beneficiary is at least 20 years old and has been declared disabled for 24 continuous months, they can qualify for Medicare. Only a child diagnosed with End-Stage Renal Disease (ESRD) will qualify for Medicare before turning 20 years old. Primary Disability Categories and Requirements
Does Someone on Social Security disability get free Medicare?
Medicare eligibility after disability usually doesn’t start right away. The date your Medicare coverage will start depends on your disability. For most qualifying disabilities, you’ll need to wait for two years to receive Medicare benefits. Your Medicare coverage begins after you’ve received SSDI for 24 months. If you have Lou Gehrig’s Disease, also known as ALS, you’ll get coverage …

What Disabilities Qualify Someone for Medicare Coverage?
If you have a disability, the costs of healthcare can add up quickly, especially if you’re no longer working. That’s why Medicare provides healthca...
When Does Coverage Begin?
Medicare eligibility after disability usually doesn’t start right away. The date your Medicare coverage will start depends on your disability.
How do People with Disabilities Enroll in Medicare?
If you’re under 65 and receiving Social Security disability benefits, enrolling in Medicare is easy. In most cases, you won’t need to do anything....
When will Medicare be available for seniors?
July 16, 2020. Medicare is the government health insurance program for older adults. However, Medicare isn’t limited to only those 65 and up—Americans of any age are eligible for Medicare if they have a qualifying disability. Most people are automatically enrolled in Medicare Part A and Part B once they’ve been collecting Social Security Disability ...
What conditions are considered to be eligible for Medicare?
Even though most people on Social Security Disability Insurance must wait for Medicare coverage to begin, two conditions might ensure immediate eligibility: end-stage renal disease (ESRD) and Lou Gehrig’s disease (ALS).
What is ESRD in Medicare?
ESRD, also known as permanent kidney failure, is a disease in which the kidneys no longer work. Typically, people with ESRD need regular dialysis or a kidney transplant (or both) to survive. Because of this immediate need, Medicare waives the waiting period. 2
What to do if your income is too high for medicaid?
If your income is too high to qualify for Medicaid, try a Medicare Savings Program (MSP), which generally has higher limits for income. As a bonus, if you qualify for an MSP, you automatically qualify for Extra Help, which subsidizes your Part D costs. Contact your state’s Medicaid office for more information.
How long does it take to get Medicare if you appeal a decision?
The result: your wait for Medicare will be shorter than two years.
How long does a disability last?
The government has a strict definition of disability. For instance, the disability must be expected to last at least one year. Your work history will also be considered—usually, you must have worked for about 10 years but possibly less depending on your age.
Does Medicare cover ALS?
Medicare doesn’t require a waiting period for people diagnosed with ALS, but they need to qualify based on their own or their spouse’s work record. 3
How long does a child have to be disabled to qualify for Medicare?
Disability benefits through SSA can be granted at any age. Once a disability beneficiary is at least 20 years old and has been declared disabled for 24 continuous months, they can qualify for Medicare. Only a child diagnosed with End-Stage Renal Disease (ESRD) ...
How old do you have to be to qualify for Medicare?
If you're age 65 or older, you will typically qualify for Medicare automatically. But you can also qualify for Medicare if you have a disability as determined by the Social Security Administration (SSA) if you're at least 20 years old.
What are the different types of disability?
The SSA determines disability eligibility through the examination of medical records, expert consults and a claimant's self-report of activity limitations. The scope and severity of health issues that lead to disability determinations are different for each individual. The SSA categorizes disabilities into the following groups : 1 Sensory and speech disorders 2 Musculoskeletal conditions 3 Cardiovascular and respiratory illnesses 4 Neurological disorders 5 Cancer and immune system disorders 6 Mental health conditions 7 Congenital disorders 8 Endocrine and digestive conditions 9 Skin disorders
How long can you be on Medicare if you have both SSI and SSDI?
Regardless of which disability benefit you receive, you will not become eligible for Medicare until you've been disabled for 24 months.
How does the SSA determine disability eligibility?
The SSA determines disability eligibility through the examination of medical records, expert consults and a claimant's self-report of activity limitations. The scope and severity of health issues that lead to disability determinations are different for each individual.
What is the difference between SSDI and SSI?
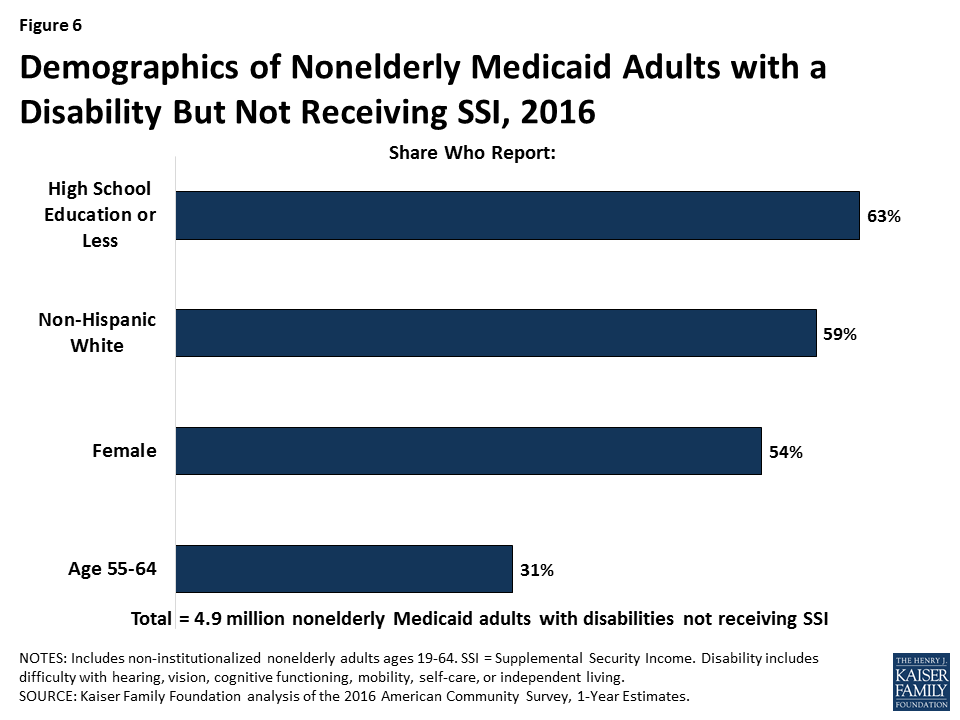
Types of Social Security Disability Benefits: SSI vs. SSDI. Most people are awarded either Supplemental Security Income (SSI) or Social Security Disability Insurance (SSDI) benefits. SSI is based on financial need, and SSDI is awarded if you have a minimum work history. Individuals with SSI may qualify for Medicaid in their home state.
Can I get Medicare Advantage if I have dual eligibility?
Depending on your financial need, you may qualify for Medicare and Medicaid, which is commonly called dual eligible. Medicare Advantage plans are available in a variety of plan types for people who are dual-eligible, in long-term care facilities or have chronic special needs.
How long do you have to wait to get Medicare if you have Social Security Disability?
Social Security Disability Insurance (SSDI) & Medicare coverage. If you get Social Security Disability Income (SSDI), you probably have Medicare or are in a 24-month waiting period before it starts. You have options in either case.
What is SSI disability?
Supplemental Security Income (SSI) Disability & Medicaid coverage. Waiting for a disability status decision and don’t have health insurance. No disability benefits, no health coverage. The Marketplace application and disabilities. More information about health care for people with disabilities.
Can I enroll in a Medicare Marketplace plan if I have Social Security Disability?
You’re considered covered under the health care law and don’t have to pay the penalty that people without coverage must pay. You can’t enroll in a Marketplace plan to replace or supplement your Medicare coverage.
Can I keep my Medicare Marketplace plan?
One exception: If you enrolled in a Marketplace plan before getting Medicare, you can keep your Marketplace plan as supplemental insurance when you enroll in Medicare. But if you do this, you’ll lose any premium tax credits and other savings for your Marketplace plan. Learn about other Medicare supplement options.
Can I get medicaid if I have SSDI?
You may be able to get Medicaid coverage while you wait. You can apply 2 ways: Create an account or log in to complete an application. Answer “ yes” when asked if you have a disability.
Can I get medicaid if I'm turned down?
If you’re turned down for Medicaid, you may be able to enroll in a private health plan through the Marketplace while waiting for your Medicare coverage to start.
How long is a person eligible for Medicare?
Everyone eligible for Social Security Disability Insurance (SSDI) benefits is also eligible for Medicare after a 24-month qualifying period. The first 24 months of disability benefit entitlement is the waiting period for Medicare coverage. During this qualifying period for Medicare, the beneficiary may be eligible for health insurance ...
How long can you keep Medicare after you return to work?
Answer: As long as your disabling condition still meets our rules, you can keep your Medicare coverage for at least 8 ½ years after you return to work. (The 8 ½ years includes your nine month trial work period.) Question: I have Medicare hospital Insurance (Part A) and medical insurance (Part B) coverage.
Why does Bill have Medicare?
Example: Bill has Medicare coverage because of permanent kidney failure. He also has group health plan coverage through the company he works for. His group health coverage will be his primary payer for the first 30 months after Bill becomes eligible for Medicare. After 30 months, Medicare becomes the primary payer.
How to order a publication from Medicare?
Answer: You can view, print, or order publications online or by calling 1-800-MEDICARE (1-800-633-4227). The fastest way to get a publication is to use our search tool and then view and print it. If you order online or through 1-800-MEDICARE, you will receive your order within 3 weeks. The link to search publications is at: http://www.medicare.gov/Publications/home.asp
Is Medicare a secondary payer?
Answer: Medicare may be the "secondary payer" when you have health care coverage through your work. See the information under "Coordination of Medicare and Other Coverage for Working Beneficiaries with Disabilities" about when Medicare is a "secondary payer or primary payer".
Does Medicare pay for non-VA hospital?
If the VA authorizes services in a non-VA hospital, but doesn't pay for all of the services you get during your hospital stay, then Medicare may pay for the Medicare-covered part of the services that the VA does not pay for. Example: John, a veteran, goes to a non-VA hospital for a service that is authorized by the VA.
Does Medicare pay for the same service?
Medicare cannot pay for the same service that was covered by Veterans benefits, and your Veterans benefits cannot pay for the same service that was covered by Medicare. You do not have to go to a Department of Veterans Affairs (VA) hospital or to a doctor who works with the VA for Medicare to pay for the service.
How long do you have to be on Medicare for SSDI?
Default Rules on Medicare for SSDI Recipients: The basic regulations provide that you become eligible for Medicare coverage two years after your date of entitlement for purposes of SSDI; this is the date that you first start receiving your SSDI benefits.
How long do you have to wait to get Medicare if you have ALS?
You may not have to wait two years if you suffer from: End-stage renal disease (ESRD) with kidney failure, which makes you eligible shortly after you begin dialysis; or, Amyotrophic lateral sclerosis (ALS), where you could qualify for Medicare at the same time you start receiving SSDI payments.
How long can you get retroactive SSDI?
Another consideration is that SSA only allows retroactive SSDI benefits for a maximum of 12 months, which impacts your disability onset date – and therefore your Medicare eligible as well.
Does Medicare start immediately after SSDI?
However, in most cases, your Medicare coverage will not start immediately once you are approved for SSDI benefits. There is a waiting period, which a Maryland Social Security disability lawyer can explain in more detail based upon your unique situation. As an overview, you should note:
Can you get Medicaid if you have assets?
Being a needs-based program, you can only receive benefits if your income and assets are below a maximum threshold. If you do meet the requirements for Medicaid, you might also qualify for SSA’s other disability program: Supplemental Security Income (SSI).
Is Medicare for older people?
Medicare is the US health insurance system for people aged 65 years or older, but certain benefits may also be available for younger individuals who suffer from disabilities. Social Security Administration (SSA) rules provide that recipients of Social Security Disability Insurance (SSDI) may be eligible to receive Medicare benefits under Part A, ...
When do you get Medicare cards?
You'll get Medicare cards in the mail three months before your 25th month of disability.
How long does it take to get approved for SSDI?
However, getting approved for SSDI can be a long process, and even after you're approved, you'll have to wait 24 months before your Medicare benefits begin (with exceptions for end-stage renal disease and amyotrophic lateral sclerosis).
How to apply for SSDI?
Your application for SSDI is likely to move more quickly if you select one doctor as the lead contact for your case. It's best to go with one who: 1 Has experience with disability cases 2 Responds promptly to requests for information 3 Is familiar with your overall health situation
How long does Medicare cover ESRD?
If you have employer-sponsored or union-sponsored insurance and you become eligible for Medicare due to ESRD, Medicare will coordinate with your existing coverage for 30 months. During that time, your private insurance will be your primary coverage, and Medicare will pick up a portion of the remaining costs.
What happens if you don't want Medicare Part B?
If you don't want Medicare Part B, you can send back the card. If you keep the card, you'll keep Part B and will pay Part B premiums. In 2021, the Part B premium is $148.50 per month for most enrollees. 6 . You'll also be eligible to join a Medicare Part D prescription drug plan.
How long does it take for SSDI to start?
According to the law, your SSDI payments cannot start until you have been disabled for at least five full months. 4 Your payment will usually start with your sixth month of disability.
How many people are covered by Medicare?
Medicare provides coverage for about 10 million disabled Americans under the age of 65 . Medicare isn't available to most people until age 65, but if you have a long-term disability or have been diagnosed with certain diseases, Medicare is available at any age.
How long do you have to wait to get Medicare?
You have to wait two years after you are entitled to disability benefits to get Medicare unless you fit into an exception. All Social Security disability insurance (SSDI) recipients can receive Medicare coverage two years after the first month they are eligible for their monthly disability benefits. This does not mean that every individual who is ...
How long is the waiting period for Medicare?
In general, the two-year waiting period for Medicare is calculated from your date of SSDI entitlement—when you are eligible to start receiving monthly benefits. This is usually the date your disability began, plus five months (due to the five-month waiting period for SSDI).
How long does it take for Medicare to start?
On the other hand, for disability applicants who apply for benefits only when they become disabled, and not before, the date that their Medicare coverage will start is more likely to be two years and five months after they apply for disability.
When will Makayla get her SSDI?
Makayla applies for disability on August 1, 2019, the day after she quit work due to her disability. Thirteen months later, on September 1, 2020, she is approved for SSDI benefits with a disability onset date of August 1, 2019. She is eligible for retroactive benefits only going back to January 1, 2020, five months after her disability onset date. Because her date of entitlement is January 1, 2020, she'll be eligible for Medicare on January 1, 2022. Note that her eligibility for Medicare starts two years and five months after her application date.
When will Isaiah be eligible for Medicare?
But he is eligible for retroactive benefits only going back to October 1, 2018, five months after his disability onset date. Because his date of entitlement is October 1, 2018, he'll be eligible for Medicare on October 1, 2020. Note that his eligibility for Medicare starts only 14 months after his application date, and only one month after his decision date.
When does Medicare cover end stage renal disease?
If you require ongoing dialysis or a kidney transplant, Medicare coverage can begin the third month after the month in which your dial ysis began. Amyotrophic lateral sclerosis (ALS). Individuals with amyotrophic lateral sclerosis (ALS) qualify for Medicare as soon as they are eligible ...
Can I get medicaid with low income?
Those with low income and low assets may qualify for the Medicaid program during the two-year waiting period for Medicare. States set their own rules regarding Medicaid eligibility, but those granted SSI at the same time as SSDI automatically qualify for Medicaid.