
When should you sign up for Medicare Part B?
Disabled individuals are automatically enrolled in Medicare Part A and Part B after they have received disability benefits from Social Security for 24 months. NOTE: In most cases, if someone does not enroll in Part B or premium Part A when first eligible, they will have to pay a late enrollment penalty. The Part B penalty is assessed for as long as the person has Part B.
What is the maximum premium for Medicare Part B?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance). You are eligible for premium-free Part A if you are age 65 or older and you or your spouse worked and …
When can I sign up for Part B Medicare?
Some of these retiree plans offer a Part B reimbursement to eligible enrollees. Each retiree plan has different eligibility requirements, so check with your plan to understand your options. However, for most plans you must be a retired employee or already enrolled in the health plan and be enrolled in Medicare Part B.
When do I have to enroll in Medicare Part B?
Dec 08, 2021 · Medicare Part B is a health insurance option that becomes available for people in the United States once they reach age 65. However, there are some special circumstances under which you may qualify to enroll in Medicare Part B before the age of 65. Below, you will find the eligibility requirements for enrolling in Medicare Part B.
Does everyone automatically get Medicare Part B?
Medicare will enroll you in Part B automatically. Your Medicare card will be mailed to you about 3 months before your 65th birthday. If you're not getting disability benefits and Medicare when you turn 65, you'll need to call or visit your local Social Security office, or call Social Security at 1-800-772-1213.
What are requirements for Medicare Part B?
You're 65 years old You automatically qualify for Medicare Part B once you turn 65 years old. Although you'll need to wait to use your benefits until your 65th birthday, you can enroll: 3 months before your 65th birthday. on your 65th birthday.
Can I get Medicare Part B at 62?
You may apply for Medicare at any age if you meet one of the following criteria: your receive Social Security disability or Railroad Retirement Board (RRB) disability insurance. you have specific medical conditions, such as amyotrophic lateral sclerosis (ALS) or end stage renal disease (ESRD)
How soon before I retire should I apply for Medicare Part B?
You should start your Part B coverage as soon as you stop working or lose your current employer coverage (even if you sign up for COBRA or retiree health coverage from your employer). You have 8 months to enroll in Medicare once you stop working OR your employer coverage ends (whichever happens first).
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.Jan 3, 2022
How do you pay for Medicare Part B if you are not collecting Social Security?
You can request to have your Part B premiums deducted from your Office of Personnel Management (OPM) annuity as long as you're NOT entitled to Social Security or RRB benefits. Call us at 1-800-MEDICARE to make your request. For questions about your bill, call the RRB at 1-877-772-5772.
Can I draw Social Security at 62 and still work full time?
You can get Social Security retirement or survivors benefits and work at the same time. But, if you're younger than full retirement age, and earn more than certain amounts, your benefits will be reduced. The amount that your benefits are reduced, however, isn't truly lost.
Is Medicare Part A free at age 65?
Most people age 65 or older are eligible for free Medical hospital insurance (Part A) if they have worked and paid Medicare taxes long enough. You can enroll in Medicare medical insurance (Part B) by paying a monthly premium. Some beneficiaries with higher incomes will pay a higher monthly Part B premium.
Does Medicare coverage start the month you turn 65?
For most people, Medicare coverage starts the first day of the month you turn 65. Some people delay enrollment and remain on an employer plan. Others may take premium-free Part A and delay Part B. If someone is on Social Security Disability for 24 months, they qualify for Medicare.
Do you pay Medicare when you retire?
Do you have to pay for Medicare when you retire? Medicare programs can help cover your healthcare needs during your retirement years. It is automatically offered when you turn age 65. While Medicare isn't necessarily mandatory, it may take some effort to opt out of.
For those who qualify, there are multiple ways to have your Medicare Part B premium paid
In 2022, the standard Medicare Part B monthly premium is $170.10. Beneficiaries also have a $233 deductible, and once they meet the deductible, must typically pay 20% of the Medicare-approved amount for any medical services and supplies.
What is the Part B premium reduction benefit?
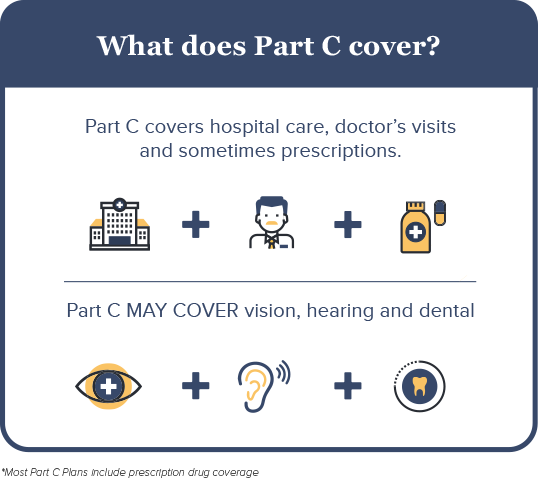
The giveback benefit, or Part B premium reduction, is when a Part C Medicare Advantage (MA) plan reduces the amount you pay toward your Part B monthly premium. Your reimbursement amount could range from less than $1 to the full premium amount, which is $170.10 in 2022.
How to find plans that offer the giveback benefit
Not all MA plans offer this benefit, so you must find a plan that does in order to take advantage of the opportunity. In 2022, these plans are offered in nearly all states, so you may find one close to you.
Other Part B reimbursement options
There are other ways you can lower or eliminate how much you pay for the Medicare Part B premium. This includes certain Medicaid programs or benefits from some retiree health plans.
What Happens When You Turn 65
If you already receive benefits from Social Security or the Railroad Retirement Board , youll be automatically enrolled in traditional Medicare, aka Original Medicare. This consists of Part A hospital insurance and Part B medical insurance. Your Medicare coverage usually starts the first day of the month you turn 65.
Is Medicare Ever Free
By and large, Medicare is not considered free. Because you have been contributing to your Medicare services through taxes throughout your life, you will have contributed money to Medicare regardless of the current cost of your copayments or premiums.
Medicare Savings Programs: How It Works
Those with limited income and resources may qualify for premium assistance through Medicare Savings Programs . Each state manages MSP funds and decides who qualifies. Programs can pay for all, or just some, of your Medicare out-of-pocket expenses, which includes premiums.
Help Paying Original Medicare Premiums
Most MSPs provide help for Medicare Part A or Part B only. All programs require eligibility for Medicare Part A, but the main difference between each is the federal poverty level range that those seeking help must be within.
How Long Can You Stay In A Nursing Home With Medicare
Medicare covers up to 100 days of care in a skilled nursing facility each benefit period. If you need more than 100 days of SNF care in a benefit period, you will need to pay out of pocket. If your care is ending because you are running out of days, the facility is not required to provide written notice.
How Much Does Medicare Cost On Disability
If you qualify for SSDI, you’ll typically qualify for premium-free Medicare Part A based on your work record. Part B requires a monthly premium , automatically deducted from your Social Security check. You can technically opt out of Part B if you dont want to pay the premiums. Just know that without Part B, youll forego extensive medical coverage.
How To Find Plans That Offer The Giveback Benefit
Not all MA plans offer this benefit, so you must find a plan that does in order to take advantage of the opportunity. In 2021, these plans are offered in nearly all states, so you may find one close to you.
What is a SEP for Medicare?
What is the Medicare Part B Special Enrollment Period (SEP)? The Medicare Part B SEP allows you to delay taking Part B if you have coverage through your own or a spouse’s current job. You usually have 8 months from when employment ends to enroll in Part B. Coverage that isn’t through a current job – such as COBRA benefits, ...
What is a Part B SEP?
The Part B SEP allows beneficiaries to delay enrollment if they have health coverage through their own or a spouse’s current employer. SEP eligibility depends on three factors. Beneficiaries must submit two forms to get approval for the SEP. Coverage an employer helps you buy on your own won’t qualify you for this SEP.
How long can you delay Part B?
You can delay your Part B effective date up to three months if you enroll while you still have employer-sponsored coverage or within one month after that coverage ends. Otherwise, your Part B coverage will begin the month after you enroll.
What to do if your Social Security enrollment is denied?
If your enrollment request is denied, you’ll have the chance to appeal.
When do you have to take Part B?
You have to take Part B once your or your spouse’s employment ends. Medicare becomes your primary insurer once you stop working, even if you’re still covered by the employer-based plan or COBRA. If you don’t enroll in Part B, your insurer will “claw back” the amount it paid for your care when it finds out.
Who is Josh Schultz?
Josh Schultz has a strong background in Medicare and the Affordable Care Act. He coordinated a Medicare ombudsman contract at the Medicare Rights Center in New York City, and represented clients in extensive Medicare claims and appeals.
How much does Medicare pay for outpatients?
Your healthcare providers will bill Medicare, and Part B will then pay 80% of your outpatient expenses after your small deductible. Medicare then sends the remainder of that bill to your Medigap plan to pay the other 20%. The same goes for Medicare Advantage plans.
How long do you have to enroll in Part B if you retire?
When you retire and lose your employer coverage, you’ll be given a 8-month Special Enrollment Period to enroll in Part B without any late penalty.
How much is Part B insurance?
Most people delay Part B in this scenario. Your employer plan likely already provides good outpatient coverage. Part B costs at least $148.50/month for new enrollees in 2020.
What happens if you opt out of Part B?
Be aware that if you opt out of Part B and then later decide to join, you will pay a Part B late penalty. You’ll also need to wait until the next General Enrollment Period to enroll, which means there could be a delay before your coverage becomes active. In my opinion, most Veterans should sign up for Part B.
Do you need Part B before you can enroll in Medigap?
Conclusion. To recap the important points in this article, most people need Part B at some point. When you enroll will depend on what other coverage you currently have when you turn 65. Also, Part B is not a supplement. You need Part B before you can enroll in Medigap or a Medicare Advantage plan.
Does Medigap replace Part B?
Medigap plans do not replace Part B. They pay secondary to Part B. Part B works together with your Medigap plan to provide you full coverage. This means you must be enrolled in Part B before you are even eligible to apply for a Medicare supplement.
Do you have to be enrolled in Part B for Medicaid?
When you are 65 or older and enrolled in Medicaid. All of these scenarios require you to be enrolled in Part B. Without it, you would be responsible for the first 80% of all outpatient charges. Even worse, your secondary coverage may not pay at all if you are not actively enrolled in Part B as your primary coverage.
What Is The Medicare Part B Give Back Benefit?
The Give Back benefit is a benefit offered by some Medicare Advantage plan carriers that can help you reduce your Medicare Part B premium. You should know, however, that the Give Back benefit is not an official Medicare program. This benefit is provided as part of some Medicare Part C plans as a way to encourage participation in a specific plan.
Who Is Eligible For The Medicare Part B Give Back Benefit?
It is pretty easy to qualify for the Medicare Give Back benefit as the eligibility criteria are straightforward. First, you must be enrolled in Original Medicare. You need to have both Medicare Part A and Medicare Part B coverage. Next, you must pay your own monthly Part B premium.
Applying For A Medicare Part B Give Back Benefit
So, what is the enrollment process for the Give Back benefit? Many people are looking to save as much money as possible when it comes to their health care costs, so they want to know how to get signed up for this program. The process is quite simple, so here is how to do it.
The Bottom Line
Since most people on Medicare are receiving Social Security benefits, finding a way to reduce the cost of your health insurance is always a plus. The Medicare Give Back program can do just that by paying for a portion or even all of your Medicare Part B premium.
What is the deadline for Medicare give back benefit?
There is no deadline to qualify for the give back benefit. You must already be enrolled in Medicare Part A and Part B, and you must pay your own monthly Part B premium. You then simply need to enroll in a Medicare Advantage plan that offers this benefit.
What are the three cost reduction programs for Medicare Part B?
The three cost reduction programs are the Qualified Medicare Beneficiary (QMB), the Specified Low-Income Medicare Beneficiary (SLMB), and Qualifying Individual (QI)
What is a qualified Medicare beneficiary?
Qualified Medicare Beneficiary. The first program that can help reduce your costs is the Qualified Medicare Beneficiary (QMB). There are two requirements to be eligible for this program, which include the income limit and asset limit. If you meet both of these requirements and are eligible for the program, your state should pay your premiums, ...
What is the asset limit for QMB?
In addition to the income limit, there is an asset limit you must meet in order to be eligible for the QMB program. The asset limit is approximately $7000 for an individual and $11,000 for a couple that is married.
How much was Medicare Part B premium in 2015?
The standard Part B premium for 2015 was $121.80, although it can be higher based on your income or other factors. Although most people have to pay a premium to be eligible to receive Medicare Part B benefits, there are programs that can help reduce or cover the cost depending on your circumstances. Enter your zip code above to receive private ...
How much does Medicare Part B cost?
The standard premium amount for Medicare Part B is $144.60. You may pay a higher premium amount if your income is higher than $85,000 as an individual and $170,000 as a couple.
What is the minimum income for a married couple in 2020?
Your income must be no more than the federal poverty level to be eligible for this program, which was an annual income of $12,760 for a single person and an annual income of $17,240 for a married couple in 2020.
