One way to do this is by having all new Medicare patients sign an ABN form when they come into the clinic for the first time. If they’re coming to the clinic later on, make sure that they sign the ABN form at least once a year.
Should My Medicare patients sign an ABN?
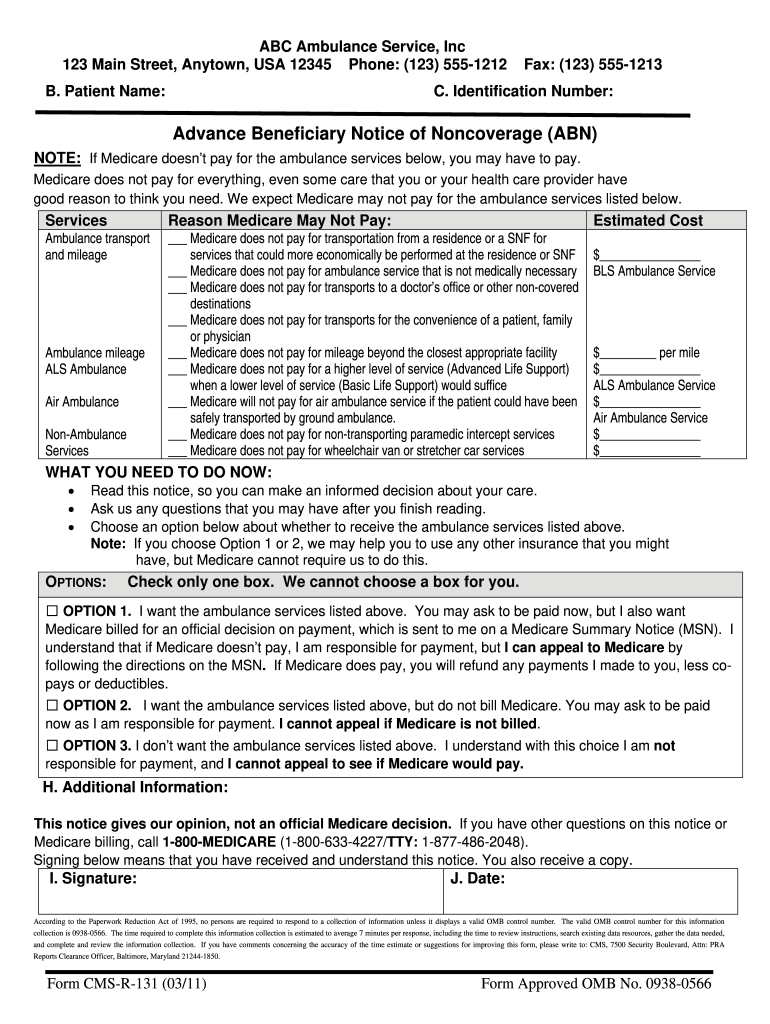
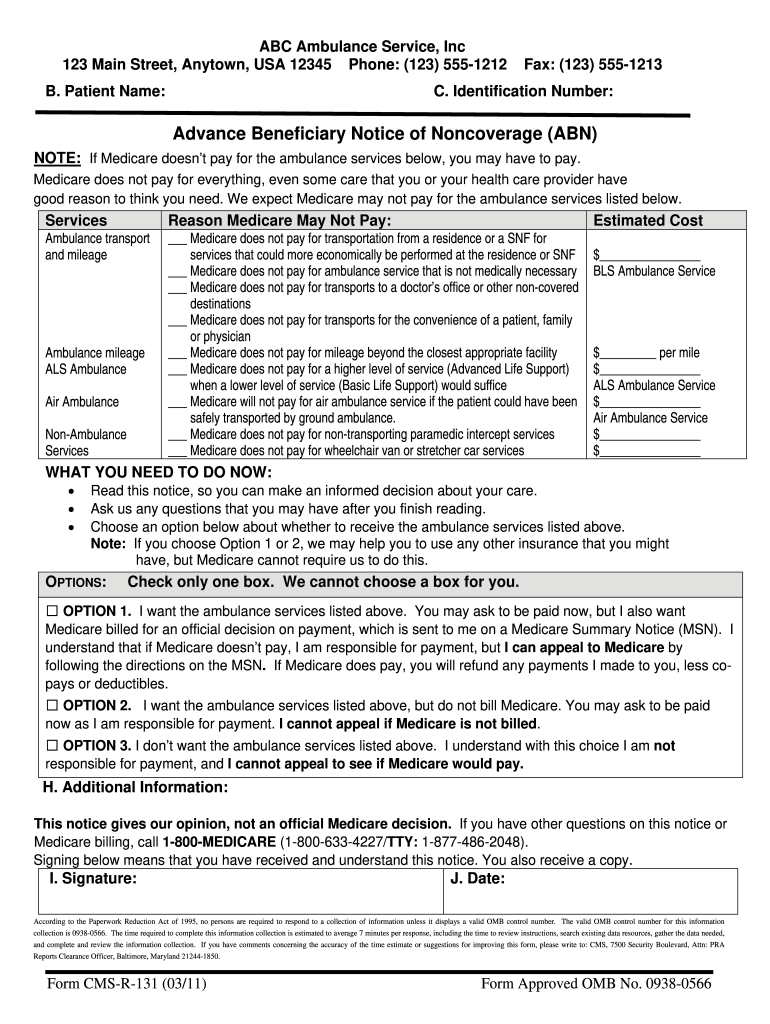
An ABN is a written notice from Medicare (standard government form CMS-R-131), given to you before receiving certain items or services, notifying you: Medicare may deny payment for that specific procedure or treatment. You will be personally responsible for full payment if Medicare denies payment.
What is an ABN in medical billing?
Sep 25, 2017 · When should I use an ABN? Medicare requires that an ABN be used in the following circumstances: You have a reasonable belief that Medicare may not pay for an item or service that is normally a covered service. In addition, the reason for denial is because it is not medically reasonable and necessary
Should My Medicare patients sign an advance beneficiary notice?
Jul 12, 2010 · When applicable, your Medicare patients should always sign an Advance Beneficiary Notice (form CMS-R-131). An ABN is not used for commercial insurance companies. What Is An ABN? An ABN is a Medicare waiver of liability that providers are required to give a Medicare patient for services provided that may not be covered or considered
What is an advance beneficiary notice (ABN)?
An ABN is valid if a patient understands what the notice means. An exception applies when patients have no financial liability to a non-contract supplier of an item from the Competitive Bidding Program unless they sign an ABN indicating Medicare won’t pay for the item because

When should a patient sign an ABN?
The ABN must be completed and signed by the patient BEFORE you provide services or items that are not covered by insurance. Do not continue with the procedure until the patient signs an ABN and accepts financial responsibility for non-covered services. Always file the signed ABN in the patient's medical records.Aug 3, 2020
Why would a patient sign an Advanced beneficiary Notice?
The Advance Beneficiary Notice helps patients decide whether to get the item or service Medicare may not cover and accept financial responsibility. If you don't provide the patient with required written notices, Medicare may hold you financially liable if they deny payment.
What is an ABN form and who needs one?
An ABN is a written notice from Medicare (standard government form CMS-R-131), given to you before receiving certain items or services, notifying you: Medicare may deny payment for that specific procedure or treatment. You will be personally responsible for full payment if Medicare denies payment.
When should an ABN not be issued?
If the provider does not have a reasonable belief that the service or item that is normally payable will be denied than an ABN is prohibited from being issued. Other circumstances were you are prohibited from issuing an ABN include: To make a beneficiary liable for Medically Unlikely Edit (MUE) denials.Sep 25, 2017
Do Medicare patients have to sign an ABN?
Does Your Medicare Patient Need To Sign An Advance Beneficiary Notice (ABN) CMS-R-131? Yes! When applicable, your Medicare patients should always sign an Advance Beneficiary Notice (form CMS-R-131). An ABN is not used for commercial insurance companies.
Does Medicare require an ABN?
You must issue an ABN: When a Medicare item or service isn't reasonable and necessary under Program standards, including care that's: Not indicated for the diagnosis, treatment of illness, injury, or to improve the functioning of a malformed body member.
Is an ABN required when Medicare is secondary?
ABN s are not required for care that is statutorily excluded or for services that are never a Medicare benefit; however, CMS does strongly encourage provider/suppliers to provide an ABN for care that they believe may not be covered to the beneficiary as a courtesy to advise of pending financial obligation.Oct 11, 2021
Is ABN for Medicare Part A or B?
Therefore, an ABN is used for services rendered to Original Medicare FFS (Part A and Part B) enrollees. That means an ABN is not required for Medicare Part C and Part D. When the services are not covered, then patient is responsible for UMDAP amount or cost of services, whichever is less.
Is an ABN required if Medicare is secondary?
The ABN needs to be on file for the year that the patient is responsible for paying. If the patient fits Medicare's guidelines for “high risk” they are allowed to have the pap every 12 months and no ABN is required.Nov 19, 2009
Which providers are likely to use an ABN form?
The Advance Beneficiary Notice of Noncoverage (ABN), Form CMS-R-131, is issued by providers (including independent laboratories, home health agencies, and hospices), physicians, practitioners, and suppliers to Original Medicare (fee for service - FFS) beneficiaries in situations where Medicare payment is expected to be ...Dec 1, 2021
Does Your Medicare Patient Need to Sign An Advance Beneficiary Notice (ABN) Cms-R-131?
Yes! When applicable, your Medicare patients should always sign an Advance Beneficiary Notice (form CMS-R-131). An ABN is not used for commercial i...
Abns Also Protect Your Patient
An ABN notifies Medicare that the patient acknowledges that certain procedures were provided. 1. It also gives the patient the opportunity to accep...
Modifiers Required When Billing With An ABN
Any procedures provided that require an ABN must be submitted with one of the following Medicare modifiers: 1. GA Modifier: Waiver of Liability Sta...
What is an ABN in Medicare?
Most of us are familiar with the term ABN and have a general idea of when it should be used, but there are some important rules to remember when working with Medicare-Fee-For-Service patients. Not being adequately informed on these guidelines can lead to costly mistakes for your practice.
What does it mean when a provider is denied an ABN?
If the provider does not have a reasonable belief that the service or item that is normally payable will be denied than an ABN is prohibited from being issued.
What is a GA ABN?
GA – ABN was issued and signed by the beneficiary as required by Medicare (Beneficiary liable) GX – ABN was issued and signed by the beneficiary as voluntary (Beneficiary liable) GY – Indicates that the service is not a benefit of Medicare in any definition (Can be billed in combination with GX if patient signed an ABN. Beneficiary is liable.)
What is the 5 year rule for Medicare?
Note: The 5 year rule includes when an ABN is declined or refused. When the beneficiary signs the form and agrees to proceed with the service or item, you may seek payment from the patient. Keep in mind that if Medicare pays part or all of the service, a prompt refund to the beneficiary will be required. Changes of Mind.
Why is Medicare not paying for an item?
In addition, the reason for denial is because it is not medically reasonable and necessary.
What are the circumstances where you are prohibited from issuing an ABN?
Other circumstances were you are prohibited from issuing an ABN include: To make a beneficiary liable for Medically Unlikely Edit (MUE) denials. To make a beneficiary liable who is under great duress or in a medical emergency. To make a beneficiary liable for a code that was paid as part of a bundle service.
Can a beneficiary refuse to sign a corrected form?
A copy of the corrected form should be given to the beneficiary. In some cases the beneficiary may refuse to select an option or sign the form. If this occurs, the staff members will need to note the refusal to sign or select and list any witness present at the time of refusal.
What is an ABN in Medicare?
An ABN is a Medicare waiver of liability that providers are required to give a Medicare patient for services provided that may not be covered or considered. medically necessary. An ABN is used when service (s) provided may not be reimbursed by Medicare. If the healthcare provider believes that Medicare will not pay for some or all ...
What happens if you don't sign an ABN?
If there is no signed ABN then you cannot bill the patient and it must be written off if denied by Medicare.
What is an ABN for a primary care provider?
Examples of services that require an ABN include a visual field exam for an ophthalmologist, a pelvic exam for a primary care provider, or an echocardiogram. These exams should be covered as long as they ...
How long is a Medicare extended treatment notice valid?
A single notice for an extended course of treatment is only valid for 1 year. If the extended course of treatment continues after 1 year, issue a new notice.
When do you issue a reduction notice?
Reductions occur when a component of care decreases (for example, frequency or service duration). Do not issue the notice every time there is a reduction in care. If a reduction occurs and the beneficiary wants to continue getting care no longer considered medically reasonable and necessary, you must issue the notice before the beneficiary gets the noncovered care.
How long does it take for Medicare to refund a claim?
Medicare considers refunds timely within 30 days after you get the Remittance Advice from Medicare or within 15 days after a determination on an appeal if you or the beneficiary file an appeal.
Is an ABN valid for Medicare?
An ABN is valid if beneficiaries understand the meaning of the notice. Where an exception applies, beneficiaries have no financial liability to a non-contract supplier furnishing an item included in the Competitive Bidding Program unless they sign an ABN indicating Medicare will not pay for the item because they got it from a non-contract supplier and they agree to accept financial liability.
Does Medicare cover frequency limits?
Some Medicare-covered services have frequency limits. Medicare only pays for a certain quantity of a specific item or service in each period for a diagnosis. If you believe an item or service may exceed frequency limits, issue the notice before furnishing the item or service to the beneficiary.
Who completes the signature box on an ABN?
Once the beneficiary reviews and understands the information contained in the ABN, the Signature Box is to be completed by the beneficiary (or representative). This box cannot be completed in advance of the rest of the notice.
What is an ABN?
The ABN is a formal information collection subject to approval by the Executive Office of Management and Budget (OMB) under the Paperwork Reduction Act of 1995 (PRA). As part of this process, the notice is subject to public comment and re-approval every 3 years. With the latest PRA submission, a change has been made to the ABN. In accordance with Title 18 of the Social Security Act, guidelines for Dual Eligible beneficiaries have been added to the ABN form instructions.
What is an ABN in Medicare?
The ABN allows you to decide whether to get the care in question and to accept financial responsibility for the service (pay for the service out-of-pocket) if Medicare denies payment. The notice must list the reason why the provider believes Medicare will deny payment.
What is an ABN waiver?
An Advance Beneficiary Notice (ABN), also known as a waiver of liability, is a notice a provider should give you before you receive a service if, based on Medicare coverage rules, your provider has reason to believe Medicare will not pay for the service.
How to get an official decision from Medicare?
To get an official decision from Medicare, you must first sign the ABN, agreeing to pay if Medicare does not, and receive the care. Make sure you request that your provider bills Medicare for the service before billing you (the ABN may have a place on the form where you can elect this option).
Did not receive ABN before service?
You did not receive an ABN from your provider before you were given the service or item; Your provider had reason to believe your service or item would not be covered by Medicare; Your item or service is not specifically excluded from Medicare coverage; and. Medicare has denied coverage for your item or service.
What happens if a beneficiary refuses to sign a properly issued notice?
If a beneficiary refuses to sign a properly issued notice, consider not furnishing the item or service unless the consequences (health and safety of the beneficiary or civil liability in case of harm) prevent this option.
What to do if a beneficiary refuses to sign a notice?
If the beneficiary or the beneficiary’s representative refuses to choose an option or sign the notice, you should annotate the original copy indicating the refusal to choose an option or sign the notice. You may list any witnesses to the refusal, although a witness is not required. If a beneficiary refuses to sign a properly issued notice, consider not furnishing the item or service unless the consequences (health and safety of the beneficiary or civil liability in case of harm) prevent this option.
How long does an ABN last?
An ABN can remain effective for up to one year. The ABN must describe an extended or repetitive course of noncovered treatment as well as a list of all items and services believed to be non-covered. If applicable, the ABN must also specify the duration of the period of treatment.
When a representative is signing the ABN on behalf of a beneficiary, should the ABN be annotated
When a representative is signing the ABN on behalf of a beneficiary, the ABN should be annotated to identify that the signature was penned by the “rep” or “representative”. If the representative’s signature is not clearly legible, the representative’s name should be printed on the ABN. 8.
What does GA mean in Medicare?
Report modifier GA to indicate that the beneficiary received an advance written notice of the likelihood of denial of a service as being not reasonable and necessary under Medicare guidelines.
What happens if a beneficiary refuses to sign a written notice?
If a beneficiary refuses to sign a valid written notice, you should consider not furnishing the item or service unless the consequences (health and safety of the patient, or civil liability in case of harm) are such that this is not an option. Additionally, you may annotate the written notice indicating the circumstances and persons involved; have the annotation witnessed.
Where is the ABN located?
The ABN is located on the CMS website as well as on the Forms Catalog ( JH) ( JL) page of our website. 2.
What is pre-printed information?
If pre-printed information is used to describe items/services and/or common reasons for noncoverage, clearly indicate on the ABN which portions of the pre-printed information are applicable to the beneficiary. Providers who pre-print a list of items/services may wish to list a cost estimate beside each item/service.
When to report a GY modifier?
Report modifier GY when you believe a service will deny because the service is a statutory exclusion or does not meet the definition of any Medicare benefit. Append the GY modifier on non-covered line items on a claim with other covered services. Reference. ABN modifiers fact sheet.
How long does an ABN last?
An ABN can remain effective for up to one year. Notifiers may give a beneficiary a single ABN describing an extended or repetitive course of noncovered treatment provided that the ABN lists all items and services that the notifier believes Medicare will not cover.
When does ABN reduce?
Reductions. A reduction occurs when there is a decrease in a component of care (i.e., frequency, duration, etc.). The ABN is not issued every time an item or service is reduced. But, if a reduction occurs and the beneficiary wants to receive care that is no longer considered medically reasonable and necessary, the ABN must be issued prior ...
What is an initiation in healthcare?
An initiation is the beginning of a new patient encounter, start of a plan of care, or beginning of treatment. If a notifier believes that certain otherwise covered items or services will be non-covered (e.g., not reasonable and necessary) at initiation, an ABN must be issued prior to the beneficiary receiving the non-covered care.
What is termination ABN?
Terminations. A termination is the discontinuation of certain items or services. The ABN is only issued at termination if the beneficiary wants to continue receiving care that is no longer medically reasonable and necessary.
How often is Medicare screening?
ADVANCED BENEFICIARY NOTIFICATION. Medicare screening services are limited to a specific frequency (e.g., once every 2 years, once every year). A physician may not know whether a patient is eligible for this service in a given year. If she is not eligible, the service will be denied.
Can an ABN be retroactively dated?
However, if the ABN is issued after repetitive treatment has been initiated; the ABN cannot be retroactively dated or used to shift liability to the beneficiary for care that had been provided before ABN issuance. ADVANCED BENEFICIARY NOTIFICATION.