But most will discontinue it at age 18. Unless you have chidlren of your own (and still meet income/resournce guildlines) or are considered disabled by SSDI
Social Security Death Index
The Social Security Death Index is a database of death records created from the United States Social Security Administration's Death Master File Extract. Most persons who have died since 1936 who had a Social Security Number and whose death has been reported to the Social Security Administration are listed in the SSDI. For most years since 1973, the SSDI includes 93 percent to 96 percent of deaths of i…
What to do if my Medicare card has expired?
In addition, it shows your name and your Medicare claim number, along with the effective date of your Medicare coverage. How to Renew an Expired Medicare Card. As the time draws near to your Medicare card’s expiration date, you will receive a renewal notification in the mail. Through this, you should request a new ID card.
Why have I not received my Medicare card?
Nov 06, 2021 · For Medicare Advantage or prescription drug plans, permission to contact expires after 9 months. Medicare supplement product lines have a 90-day expiration date. Permission to contact MUST be established again after it expires even if ongoing contact is intended.
Does Medicare health insurance expire?
Dec 01, 2021 · Renewing Your Enrollment. You’re required to revalidate—or renew—your enrollment record periodically to maintain Medicare billing privileges. In general, providers and suppliers revalidate every five years but DMEPOS suppliers revalidate every three years. CMS also reserves the right to request off-cycle revalidations.
How do I get a replacement Medicare card?
Your plan doesn’t renew its Medicare contract for the following year. Your plan leaves the Medicare program in the middle of the year. Your plan’s contract is terminated by Medicare.
How long is Medicare good for?
Medicare covers Medicare provides 60 lifetime reserve days of inpatient hospital coverage following a 90-day stay in the hospital. These lifetime reserve days can only be used once — if you use them, Medicare will not renew them. Very few people remain in a hospital for 150 consecutive days.
Does a Medicare card expire?
Healthcare providers use the Medicare number on the card to bill services. Generally, a person does not have to renew their Medicare card each year, as it will automatically renew. If a card is lost, stolen, or damaged people can get a new card at no cost.Aug 11, 2020
How do I know if my Medicare is active?
How Do I Check the Status of My Medicare Enrollment? The status of your medical enrollment can be checked online through your My Social Security or MyMedicare.gov accounts. You can also call the Social Security Administration at 1-800-772-1213 or go to your local Social Security office.
Does Medicare have to be renewed every year?
In general, once you're enrolled in Medicare, you don't need to take action to renew your coverage every year. This is true whether you are in Original Medicare, a Medicare Advantage plan, or a Medicare prescription drug plan.Oct 9, 2021
Does Medicare renew automatically?
Although there are a few exceptions, Medicare plans generally renew each year automatically. This is true for original Medicare as well as Medicare Advantage, Medigap, and Medicare Part D plans.
Is Medicare issuing new cards in 2021?
All Medicare beneficiaries will be receiving new Medicare cards with their MBI. Current beneficiaries will be mailed a replacement Medicare card and instructions, while individuals who are new to Medicare in or after April 2018 will receive a new Medicare card with their MBI upon enrollment.
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
Are you automatically enrolled in Medicare if you are on Social Security?
Yes. If you are receiving benefits, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. (Medicare is operated by the federal Centers for Medicare & Medicaid Services, but Social Security handles enrollment.)
Can you lose Medicare benefits?
If you qualify for Medicare by age, you cannot lose your Medicare eligibility.
Why was I automatically enrolled in Medicare Part B?
You'll be automatically enrolled in Medicare Part A and Part B: If you are already getting benefits from Social Security or the Railroad Retirement Board. If you are younger than 65 and have a disability. If you have Lou Gehrig's disease, also called Amyotrophic Lateral Sclerosis, or ALS.Jan 28, 2020
Does Medicare coverage roll over?
You don't have to re-enroll in or renew Medicare each year. Your existing plan(s) will roll over automatically and remain in effect as long as you continue paying any necessary premiums.Oct 14, 2021
Does Medicare Part B renew automatically?
If you have Medicare Part A (hospital insurance) and/or Part B (medical insurance) and you are up to date on your Medicare premiums, your Medicare coverage will automatically carry over from one year to the next and there is nothing you need to do to renew your plan.Dec 8, 2021
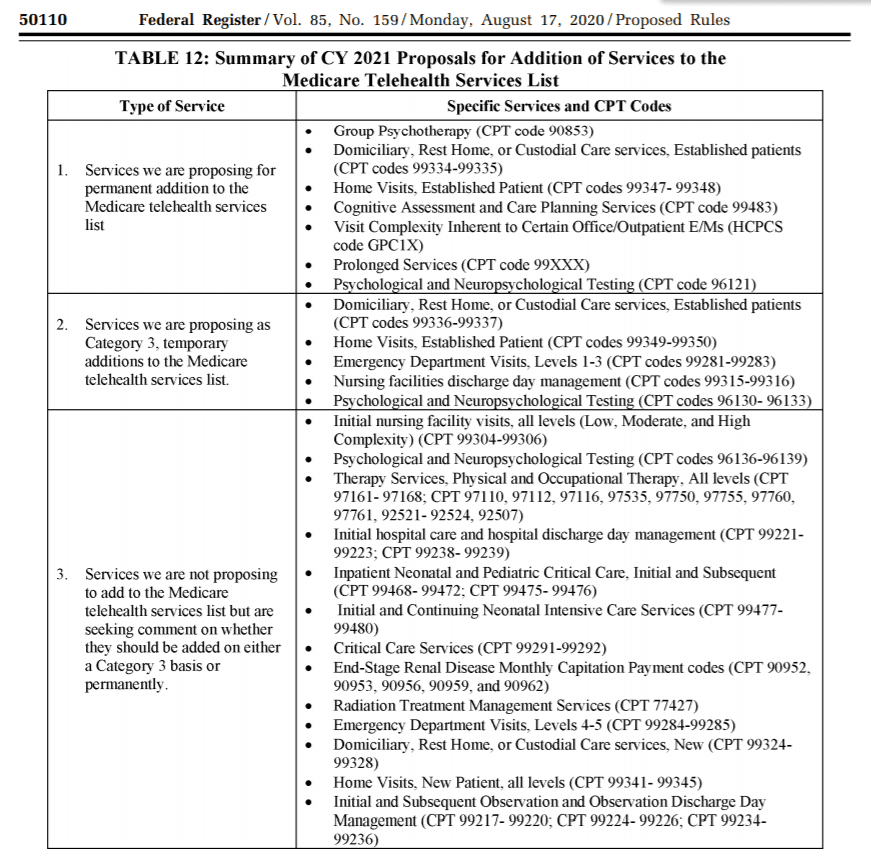
Which Services Qualify For A Cost
For the duration of the PHE, Medicare is waiving and will cover cost-sharing for COVID-19 diagnostic tests and visits related to COVID-19 testing. Additionally, physicians may voluntarily waive cost-sharing for non-COVID-19-related telehealth and virtual/digital services.
How To Compliantly Receive Permission To Contact
According to MCMG Guidelines, agents must have permission before they can make marketing calls. Cold calling, canvassing door to door, and other activities are strictly forbidden.
Medicare Scope Of Appointment Form
The Scope of Appointment is a requirement for in-person appointments. Agents must document their meetings with potential and current beneficiaries. The form goes on file for ten years and protects all parties. Sadly, many people have used a sales approach to profit from misunderstandings of the insurance world.
Establishing Permission To Contact Makes You A Better Agent
Establishing permission to contact is an agents best practice because it sets them apart from the unethical shady agents that do not comply and send intimidating emails or make unsolicited calls. Permission to contact also sets you up for the next step, scope of appointment forms.
Can I Provide Chronic Care Management Or Transitional Care Management Using Telehealth
Yes. CCM is already considered a non-face-to-face service. Patient consent is required. Verbal consent is sufficient and must be documented in the patient medical record. Patients who have not been seen in the office in the past 12 months must have an initiating visit, such as an office visit. The initiating visit may be provided via telehealth.
What Is Considered A Covid
The Coronavirus Aid, Relief, and Economic Security Act and the Families First Coronavirus Response Act require Medicare and group health plans to cover diagnostic testing related to COVID-19 at no cost to patients for the duration of the PHE. As defined by the laws, COVID-related services include:
What Does Medicare Permission To Contact Cover
Medicare beneficiaries will decide how they would like to be contacted whether that may be by phone call, email, direct mail, or the form they prefer most. Medicare beneficiaries also decide the time they would like to be called and what products they want more information on.
What happens if you don't revalidate Medicare?
Failing to revalidate on time could result in a hold on your Medicare reimbursement or deactivation of your Medicare billing privileges. If your Medicare billing privileges are deactivated, you’ll need to re-submit a complete Medicare enrollment application to reactivate your billing privileges.
Does Medicare reimburse you for deactivated services?
Medicare won’t reimburse you for any services during the period that you were deactivated. There are no exemptions from revalidation. Additionally, CMS doesn’t grant extensions; your notification email or letter will allow sufficient time to revalidate before your due date.
Can you revalidate a PECOS application?
Because PECOS is paperless, you won’t need to mail anything. Additionally, PECOS is tailored to ensure that you only submit information that’s relevant to your application. Revalidate online using PECOS.
What happens if my medicare card expires?
If your Medicare card has expired, your plan does not get renewed, or you feel anxious because you haven’t yet received a new one, the steps to get your card are relatively quick and easy .
What happens if my Medicare plan doesn't renew?
Your plan’s contract is terminated by Medicare. If your plan doesn’t automatically renew, you’ll have a special election period. During a special enrollment period for a Medicare Advantage nonrenewal, you can sign up for a Medicare supplement plan or change your coverage to a new Medicare Advantage plan.
What is a Medicare card?
Medicare cards are an important document that provide proof of your Medicare insurance. They contain: your name. your Medicare ID number. coverage information (Part A, Part B, or both) coverage dates. As long as you continue paying the required premiums, your Medicare coverage (and your Medicare card) should automatically renew every year.
How long does it take to get proof of Medicare?
If you need to prove that you have Medicare in less than 30 days, you can request temporary proof in the form of a letter. This will typically be received within 10 days. If you need proof immediately, such as for a doctor’s visit or prescription, the best option is to visit your nearest Social Security office.
How long does it take to get a new Social Security card?
Your new card should arrive in the mail at the address listed with your Social Security number within 30 days. If you don’t receive it in that time period, you may need to correct something in your account.
Does Medicare automatically renew?
There are some cases where Medicare renewal doesn’t happen automatically, specifically for Medicare Advantage or stand-alone Part D coverage. Some specific situations include: Your plan changes the size of its service area and you live outside that area.
When is the Medicare enrollment period?
The Medicare Annual Enrollment Period (also known as the Fall Medicare Open Enrollment Period for Medicare Advantage plans) takes place each year from October 15 to December 7. During this time, you may join, leave or switch Medicare Advantage plans or Medicare Part D plans.
What happens if a Medicare plan stops serving your area?
If this happens, all members of the plan will receive a notice informing them of the decision, and they will be granted a Special Enrollment Period to sign up for a different Medicare plan. The plan stops serving your area.
What is a SEP in Medicare?
Medicare Special Enrollment Period (SEP) Some Medicare beneficiaries may qualify for a Special Enrollment Period (SEP) at any time throughout the year to beneficiaries who experience a qualifying event. There are other reasons a beneficiary may qualify for a Medicare SEP.
What is the rating for Medicare Advantage?
Anyone who is enrolled in a Medicare Advantage or Medicare Part D plan with a rating of fewer than five stars is typically eligible to make changes to their Medicare coverage during the Five-Star Special Enrollment Period. 1
What is the definition of being released from jail?
Residing in, moving into or moving out of a skilled nursing facility or long-term care hospital. Being released from jail. Losing Medicaid eligibility. Losing or leaving employer, union or COBRA coverage. Losing drug coverage that’s at least as good as Medicare drug coverage.
How many stars does Medicare give?
Medicare rates all Medicare Advantage plans and Part D plans each year using the Medicare Star Rating system. Each plan is given a rating of one to five stars, with five stars being the highest ranking. 1. If a plan receives fewer than three stars for three consecutive years, Medicare will flag the plan as low performing.
How long can you carry Medigap?
For 30 days , you can carry two Medigap plans: your current plan and the plan you are considering changing to. At the end of the 30 day period, you will decide which plan to keep and which one to drop. You will need to pay the plan premiums for both plans while you are enrolled in each plan.
When do SS benefits expire?
These benefits expire when the child turns 18, or 19 if still in high school, or when you or the child dies.
When do disabled workers' benefits expire?
Disabled worker benefits expire either upon your death or if the SSA determines that you do not qualify for them any longer. If you are one of the millions of Americans who depend on your monthly social benefits check to live on, it is important to know the facts about whether your benefits expire.
How many people depend on SSDI?
The remaining one-fifth are either getting disability insurance benefits (SSDI) or are the dependent survivors of a deceased relative. Information and statistics gathered by the SSA reveal that 61 percent of retirees depend on their SS benefit check for 50 percent of their total monthly income. Also, people who are collecting disability benefits ...
What happens if you stop working because of an illness?
If you have to stop working because you are injured or have an illness, you may be eligible to receive SS benefits that are provided by the Disability Insurance Trust Fund.
How long do you have to be employed to get disability?
You can begin receiving disabled worker benefits after a six-month period elapses following your disability, and you must be certified as incapable of working for at least 12 months following the disability.
How many credits do you need to be eligible for Social Security?
1. Retirement Benefits. To be eligible for retirement benefits you must have at least 40 credits of Social Security. You earn these credits when you work and pay FICA taxes. The credit limit per year is four, but you can earn them any time during your life. Once you have earned credits they never expire.
When does a spouse receive SS benefits?
A surviving spouse is eligible to receive SS benefits upon the death of the working spouse.#N#If the spouse is younger than 60 but meets the eligibility requirements, the spouse receives benefits until they expire when the spouse turns 60.#N#If the surviving spouse is over 60, they receive benefits until they die.
What is Medicare Communications and Marketing Guidelines?
The Centers for Medicare & Medicaid Services (CMS) have published the Medicare Communications and Marketing Guidelines (MCMG) which governs the kind of language brokers and agents can use in informational and marketing materials.
How long does a PTC last?
For Medicare Advantage (MA) or Prescription Drug Plans (PDP), PTC expires 9 months after the date the request is received. However, the PTC for Medicare Supplement products is 90 days. It is important to note that the PTC must be renewed if it expires, even when ongoing contact is intended.
What does PTC cover?
What Does it Cover? Specifically, the Medicare Permission to Contact (PTC) rule outlines when it is okay to contact a current or potential Medicare beneficiary, the specific products they are giving you permission to contact them for, how you can approach them, and when you can contact them.
What does BRC mean on a phone call?
On the BRC, phone call, or email, the consumer will indicate what program they want information about. A client should indicate whether they want information on Medicare Supplements, Medicare Advantage, or both. Once a beneficiary gives permission for an agent to contact them, the agent still has to be careful.
Why were extensive guidelines issued?
Ultimately, extensive guidelines were issued to protect seniors from misinformation, pressure tactics, and fraud.
Can an agent contact a client without PTC?
An agent may contact a client without PTC if one of these criteria are met and the burden of proof can be met: Current, active contract with another product (i.e. life insurance) Ongoing, active business relationship. Agent of Record (AOR) for the beneficiary’s plan they are currently enrolled in.
