Full Answer
How to get a home health aide through Medicare?
- part-time skilled nursing care, which could include wound care, catheter care, vital signs monitoring, or intravenous therapy (such as antibiotics)
- occupational therapy
- physical therapy
- medical social services
- speech-language pathology
How much does Medicare pay for in home health care?
The only extra cost you’ll have for home health services is 20 percent of whatever durable medical equipment is needed for your services. Medicare covers the other 80 percent of the costs under your Part B plan. What Parts Aren’t Covered?
How to get Medicare to pay for home health care?
- You can’t leave home other than for short outings, such as going to the doctor or to religious services. ...
- Your doctor verifies that you need at-home care and writes a plan outlining the care you need.
- You need skilled nursing care (less than 8 hours per day and no more than 28 hours per week, for up to 3 weeks).
Does Medicare cover home health care aides?
Though Medicare Part A and Part B cover home health aides, they do not provide coverage for custodial care. They will only cover custodial care if you need it for a short period while you recover from an injury or illness. Medicare Advantage plans (Medicare Part C) also provide coverage for home health aides.

What is home health aide?
Home health aides are health professionals who help people in their home when they have disabilities, chronic illnesses, or need extra help. Aides may help with activities of daily living, such as bathing, dressing, going to the bathroom, or other around-the-home activities. For those who need assistance at home, home health aides can be invaluable.
What education do you need to be a home health aide?
According to the U.S. Bureau of Labor Statistics, the typical educational level for a home health aide is a high school diploma or equivalent. Some people may use the term “home health aide” to describe all occupations that provide care at home, but a home health aide is technically different from a home health nurse or therapist.
What is the difference between home health and skilled nursing?
The difference is that, for reimbursement, you must be getting skilled nursing services as well.
How to qualify for home health care?
Ideally, home health can enhance your care and prevent re-admission to a hospital. There are several steps and conditions to qualify for home health care: 1 You must be under the care of a doctor who has created a plan for you that involves home health care. Your doctor must review the plan at regular intervals to make sure it is still helping you. 2 Your doctor must certify that you need skilled nursing care and therapy services. To need this care, your doctor must decide that your condition will improve or maintain through home health services. 3 Your doctor must certify that you are homebound. This means it is very difficult or medically challenging for you to leave your home.
What is Medicare Part A?
Medicare Part A is the portion that provides hospital coverage. Medicare Part A is free to most individuals when they or their spouse worked for at least 40 quarters paying Medicare taxes.
Who must review home health care plans?
You must be under the care of a doctor who has created a plan for you that involves home health care. Your doctor must review the plan at regular intervals to make sure it is still helping you. Your doctor must certify that you need skilled nursing care and therapy services.
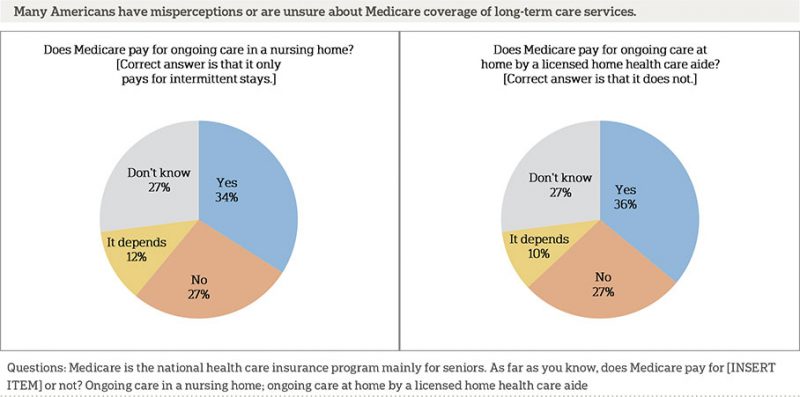
Is long term care insurance part of Medicare?
Some people choose to purchase separate long-term care insurance, which isn’t a part of Medicare . These policies may help to cover more home health care services and for longer time periods than Medicare. However, the policies vary and do represent an extra cost to seniors.
What is an ABN for home health?
The home health agency should give you a notice called the Advance Beneficiary Notice" (ABN) before giving you services and supplies that Medicare doesn't cover. Note. If you get services from a home health agency in Florida, Illinois, Massachusetts, Michigan, or Texas, you may be affected by a Medicare demonstration program. ...
What is a medical social service?
Medical social services. Part-time or intermittent home health aide services (personal hands-on care) Injectible osteoporosis drugs for women. Usually, a home health care agency coordinates the services your doctor orders for you. Medicare doesn't pay for: 24-hour-a-day care at home. Meals delivered to your home.
Does Medicare cover home health services?
Your Medicare home health services benefits aren't changing and your access to home health services shouldn’t be delayed by the pre-claim review process.
Do you have to be homebound to get home health insurance?
You must be homebound, and a doctor must certify that you're homebound. You're not eligible for the home health benefit if you need more than part-time or "intermittent" skilled nursing care. You may leave home for medical treatment or short, infrequent absences for non-medical reasons, like attending religious services.
Who is covered by Part A and Part B?
All people with Part A and/or Part B who meet all of these conditions are covered: You must be under the care of a doctor , and you must be getting services under a plan of care created and reviewed regularly by a doctor.
Can you get home health care if you attend daycare?
You can still get home health care if you attend adult day care. Home health services may also include medical supplies for use at home, durable medical equipment, or injectable osteoporosis drugs.
What is home health agency?
The home health agency will be responsible for all of your medical, nursing, and rehabilitative care and will communicate your needs to the managing physician. Your condition will be monitored and assessed regularly and will create discharge plans when appropriate.
What can a registered nurse do for home care?
A registered nurse or licensed practical nurse may administer your home care which may include giving IV drugs, changing wound dressings, tube feedings, teaching about diabetes care, or certain injections. The home health aides must work for a Medicare-approved home health agency and your doctor must certify that you are homebound.
Is home health care as effective as inpatient care?
Most patients would prefer to receive care for an illness or injury in the comfort of their own home. Fortunately, home health care can be as effective as inpatient care in a hospital or skilled nursing facility. Studies on healing at home have shown improved outcomes and quicker recoveries for patients. Home health care can be less costly ...
Does Medicare cover home health care?
Home health care can be less costly than a long hospital stay and Medicare can help cover the costs. If your physician orders reasonable and medically necessary treatment of an illness or injury, Medicare will help pay for home health services as long as you meet certain criteria.
Do home health aides have to be Medicare approved?
The home health aides must work for a Medicare-approved home health agency and your doctor must certify that you are homebound. These agencies agree to be paid the Medicare-approved amount and to be paid directly by Medicare. The home health agency will be responsible for all of your medical, nursing, and rehabilitative care ...
Does Medicare Part B cover out of pocket costs?
The Medicare Part B deductible will apply. Many Medicare recipients choose to purchase supplemental insurance to help cover the out-of-pocket costs from Part A and Part B. If you have enrolled in a Medigap plan, it may help pay for deductibles and coinsurance associated with home health care.
What kind of home health services does Medicare cover?
Here’s the kind of home health services Medicare may cover: Part-time or intermittent home health aide. Part-time or intermittent skilled nursing care. Physical and/or occupational therapy. Speech language pathology services. Medical social services.
What does it mean to be homebound on Medicare?
Medicare considers homebound to mean you can’t leave your home without help, or your health condition generally requires you to stay at home.
How much does Medicare pay for durable medical equipment?
If you need durable medical equipment, you’ll typically pay 20% of the Medicare-approved amount. Be aware, however, that your doctor might request more home health care services for you than Medicare will approve. If you have questions, ask your doctor, or call Medicare at the number listed at the bottom of this page.
Does Medicare cover home health aides?
Medicare Part A (hospital insurance) and/or Part B (medical insurance) may cover home health aides if your doctor orders this care for you and determines that it’s medically necessary. Usually Medicare won’t cover a full-time, long-term home health aide.
Does Medicare cover laundry?
Also, be aware that: Homemaker services, such as shopping or laundry, aren’t generally covered under Medicare. Medicare doesn’t cover meals delivered to your house.
What is home health aide?
Home health aides, when the only care you need is custodial. That means you need help bathing, dressing, and/or using the bathroom. Homemaker services, like cleaning, laundry, and shopping. If these services aren’t in your care plan, and they’re the only care you need, they’re generally not covered.
Do you have to be Medicare approved to be homebound?
The in-home health agency must be Medicare-approved. Your doctor must certify that you’re unable to leave your home without some difficulty – for example, you might need transportation and/or help from a cane, a walker, a wheelchair, and/or someone to help you. In other words, you’re homebound.
Does Medicare cover in-home care?
When might Medicare cover in-home health care? In general, Medicare doesn’t cover long- term home health care. Here’s how Medicare coverage of in-home health care typically works. In most cases, even when Medicare covers in-home health care, it’s for part-time care, and for a limited time.
Does Medicare Advantage have a deductible?
Medicare Advantage plans may have annual deductibles, and may charge coinsurance or copayments for these services. Medicare Advantage plans have out-of-pocket maximum amounts, which protect you from unlimited health-care spending.
How do I contact Medicare for home health?
If you have questions about your Medicare home health care benefits or coverage and you have Original Medicare, visit Medicare.gov, or call 1-800-MEDICARE (1-800-633-4227) . TTY users can call 1-877-486-2048. If you get your Medicare benefits through a Medicare Advantage Plan (Part C) or other
What happens when home health services end?
When all of your covered home health services are ending, you may have the right to a fast appeal if you think these services are ending too soon. During a fast appeal, an independent reviewer called a Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) looks at your case and decides if you need your home health services to continue.
What is an appeal in Medicare?
Appeal—An appeal is the action you can take if you disagree with a coverage or payment decision made by Medicare, your Medicare health plan, or your Medicare Prescription Drug Plan. You can appeal if Medicare or your plan denies one of these:
Why is home health important?
In general, the goal of home health care is to provide treatment for an illness or injury. Where possible, home health care helps you get better, regain your independence, and become as self-sucient as possible. Home health care may also help you maintain your current condition or level of function, or to slow decline.
Can Medicare take home health?
In general, most Medicare-certified home health agencies will accept all people with Medicare . An agency isn’t required to accept you if it can’t meet your medical needs. An agency shouldn’t refuse to take you because of your condition, unless the agency would also refuse to take other people with the same condition.
How much does a home health aide cost?
Cost of hiring a caregiver. A 2019 industry survey on home health costs found that a home health aide is likely to cost an average of $4,385 per month. The same survey listed the average monthly cost of a caregiver to provide custodial care services as $4,290.
What do you need to be a home health aide?
You need a home health aide to help care for you while you recover. The home health agency providing your care is Medicare-approved or certified.
What is a Medicare supplement?
If you think you or someone in your family might need custodial care, you may want to consider a long-term care insurance policy to help you cover the cost. A Medicare supplement (Medigap) plan may also help you pay some of the costs that Medicare won’t cover.
How long does Medicare Part A cover?
If you were admitted to the hospital for 3 consecutive days or Medicare covered your stay in a skilled nursing facility, Part A will cover home healthcare for 100 days, as long as you receive home health services within 14 days of leaving the hospital or nursing facility .
What is Medicare Part B?
Medicare Part B is medical coverage. If you need home health services but weren’t admitted to the hospital first, Part B covers your home healthcare. You do have to meet the other eligibility requirements, though.
How long do you have to see a doctor before you can get home health care?
To remain eligible for in-home care, you’ll need to see your doctor fewer than 90 days before or 30 days after you start receiving home healthcare services.
How many hours of nursing do you need?
Your doctor verifies that you need at-home care and writes a plan outlining the care you need. You need skilled nursing care (less than 8 hours per day and no more than 28 hours per week, for up to 3 weeks). Your doctor thinks your condition is going to improve in a reasonable, or at least predictable, amount of time.
Medicare Covers Medically Necessary Home Health Services
Medicare does not usually cover the cost of non-medical home care aides if that is the only type of assistance that a senior needs.
Medicare Advantage May Offer More Comprehensive Coverage
Private insurance companies run Medicare Advantage. Those companies are regulated by Medicare and must provide the same basic level of coverage as Original Medicare. However, they also offer additional coverage known as “supplemental health care benefits.”