Will Missouri lawmakers expand Medicaid in 2019?
Medicaid expansion was not considered by Missouri lawmakers during the 2019 legislative session. But SB713, introduced in the 2018 session, would have expanded Medicaid eligibility to include adults with income up to 138 percent of the poverty level, as called for in the ACA, with an effective date of January 2019.
When will I get my Medicare card?
When Will I Get My Medicare Card? When you reach the age of 65 or have been disabled and receiving Social Security benefits for 24 months, you may become eligible for Medicare insurance. This insurance provides good coverage for both inpatient and outpatient healthcare services.
Are you eligible for Medicaid long-term care in Missouri?
The American Council on Aging now offers a free, quick and easy Medicaid eligibility test for seniors. There are several different Medicaid long-term care programs for which Missouri seniors may be eligible.
Does Miss Missouri have a targeted enrollment strategy for Medicaid?
Missouri has adopted one or more of the targeted enrollment strategies outlined in guidance CMS issued on May 17, 2013, designed to facilitate enrollment in Medicaid and CHIP. In federal fiscal year (FFY) 2019, Missouri voluntarily reported 16 of 21 frequently reported health care quality measures in the CMS Medicaid/CHIP Child Core Set.

Is Medicare changing their cards for 2022?
15 through Dec. 7, the more than 63 million Medicare beneficiaries can pick a new Medicare Part D drug plan, a new Medicare Advantage plan, or switch from Original Medicare into a Medicare Advantage plan or vice versa. Any coverage changes made during this period will go into effect Jan. 1, 2022.
Is Medicare issuing a new card in 2021?
TIPS: Here's what you should know: Medicare IS NOT sending new 2021 Medicare cards. number is no longer your Social Security number.
When should I expect my Medicare card?
Your Medicare card should arrive about three months before your 65th birthday, and your Medicare coverage starts the first day of the month you turn 65.
Are they sending out new Medicare cards this year?
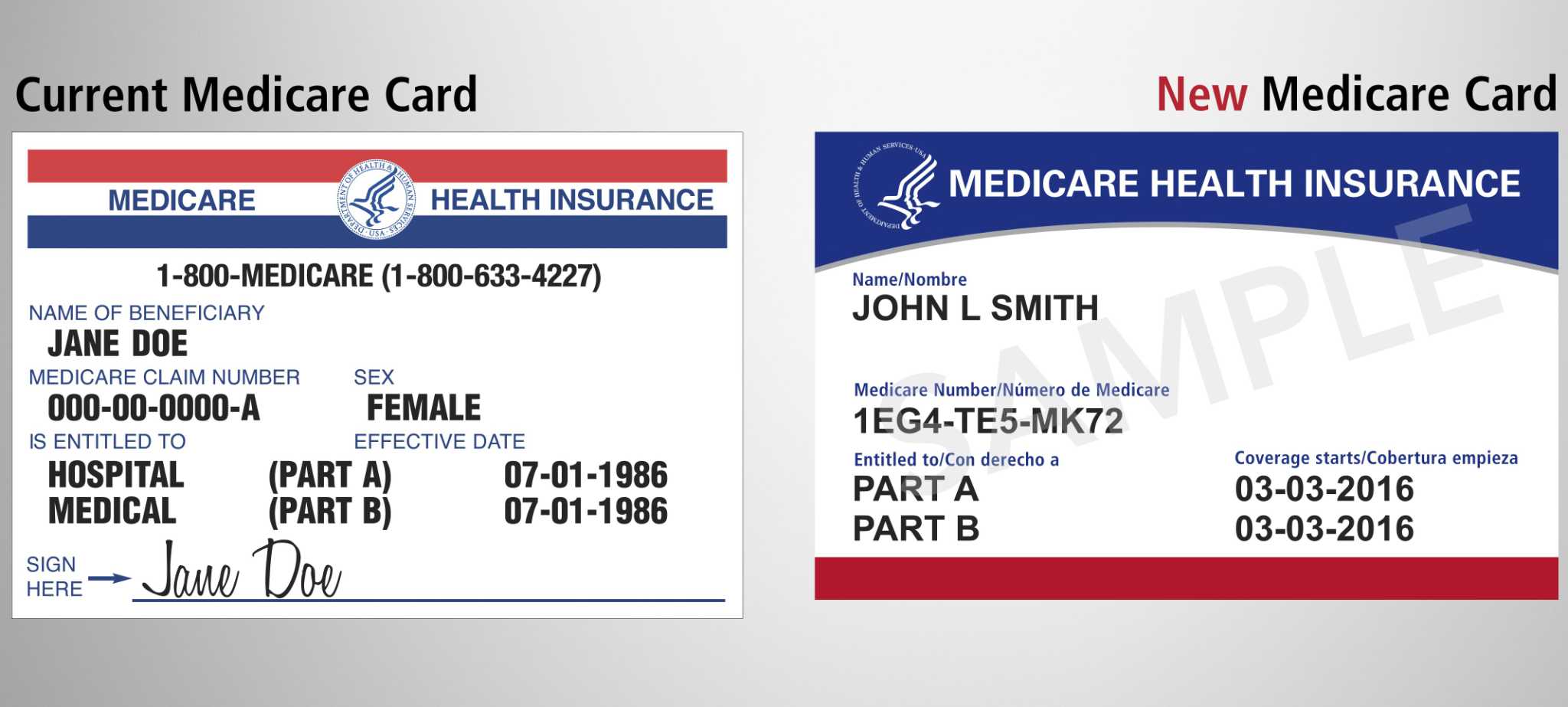
You're getting a new Medicare card! Between April 2018 and April 2019, we'll be removing Social Security numbers from Medicare cards and mailing each person a new card. This will help keep your information more secure and help protect your identity.
Is Medicare calling to issue new cards?
Medicare isn't issuing new cards and Medicare employees don't contact participants through unsolicited calls, emails, or visits. Medicare communicates with beneficiaries via mail. Scammers falsely allege Medicare is issuing new plastic or metal Medicare cards or black and white Covid-19 Medicare cards.
Does Medicare automatically send you a card?
You should automatically receive your Medicare card three months before your 65th birthday. You will automatically be enrolled in Medicare after 24 months and should receive your Medicare card in the 25th month.
Will Medicare automatically send me a Medicare card?
Once you're signed up for Medicare, we'll mail you your Medicare card in your welcome packet. You can also log into (or create) your secure Medicare account to print your official Medicare card. I didn't get my Medicare card in the mail. View the Medicare card if you get benefits from the Railroad Retirement Board.
Are all new Medicare cards mailed?
A new, unique Medicare Number is replacing the SSN-based Health Insurance Claim Number (HICN) on each new Medicare card. Starting April 2018, CMS is mailing new Medicare cards to all people with Medicare on a flow basis, based on geographic location and other factors.
How much money can you make to qualify for Medicaid in Missouri?
All Medicaid-eligible populations are subject to income limits (as we’ll discuss in a moment, some populations are also subject to asset limits). I...
What is the asset limit for Medicaid in Missouri?
For the groups described above, only an income limit applies. But for Missouri Medicaid applicants whose eligibility is based on their status as ag...
How does Medicaid provide assistance to Medicare beneficiaries in Missouri?
Many Medicare beneficiaries receive help through Medicaid with the cost of Medicare premiums, co-pays, deductibles, and services Medicare doesn’t c...
How many signatures are needed for Medicaid expansion in Missouri?
Advocates spent the summer determining the feasibility of Medicaid expansion by ballot initiative in Missouri, and announced in September 2019 that they would commit to gathering the 172,000 signatures necessary for the measure to appear on the ballot.
When will Medicaid be expanded?
Constitutional amendment to expand Medicaid was approved by voters in August 2020 election. The Medicaid expansion ballot measure passed in August 2020 by a margin of about 53 to 47. It called for the state to submit a Medicaid expansion state plan amendment to the federal government by March 2021, and for Medicaid expansion to take effect by July ...
How much will Medicaid be available in 2021?
In 2021, that amounts to about $17,774 for a single individual, and $36,570 for a household of four (children are already eligible for Medicaid at higher income levels).
What is the income threshold for CHIP 2021?
For a household of three in 2021, that amounts to just under $33,000 in annual income. Children above the Medicaid income thresholds are eligible for CHIP if their household incomes are up to 300% of poverty.
How many people are in the coverage gap in Missouri?
For now, 127,000 people remain in the coverage gap in Missouri — unable to qualify for Medicaid because the state still has not expanded eligibility for Medicaid coverage, and unable to qualify for premium subsidies in the exchange/marketplace because they earn less than the poverty level.
Which states have lower Medicaid eligibility caps?
Only Texas and Alabama have lower Medicaid eligibility caps, at 18%. As the ACA was written, it called for Medicaid expansion in every state for residents with incomes up to 133% of poverty (138% with the built-in 5% income disregard). But in 2012, the Supreme Court ruled that states could not be penalized for opting out of expansion, ...
When will the Missouri Supreme Court hear the appeal?
But lawmakers refused to implement it, and a judge sided with the lawmakers. An appeal will be heard by the Missouri Supreme Court in July 2021.
EBT Card
If your EBT card has been lost, stolen, or damaged, please call 800-997-7777 to ask for a replacement EBT card. You can also call the FSD Information Center at 855-FSD-INFO (855-373-4636).
Healthcare Card
If you need a new MO HealthNet ID card, please call 855-FSD-INFO (855-373-4636). If you need a new Managed Care health plan card, please reach out to your health plan directly:
How many months are you eligible for Medicare?
The seven months encompass the three months prior to your birthday, your birth month, and the three months following your birth month. You are able to apply for Medicare in a few different ways. If you prefer to apply in person, you can do so at your local Social Security office.
How long does it take to get Medicare?
This date marks the beginning of your Initial Enrollment Period. This period lasts for a total of seven months , and you must apply for Medicare coverage during this period to avoid having to pay late enrollment penalties. The seven months encompass the three months prior to your birthday, your birth month, and the three months following your birth month.
What happens after you enroll in Medicare?
After enrolling in Medicare, you will receive your Medicare identification card so that you can use it to receive healthcare coverage at a variety of different facilities across the United States. Since Medicare is a government-run entity, applications for insurance coverage are handled by the Social Security Administration.
Is Medicare dependent on Social Security?
Unlike Social Security benefits, Medicare eligibility is not dependent on retirement. However, if you are already receiving Social Security benefits at the age of 65, you will automatically be enrolled in Medicare. It is important to note that even if you are automatically enrolled in Part A and Part B, you still must apply to Part D separately ...
Does Medicare cover prescription drugs?
Original Medicare encompasses both Part A and Part B. At the time you apply for Original Medicare, you also have the ability to sign up for Medicare Part D coverage, which covers prescription drugs.
What is CSRA in Missouri?
This, in Medicaid speak, is called the Community Spouse Resource Allowance (CSRA) and is intended to prevent spousal impoverishment. The CSRA does not extend to non-applicant spouses of regular Medicaid applicant spouses. It’s important to be aware that Missouri has a 5-year Medicaid Look-Back Period.
What is MO HealthNet?
Medicaid, which is called MO HealthNet in Missouri, is a wide-ranging, jointly funded state and federal health care program. Through MO HealthNet, many groups of low-income people, including pregnant women, families, and the blind, disabled, and elderly are able to receive medical and care assistance. That being said, this page is focused on ...
What income is counted for Medicaid?
Examples include employment wages, alimony payments, pension payments, Social Security Disability Income, Social Security Income, IRA withdrawals, and stock dividends.
What is MMMNA in Medicaid?
Relevant to married couples with one spouse applying for home and community based services via a Medicaid waiver or nursing home Medicaid, there is a Minimum Monthly Maintenance Needs Allowance (MMMNA). This is the minimum amount of monthly income to which the non-applicant spouse is entitled.
When only one spouse of a married couple is applying for nursing home Medicaid or a HCBS waiver, is
When only one spouse of a married couple is applying for nursing home Medicaid or a HCBS Medicaid waiver, only the income of the applicant is counted. Said another way, the income of the non-applicant spouse is disregarded.
What is institutional Medicaid?
1) Institutional / Nursing Home Medicaid – is an entitlement (anyone who is eligible will receive assistance) and is provided only in nursing homes. 2) Medicaid Waivers / Home and Community Based Services – Limited number of participants and is provided at home, adult day care or in assisted living. More on Waivers.
Do you need a nursing facility for Medicaid?
For nursing home Medicaid and many HCBS Medicaid Waivers, a nursing facility level of care (NFLOC) is required . Moreover, some program benefits, such as home modifications, may have additional eligibility criteria. For instance, the inability to safely live at home without modification of the home may be necessary.
View Another State
Explore key characteristics of Medicaid and CHIP in , including documents and information relevant to how the programs have been implemented by within federal guidelines.
Eligibility in
Information about how determines whether a person is eligible for Medicaid and CHIP.
Enrollment in
Information about efforts to enroll eligible individuals in Medicaid and CHIP in .
Quality of Care in
Information about performance on frequently-reported health care quality measures in the CMS Medicaid/CHIP Child and Adult Core Sets in .