When will my first Medicare premium bill be due?
If you enroll in Medicare before you begin collecting Social Security benef it s, your first premium bill may surprise you. It will be due, paid in full, 1 month before your Medicare coverage begins. This bill will typically be for 3 months’ worth of Part B premiums. So, it’s known as a quarterly bill.
When will my Medicare premium be deducted from my check?
The Medicare premium deducted from that check will also be for July. If you have original Medicare and aren’t yet collecting Social Security, you’ll receive a bill from Medicare either monthly or once every 3 months in these cases: If you don’t have premium-free Part A, you’ll receive a monthly bill for your Part A premium.
What happens when you pay Medicare premiums in advance?
If you pay a Part A premium, you’ll also receive a bill from Medicare. These bills are paid in advance for the coming month or months, depending on the parts of Medicare you’re paying for. If you’re already receiving retirement benefits, your premiums may be automatically deducted from your check.
What does it mean when you get a Medicare check in August?
This means that the benefit check you receive is for the previous month. For example, the Social Security benefit check you receive in August is for July benefits. The Medicare premium deducted from that check will also be for July. When to pay for original Medicare
How do I find out when my Medicare payment is due?
All Medicare bills are due on the 25th of the month. In most cases, your premium is due the same month that you get the bill. Example of our billing timeline. For your payment to be on time, we must get your payment by the due date on your bill.
When should I receive my Medicare bill?
People who do not receive these benefits must pay their parts A and B premiums and the Part D IRMAA each month. Those who only pay for Part B will pay every 3 months. Medicare bills arrive on or around the 10th day of the month, and the payment is due by the 25th.
Does Medicare bill quarterly?
BILL TYPE Some people with Medicare are billed either monthly or quarterly. If you are billed for Part A or IRMAA Part D, you will be billed monthly. If this box says: • FIRST BILL, it means your last payment was received timely or this is your initial bill. SECOND BILL, it means a payment is late by at least 60 days.
Does Medicare send monthly statements?
It's a notice that people with Original Medicare get in the mail every 3 months for their Medicare Part A and Part B-covered services. The MSN shows: All your services or supplies that providers and suppliers billed to Medicare during the 3-month period.
Are Medicare premiums deducted a month in advance?
If you pay a Part A premium, you'll also receive a bill from Medicare. These bills are paid in advance for the coming month or months, depending on the parts of Medicare you're paying for. If you're already receiving retirement benefits, your premiums may be automatically deducted from your check.
Can I see my Medicare premium bill online?
You can use your online MyMedicare account to view your Medicare premium bills, check your payment history and set up Medicare Easy Pay for auto payments.
What is the Medicare Part B premium for 2021?
$148.50Medicare Part B Premium and Deductible The standard monthly premium for Medicare Part B enrollees will be $170.10 for 2022, an increase of $21.60 from $148.50 in 2021. The annual deductible for all Medicare Part B beneficiaries is $233 in 2022, an increase of $30 from the annual deductible of $203 in 2021.
How often does Medicare bill for Part B?
Part B premiums You pay a premium each month for Part B. Your Part B premium will be automatically deducted from your benefit payment if you get benefits from one of these: Social Security. Railroad Retirement Board.
Are Medicare Part B premiums going up in 2021?
In November 2021, CMS announced the monthly Medicare Part B premium would rise from $148.50 in 2021 to $170.10 in 2022, a 14.5% ($21.60) increase.
How do I get my yearly Medicare statement?
If you have lost your MSN or you need a duplicate copy, call 1-800-MEDICARE or go to your account on www.mymedicare.gov.
Can I get my Medicare Summary Notice Online?
Yes, Medicare summary notices are available online — but you must sign up to receive them electronically. If you opt for electronic notices, you'll stop receiving printed copies of your MSNs in the mail. Instead, you'll get an email every month from your online My Medicare Account.
Does Medicare send a year end statement?
At the end of each year, Medicare sends a 1095-B statement. This statement shows the IRS a person had qualifying health insurance that year. An individual may receive more than one statement if they have a secondary insurance policy.
When was the Medicare buy in manual released?
Manual for State Payment of Medicare Premiums (formerly called “State Buy-in Manual”) On September 8, 2020, the Centers for Medicare & Medicaid Services (CMS) released an updated version of the Manual for State Payment of Medicare Premiums (formerly called “State Buy-in Manual”). The manual updates information and instructions to states on federal ...
How many people pay Medicare Part B?
States pay Medicare Part B premiums each month for over 10 million individuals and Part A premium for over 700,000 individuals.
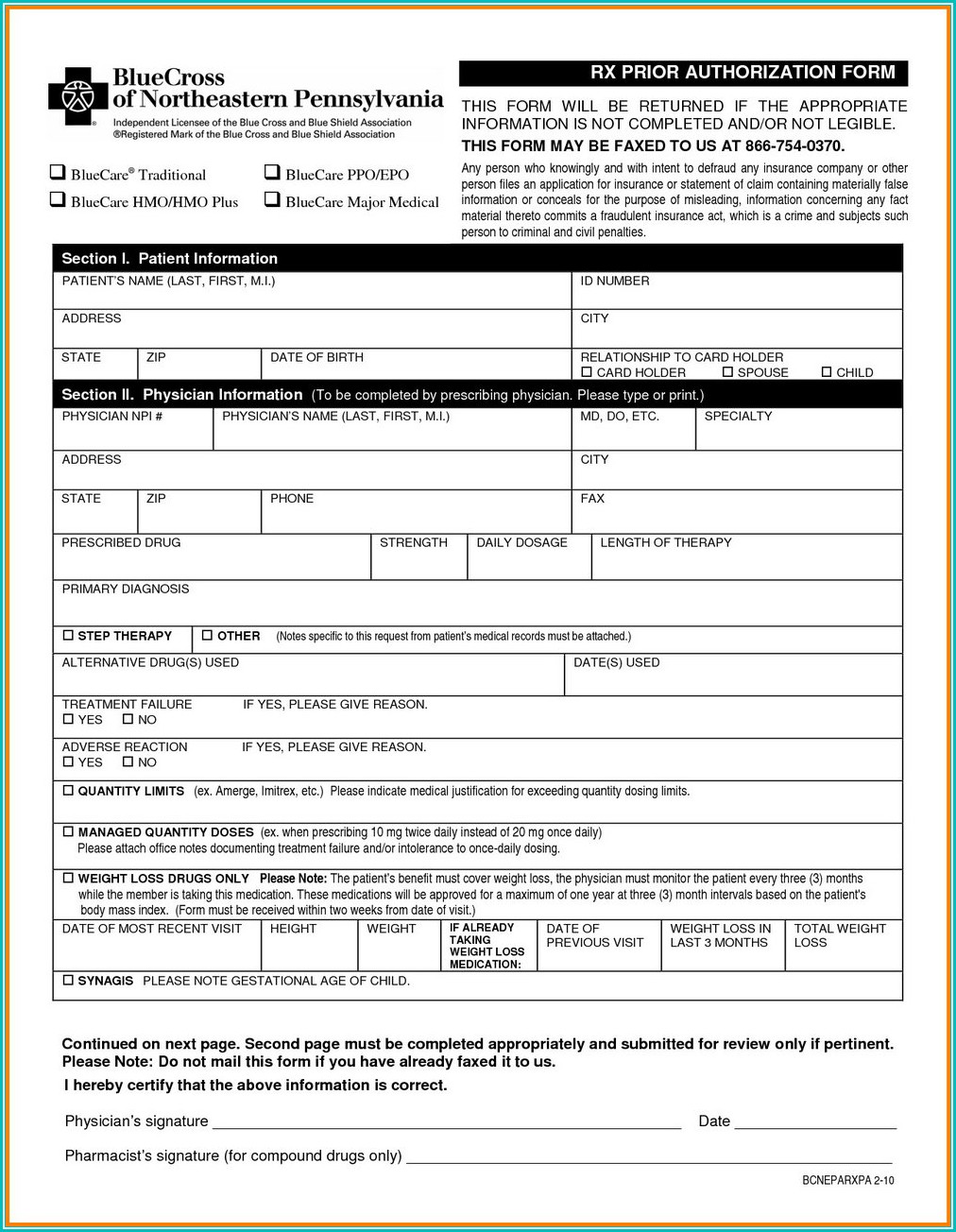
When is Medicare Part D notice required?
According to CMS, the requirement to provide the notice prior to an individual's initial enrollment period will also be satisfied as long as the notice is provided to all plan participants each year before the beginning of the Medicare Part D annual enrollment period.
When does Medicare have to disclose coverage?
This disclosure must be made no more than 60 days after the beginning of each plan year— generally, by March 1. The CMS disclosure obligation applies to all plan sponsors that provide prescription drug coverage, even those that do not offer prescription drug coverage to retirees.
Why is no notice required when prescription drug coverage is not offered?
Because the notice informs individuals whether their prescription drug coverage is creditable or non-creditable , no notice is required when prescription drug coverage is not offered.
How many days can you go without Medicare Part D?
Individuals who do not enroll in Medicare Part D during their initial enrollment period, and who subsequently go at least 63 consecutive days without creditable coverage (e.g., because they dropped their creditable coverage or have non-creditable coverage) generally will pay higher premiums if they enroll in a Medicare drug plan at a later date.
What language are CMS model notices available in?
Model notices that can be used to satisfy creditable/non-creditable coverage disclosure requirements are available in both English and Spanish on the CMS website.
When is the enrollment period for Medicare Part D?
The Medicare Part D annual enrollment period runs from Oct. 15 to Dec. 7. Each year , before the enrollment period begins (i.e., by Oct. 14), plan sponsors must notify Medicare-eligible individuals whether their prescription drug coverage is creditable or non-creditable. The Oct. 15 deadline applies to insured and self-funded plans, regardless of plan size, employer size or grandfathered status.
Is prescription drug coverage creditable?
Prescription drug coverage is creditable when it is at least actuarially equivalent to Medicare's standard Part D coverage and non-creditable when it does not provide , on average, as much coverage as Medicare's standard Part D plan.
How long is Medicare payment due?
If a Medicare recipient receives the first notice of a premium being due and it remains unpaid, a second notice goes out saying the payment is 60 days late, the spokesman said. If the premium still is unpaid, next is a delinquency notice and final bill saying the payment is 90 days late, he said.
What happens if you get late arriving Medicare?
The beneficiaries hit with the late-arriving bills are in a subset of the people who use Medicare. The subset comprises people who accept Medicare coverage but are not yet drawing Social Security benefits. If a person receives benefits from both programs, as is usually the case, Medicare premiums are deducted from Social Security checks.
How to pay Medicare premiums?
People should pay the premiums “as soon as possible” and put their Medicare number on their check or money order. Payments also may be made via the mail using a major credit card. To avoid using snail mail, here are two other ways to pay: Use your bank’s online payment mechanism.
How many Americans are covered by Medicare?
Altogether, an estimated 59.1 million Americans are covered by Medicare Part A and/or B, according to a July 2018 report from CMS. Part A covers hospital care and some nursing home, rehabilitation and hospice care. Part B covers doctor visits, lab tests, screenings and other outpatient services.
Is Medicare mailed late?
After some Medicare premium bills for December were mailed late , a spokesman at the Centers for Medicare & Medicaid Services (CMS) said Wednesday the agency is trying to identify beneficiaries at risk of being terminated so they can keep their health coverage.
What happens to Medicare premiums once you start?
Once your benefits begin, your premiums will be taken directly out of your monthly payments. You’ll also receive bills directly from your plan’s provider if you have any of the following types of plans: Medicare Part C, also known as Medicare Advantage. Medicare Part D, which is prescription drug coverage.
How long does it take to pay Medicare premiums?
If you enroll in Medicare before you begin collecting Social Security benef it s, your first premium bill may surprise you. It will be due, paid in full, 1 month before your Medicare coverage begins. This bill will typically be for 3 months’ worth of Part B premiums. So, it’s known as a quarterly bill.
What about Part C, Part D, and Medigap?
You pay these bills directly to your plan provider. Each company may have a preferred method of payment.
What does it mean when you receive a Social Security check in August?
This means that the benefit check you receive is for the previous month. For example, the Social Security benefit check you receive in August is for July benefits. The Medicare premium deducted from that check will also be for July.
How much is Medicare Part B 2021?
Medicare Part B costs. Most people pay the standard Part B premium. In 2021, that amount is $148.50. If the modified adjusted gross income you reported on your taxes from 2 years ago is higher than a certain limit, though, you may need to pay a monthly IRMAA in addition to your premium.
What is Medicare Part D?
Medicare Part D, which is prescription drug coverage. Medigap, also called Medicare supplement insurance. The structure of these bills and their payment period may vary from insurer to insurer. Social Security and RRB benefits are paid in arrears. This means that the benefit check you receive is for the previous month.
How often do you get Medicare premiums?
If you’re not receiving these benefits, you’ll get a bill for your premiums, either monthly or quarterly, depending on which part of Medicare you’re paying for. These bills are paid in advance of your coverage.
Who receives Medicare refund?
The individual or entity that paid the excess Medicare premiums receives the refund. The payer may be:
What is Medicare excess?
The law requires the Centers for Medicare & Medicaid Services (CMS) to dispose of excess Medicare premiums paid by , or on behalf of , a deceased beneficiary. The excess premiums may be for supplementary medical insurance (SMI) or hospital insurance (HI). They could be the result of premiums paid for months of coverage following the individual’s death or be the result of retroactive premium adjustments for months of coverage before the individual’s death, such as:
What is a beneficiary in a CMS?
an entity with a third party payer arrangement with CMS. 1. Beneficiary is the premium payer. When the Social Security Administration (SSA) records do not indicate that a third party payer or another individual paid the deceased beneficiary’s premiums, assume that the deceased beneficiary paid them.
What is a third party payer?
Third party payers are typically organizations, municipalities, or other entities that pay premiums on behalf of a group of beneficiaries. These include:
When a beneficiary not covered under a State buy-in agreement has entitlement to both a Social Security benefit and?
When a beneficiary not covered under a State buy-in agreement has entitlement to both a Social Security benefit and a Railroad Retirement annuity or pension, the beneficiary pays SMI premiums to the RRB. The RRB handles refunds to these deceased beneficiaries.
What does MARD stand for in Medicare?
annotation or change in Medicare Advantage Reduction (MARD).
Who pays Medicare premiums to a deceased person?
In cases where there is an A80022 alert and SSA records indicate payment by the deceased beneficiary and a third party payer for the same months, pay the excess Medicare premiums to the deceased beneficiary, or the individual who paid premiums of behalf of the beneficiary. This is because the third party payer can retroactively pay ...