Do Medicare Part D plans automatically renew?
If you have another form of Medicare coverage – such as a Medicare Advantage plan (Medicare Part C), a Medicare Part D plan or a Medicare Supplement Insurance plan (Medigap) – your coverage should renew automatically, as long as the plan is still being provided and you are paying your plan premiums.
When does Medicare coverage automatically renew?
With a few exceptions, Medicare coverage automatically renews at the end of each year. If a plan decides it will no longer contract with Medicare, your plan will not renew.
How does Medicare Part D work?
It works the same whether you have Original Medicare (Parts A and B), a Medicare Advantage plan (Part C) or a Medicare prescription drug plan (Part D). You simply do nothing and your current coverage choices stay in place for another year.
Do I have to reenroll in my Medicare Part D prescription drug plan?
Do I have to reenroll in my Medicare Part D prescription drug plan every year? En español | If you like your current Part D drug plan, you can remain with it into the following plan year, which begins Jan. 1. You don’t have to reenroll or inform the plan that you’re staying.
Does Medicare Part D automatically renew?
Like Medicare Advantage, your Medicare Part D (prescription drug) plan should automatically renew. Exceptions would be if Medicare does not renew the contract with your insurance company or the company no longer offers the plan.
Do you need to renew Part D every year?
Do I have to reenroll in my Medicare Part D prescription drug plan every year? En español | No. If you like your current Part D drug plan, you can keep it without doing anything additional. You don't have to reenroll or inform the plan that you're staying.
Does Medicare Part D expire?
If your Medicare Advantage or Part D plan is ending at the close of the year, it is important to understand how you are affected and actions you should take to ensure you have needed coverage. If your plan is ending, it should send you a letter in early October explaining that it will no longer be available next year.
How often can Medicare Part D be changed?
You can change from one Part D plan to another during the Medicare open enrollment period, which runs from October 15 to December 7 each year. During this period, you can change plans as many times as you want.
What is the initial enrollment period for Medicare Part D?
7 monthsFor people who are new to Medicare, the Initial Enrollment Period (IEP) for Part D is 7 months long. It begins 3 months prior to the month you become eligible for Medicare Part A or B, includes the month you become eligible and ends 3 months later.
How much is Medicare Part Da month?
You pay your portion of the monthly premium if you receive Part D coverage as part of Medicare. The cost varies, but the nationwide base is about $33 per month in 2022. Each plan will also have a copayment and coinsurance amount.
Why was my Medicare Part D Cancelled?
Why was my Medicare plan coverage cancelled? Your Medicare Part D prescription drug plan (PDP) or Medicare Advantage plan (MA, MAPD, or SNP) coverage can be cancelled because of changes to the Medicare plan or because of something that you have done (or not done).
What are the 4 phases of Part D coverage?
Throughout the year, your prescription drug plan costs may change depending on the coverage stage you are in. If you have a Part D plan, you move through the CMS coverage stages in this order: deductible (if applicable), initial coverage, coverage gap, and catastrophic coverage.
What is the main problem with Medicare Part D?
The real problem with Medicare Part D plans is that they weren't set up with the intent of benefiting seniors. They were set up to benefit: –Pharmacies, by having copays for generic medications that are often far more than the actual cost of most of the medications.
Is GoodRx better than Medicare Part D?
GoodRx can also help you save on over-the-counter medications and vaccines. GoodRx prices are lower than your Medicare copay. In some cases — but not all — GoodRx may offer a cheaper price than what you'd pay under Medicare. You won't reach your annual deductible.
Are all Medicare Part D plans the same?
All Medicare drug coverage must give at least a standard level of coverage set by Medicare. However, plans offer different combinations of coverage and cost sharing. Plans offering Medicare drug coverage may differ in the drugs they cover, how much you have to pay, and which pharmacies you can use.
What drugs are not covered by Medicare Part D?
Medicare does not cover:Drugs used to treat anorexia, weight loss, or weight gain. ... Fertility drugs.Drugs used for cosmetic purposes or hair growth. ... Drugs that are only for the relief of cold or cough symptoms.Drugs used to treat erectile dysfunction.More items...
When is the Medicare enrollment period?
The Medicare Annual Enrollment Period (also known as the Fall Medicare Open Enrollment Period for Medicare Advantage plans) takes place each year from October 15 to December 7. During this time, you may join, leave or switch Medicare Advantage plans or Medicare Part D plans.
How many stars does Medicare give?
Medicare rates all Medicare Advantage plans and Part D plans each year using the Medicare Star Rating system. Each plan is given a rating of one to five stars, with five stars being the highest ranking. 1. If a plan receives fewer than three stars for three consecutive years, Medicare will flag the plan as low performing.
What happens if a Medicare plan stops serving your area?
If this happens, all members of the plan will receive a notice informing them of the decision, and they will be granted a Special Enrollment Period to sign up for a different Medicare plan. The plan stops serving your area.
What is a SEP in Medicare?
Medicare Special Enrollment Period (SEP) Some Medicare beneficiaries may qualify for a Special Enrollment Period (SEP) at any time throughout the year to beneficiaries who experience a qualifying event. There are other reasons a beneficiary may qualify for a Medicare SEP.
What is the rating for Medicare Advantage?
Anyone who is enrolled in a Medicare Advantage or Medicare Part D plan with a rating of fewer than five stars is typically eligible to make changes to their Medicare coverage during the Five-Star Special Enrollment Period. 1
How long can you carry Medigap?
For 30 days , you can carry two Medigap plans: your current plan and the plan you are considering changing to. At the end of the 30 day period, you will decide which plan to keep and which one to drop. You will need to pay the plan premiums for both plans while you are enrolled in each plan.
Who sells Medicare Advantage plans?
Medicare Advantage plans, Medicare Part D plans and Medicare Supplement Insurance plans are sold by private insurance companies. The company that provides a plan may choose to no longer offer that specific plan. If this happens, plan members may be granted a Special Enrollment Period to enroll in a new Medicare plan.
When do you get a non renewal notice for Medicare?
What is a non-renewal notice? You will receive a Medicare plan non-renewal notice in October if your insurance company is not renewing its contract with Medicare. Participating health plans may not to renew their contract with Medicare if the plan lost a significant amount of revenue during the year.
When is the enrollment period for Medicare?
General enrollment period. The general enrollment period is from January 1 through March 31. During this time, you can make a change to your coverage, such as signing up for original Medicare, going from Medicare Advantage to original Medicare, or switching from one Medicare Advantage plan to another.
How long does it take to sign up for Medicare?
The initial enrollment period is the 7-month time period where you can sign up for Medicare. This includes the 3 months before your 65th birthday, the month of your birthday, and the 3 months after you turn age 65.
When is Medicare open enrollment?
Also known as Medicare open enrollment, this time period is from October 15 through December 7. This is when you can switch from original Medicare to Medicare Advantage and vice-versa.
Does Medicare Advantage automatically renew?
Medicare Advantage. Your Medicare Advantage, or Medicare Part C, plan will automatically renew unless Medicare cancels its contract with the plan or your insurance company decides not to offer the plan you’re currently enrolled in. Medicare Part D. Like Medicare Advantage, your Medicare Part D (prescription drug) plan should automatically renew. ...
Does Medicare renew at the end of the year?
Annual notice of change. Choosing a plan. Enrollment periods. Takeaway. With a few exceptions, Medicare coverage automatically renews at the end of each year. If a plan decides it will no longer contract with Medicare, your plan will not renew. There are key dates throughout the year when an insurer must notify you of coverage changes ...
Is it a good idea to shop around for Medicare?
Even if your plan hasn’t changed dramatically, it’s still a good idea to shop around. Plans can change significantly from year to year, so it’s worthwhile to spend some time comparing different Medicare plans. Sometimes, your current plan is still the best.
What Is Medicare?
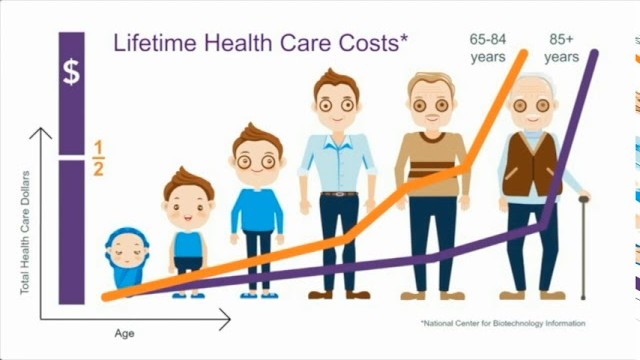
The federal Medicare program is a health insurance coverage for individuals 65 or older, disabled people and those that suffer from ESRD.
If I Have Original Medicare, Will It Renew Automatically?
Original Medicare coverage is the government’s insurance program for Part A and Part B medical expenses.
Will Medicare Advantage plans, Medicare Supplement Insurance plans, and Part D plans Automatically Renew?
Medicare Advantage plans follow the same rules for renewal and enrollment as basic Medicare (Part A and B cover).
When Might My Medicare Advantage, Supplement Insurance Plan, and Part D Plans Not Automatically Renew?
Your private Medicare policies will renew automatically each year as long as you pay your monthly premiums. But certain events can lead to your subscription not being renewed.
Will I Need to Renew My Medicare Card Each Year?
You will not have to renew your Medicare card each year. However, you will need to replace your card if it is lost, damaged, stolen, or if your details have changed.
How Can I Learn More about My Health Care?
Visit our Medicare Hub to get the latest information about Medicare, Medicare eligibility, and Medicare Advantage. You’ll be able to find in-depth guides on the next enrollment period and how you can make the most of your Medicare coverage, costs, and benefits.
What age can I renew my medicare?
In some cases, policies will renew automatically, but some require a person to confirm renewal. Medicare is a federally funded health plan for people aged 65 and older or those under age 65 with specific health conditions. ...
Why is Medicare not renewing?
The main reason either plan would not automatically renew is if the insurer does not receive payment of a monthly premium. Other exceptions can also apply.
What is Medicare Advantage?
Medicare Advantage enrollment. Private insurance companies sell Medicare Advantage plans. The plans must cover all the benefits of original Medicare. They can also include additional benefits like prescription medication, hearing, or dental care. A person must have Medicare parts A and B to enroll in Medicare Advantage.
What happens if you pay a late IEP premium?
If a person pays a monthly premium for Part A, they must enroll during the IEP. Delayed enrollment can result in a late enrollment penalty, which can see the monthly premium go up by 10%. The Part A late enrollment penalty is added to the monthly premium for twice the number of years enrollment was delayed.
How long does Medicare open?
The IEP opens for a total of 7 months. It first opens 3 months before a person’s birth month and closes 3 months after a person’s birth month. If a person does not enroll within the IEP, a penalty may be applied to the premium.
What happens if you don't enroll in Medicare?
If a person does not enroll within the IEP, a penalty may be applied to the premium. An individual can apply for Medicare through the Social Security Administration (SSA). Enrollment can be carried out online or at a local Social Security office.
How do I get a replacement Medicare card?
If the card is lost, stolen, or destroyed, a person can request a new card online, through their My Social Security account. Once logged into the Social Security account, a person can click “Replace Documents” and then “Mail my replacement Medicare Card.”.
When does Medicare Special Enrollment end?
The Special Enrollment Period for this begins one month before the effective termination date and ends two months after it.
How long does Medicare enrollment last?
Medicare treats this much like it does when a provider terminates a contract, which means you will have a Special Enrollment Period that begins two months before the coverage area reduction and lasts one month after it occurs.
What is Medicare Part A and Part B?
Original Medicare insurance, Part A and Part B, provides fee-for-service coverage through contracts with hospitals, healthcare facilities and professionals. These contracts can change throughout the year or the location or healthcare professional may not renew their certification with Medicare for the coming coverage year.
When does the special enrollment period end?
In cases where the provider will not renew for the next coverage year, your Special Enrollment Period begins in December and ends on the last day of the following February. Your Special Enrollment Period lasts for three months when your provider terminates their contract with Medicare mid-year.
How long does it take to change providers after moving?
When you inform your provider before you move, you may be given the month before the move takes place and two months afterwards to change providers. After you move, your Special Enrollment Period begins the month in which you provided notification and lasts for two more months after that. Related articles:
Does Medicare Advantage vary from state to state?
Changes to a Insurer’s Medicare Coverage Area. Private insurers who offer benefits through the Part D, Medigap and Medicare Advantage plans can vary from state to state. Coverage areas may also differ from one area to another within a state.
Does Medicare change membership?
If this happens, your Medicare membership does not change, but you may need to find a different location or healthcare professional to manage your care. Benefits can be provided by Part D Prescription Drug, Medigap or Medicare Advantage plans.
What is an annual notice of change for Medicare?
This is the Annual Notice of Change that Medicare requires plans to send to all of their enrollees. It informs you of any changes the plan will make for next year — including costs (premiums, deductibles, copays); benefits (which drugs are covered); service area; and which pharmacies can dispense drugs under this plan.
Do you have to reenroll for Part D?
You don’t have to reenroll or inform the plan that you’re staying. But be aware that all Part D plans can change their costs and coverage every calendar year. Therefore, the plan that works best for you this year won’t necessarily be your best deal next year.
How to get prescription drug coverage
Find out how to get Medicare drug coverage. Learn about Medicare drug plans (Part D), Medicare Advantage Plans, more. Get the right Medicare drug plan for you.
What Medicare Part D drug plans cover
Overview of what Medicare drug plans cover. Learn about formularies, tiers of coverage, name brand and generic drug coverage. Official Medicare site.
How Part D works with other insurance
Learn about how Medicare Part D (drug coverage) works with other coverage, like employer or union health coverage.
