Who really pays for Medicaid?
Who Really Pays For Health Care Might Surprise You
- Before Obamacare we had a free-market health-care system. Government has been part of the business of medicine at least since the 1940s, when Washington began appropriating billions to build private ...
- I fully paid for Medicare through taxes deducted from my salary. ...
- Premiums from my paycheck fund my company health plan. Probably not entirely. ...
Is Medicaid and Medicare the same thing?
The terms Medicare and Medicaid sound similar and are both government-funded health insurance programs, but the programs are not the same thing and the terms are not interchangeable. Navigating the world of health insurance is difficult enough, and with the surprisingly low amount of information available about these two systems, it’s no wonder that things can sometimes get confusing.
Does Medicaid replace Medicare?
More than 8 million people have both Medicare and Medicaid. In this situation, Medicare becomes your primary insurance and settles your medical bills first; and Medicaid become secondary, paying for services that Medicare doesn’t cover and also paying most of your out-of-pocket expenses in Medicare (premiums, deductibles and copays).
Who is eligible for Medicaid?
— The Department of Human Services (DHS) must routinely check whether recipients of public assistance are still eligible for the Supplemental Nutrition Assistance Program (SNAP) or Medicaid. — Applicants for SNAP would be required to cooperate with child support in order to qualify for the program.
What is the difference in Medicare and Medicaid?
The difference between Medicaid and Medicare is that Medicaid is managed by states and is based on income. Medicare is managed by the federal government and is mainly based on age. But there are special circumstances, like certain disabilities, that may allow younger people to get Medicare.
What are the disadvantages of Medicaid?
Disadvantages of Medicaid They will have a decreased financial ability to opt for elective treatments, and they may not be able to pay for top brand drugs or other medical aids. Another financial concern is that medical practices cannot charge a fee when Medicaid patients miss appointments.
How long can I get Medicaid?
10. How Long Will My Medicaid Benefits Last? Your benefits will last as long as you remain eligible.
Which state has best Medicaid program?
New YorkStates with the Best Medicaid Benefit ProgramsRankStateTotal Spending Per Person1New York$12,5912New Hampshire$11,5963Wisconsin$10,0904Minnesota$11,63346 more rows•Jun 16, 2020
If you qualify for both Medicare and Medicaid, you're what's known as dual eligible - and your state Medicaid program will pay your Part B premiums
Medicare provides medical coverage and benefits to people age 65 or older, or who have a qualifying disability. Medicaid is a federal and state program that helps with medical costs for some people with limited income and resources, and also offers benefits not normally covered by Medicare.
Medicaid with Medicare
The difference between Medicare and Medicaid is that Medicaid eligibility is based on income, while Medicare eligibility is based on age or disability status. Medicare coverage includes Part A (hospital care) and Part B (medical care, like physician services, durable medical equipment, and outpatient care).
Medicare and Medicaid Dual Eligibility
Some people may be eligible for Medicare due to age or disability, as well as Medicaid due to income or other state requirements. If you are eligible for both Medicare and Medicaid, you have dual eligibility. Between the two, most of your health care costs will likely be covered and you may not have to pay anything out-of-pocket.
Is Medicare or Medicaid Primary?
If you have both Medicare and Medicaid, Medicare is the primary insurer and will pay first. Medicaid will then pay second. Medicaid never pays first for services covered by Medicare. It will only pay after Medicare, employer group health plans, and/or Medicare Supplement (Medigap) insurance has paid.
Additional reading
We were unable to load Disqus. If you are a moderator please see our troubleshooting guide.
Which pays first, Medicare or Medicaid?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second.
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
What is not covered by Medicare?
Offers benefits not normally covered by Medicare, like nursing home care and personal care services
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Does Medicare cover health care?
If you have Medicare and full Medicaid coverage, most of your health care costs are likely covered.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. . If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare.
Can you get medicaid if you have too much income?
Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid. The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid. In this case, you're eligible for Medicaid because you're considered "medically needy."
Why do people need Medicare Supplement Insurance?
The main reason people consider a Medicare Supplement Insurance policy comes down to the fact that one’s Original Medicare policy may not cover all health care costs. 4 When facing deductibles and coinsurance in Original Medicare, Medicare Supplement Insurance plans can help Medicare beneficiaries cover costs where it’s needed most. Because there are a number of Medicare Supplement Insurance policies available to consumers on Original Medicare, it may be easier to find your metaphorical ‘glass slipper’ when it comes to getting additional coverage – turning your health care experience from a possible nightmare into a Cinderella story.
What is Medicare for 65?
According to the Department of Health and Human Services, Medicare is health insurance for people 65 years of age or older, certain people under 65 with disabilities, and people of any age with End-Stage Renal Disease (ESRD). 1 This federal government program has several parts, with the most frequently referenced parts being that of Original Medicare, Part A (inpatient/hospital coverage) and Part B (outpatient/medical coverage). 2
Why is it important to review your existing coverage?
As such, it’s important to review your existing coverage before making a decision to enroll in any additional coverage options. Having a comprehensive understanding of what your coverage is and what you may need more of will help you make the best decision possible for your unique situation.
Is United American a Medicare Supplement?
United American has been a prominent Medicare Supplement insurance provider since Medicare began in 1966. Additionally, we’ve been a long-standing participant in the task forces working on Medicare Supplement insurance policy recommendations for the National Association of Insurance Commissioners.
Is United American Insurance endorsed by the government?
The purpose of this communication is the solicitation of insurance. United American Insurance Company is not connected with, endorsed by, or sponsored by the U.S. government, federal Medicare program, Social Security Administration, or the Department of Health and Human Services. Policies and benefits may vary by state and have some limitations and exclusions. Individual Medicare Supplement insurance policy forms MSA10, MSB10, MSC10, MSD10, MSF10, MSHDF10, MSG10, MSHDG, MSK06R, MSL06R, MSN10 and in WI, MC4810 and MC4810HD, MC4810HDG are available from our Company where state-approved. Some states require these plans be available to persons under age 65 eligible for Medicare due to disability or End Stage Renal disease (ESRD). You may be contacted by an agent or producer representing United American Insurance Company, PO Box 8080, McKinney, TX 75070-8080. OUTLINE OF COVERAGE PROVIDED UPON REQUEST.
Does Medicare Supplement Insurance cover deductibles?
The purpose of Medicare Supplement Insurance is to cover the cost left by deductibles and coinsurance in Original Medicare, but as full Medicaid coverage should cover the majority of those costs, a Medicare Supplement Insurance policy isn’t necessary. 3.
Does Medicaid cover cost sharing?
If you are enrolled in QMB, you do not pay Medicare cost-sharing, which includes deductibles, coinsurances, and copays.
Does Medicare cover medicaid?
If you qualify for a Medicaid program, it may help pay for costs and services that Medicare does not cover.
Does Medicaid offer care coordination?
Medicaid can offer care coordination: Some states require certain Medicaid beneficiaries to enroll in Medicaid private health plans, also known as Medicaid Managed Care (MMC) plans. These plans may offer optional enrollment into a Medicare Advantage Plan designed to better coordinate Medicare and Medicaid benefits.
Does Medicare pay for home care?
Medicaid can provide secondary insurance: For services covered by Medicare and Medicaid (such as doctors’ visits, hospital care, home care, and skilled nursing facility care), Medicare is the primary payer. Medicaid is the payer of last resort, meaning it always pays last. When you visit a provider or facility that takes both forms of insurance, Medicare will pay first and Medicaid may cover your Medicare cost-sharing, including coinsurances and copays.
How old do you have to be to apply for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old.
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
What is the CMS?
The Centers for Medicare and Medicaid Services, abbreviated as CMS, oversees both the Medicare and Medicaid programs. For the Medicaid program, CMS works with state agencies to administer the program in each state, and for the Medicare program, the Social Security Administration (SSA) is the agency through which persons apply.
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
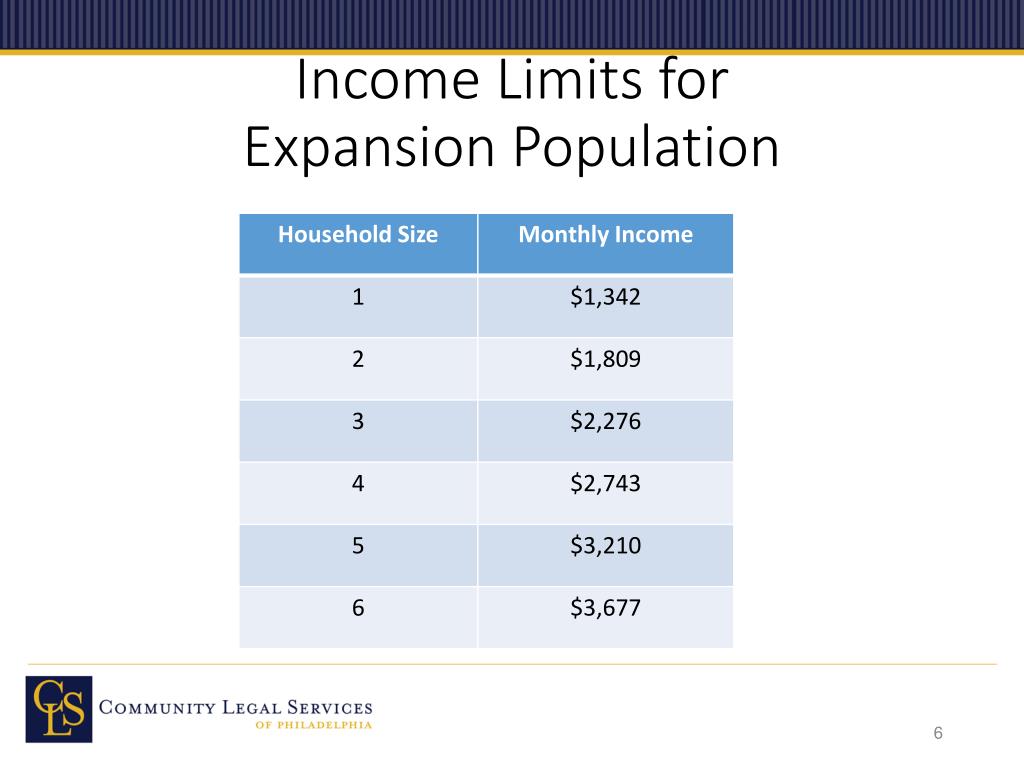
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
Is Medicare the first payer?
For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid ...
Can you be disqualified from Medicaid if you have assets?
Please note that income and assets over the Medicaid limit (s) in one’s state is not cause for automatic disqualification. This is because there are Medicaid-compliant planning strategies intended to lower one’s countable income and / or assets in order to meet the limit (s). A word of caution: It is vital that assets not be given away a minimum of 5 years (2.5 years in California) prior to the date of one’s Medicaid application. (New York is in the process of implementing a 2.5 year look back for long-term home and community based services). This is because Medicaid has a look-back period in which past transfers are reviewed to ensure an applicant (and / or an applicant’s spouse) has not gifted assets or sold them under fair market value. If this rule has been violated, it is assumed the assets were transferred in order to meet Medicaid’s asset limit and a penalty period of Medicaid disqualification will be calculated.
Qualifying For Different Types Of Coverage
Medicare is a federal insurance program that helps pay medical bills from a fund to which users have contributed. It covers people 65 and older, people younger than 65 with certain disabilities and patients with end-stage kidney disease and other conditions requiring dialysis. Participants usually pay part of the cost.
Can I Select An Insurance Plan For My Medicare And Medicaid Benefits
If you are dual eligible, you are can enroll in a dual eligible special needs plan that covers both Medicare and Medicaid benefits. These plans may also pay for expenses that Medicare and Medicaid dont over individually, including over-the-counter items, hearing aids, and vision or dental care.
If I Have Other Health Insurance Do I Need Part B
65 Incorporated came across this question from a Medicare beneficiary.
Do You Need Medicare Part B
Ever wonder if you really need Medicare Part B? For most people over 65 the answer is: Yes, you need to enroll in Part B and you should do so when first eligible. If you miss your Part B deadline, you could be subject to penalties. Check out our Medicare deadline Calculator here
Medicare Part B Enrollment And Penalties
Medicare Part B is optional, but in some ways, it can feel mandatory, because there are penalties associated with delayed enrollment. As discussed later, you dont have to enroll in Part B, particularly if youre still working when you reach age 65.
Do I Need Medicaid If I Have Medicare
Medicaid and Medicare are the two largest publicly funded health programs in the country, with different missions that often overlap. Medicare provides health coverage to seniors and some individuals with disabilities. Medicaid covers adults and children who cannot afford insurance, or who have health care costs they cannot afford.
What The Part B Late Enrollment Penalty
If you do not have creditable coverage after you first become eligible for Medicare Part B, you incur a penalty that you will pay when you eventually do enroll in Part B.
What is Medicare Extra Help?
Medicare Extra Help is a program that helps people with limited income and financial resources pay for Medicare Part D costs such as premiums, deductibles and copayments. If you qualify for both Medicaid and Medicare, you automatically qualify for Extra Help. Extra Help is also referred to as the Part D Low-Income Subsidy (LIS).
Can you get Medicare and Medicaid?
If you are eligible for both Medicare and Medicaid, you may also be eligible to join a Dual-eligible Special Needs Plan (D-SNP). This is a certain type of Medicare Advantage plan that offers all of the same coverage as Medicare Part A and Part B along with additional benefits that are tailored to the needs of someone with limited income and resources.
Can you get Medicare Part D?
Beneficiaries who are eligible for both Medicaid and Medicare can get Part D prescription drug coverage through the Medicare Extra Help program or a Medicare Special Needs Plan. We explain more about each of those programs below.
Does Medicaid work with Medicare?
Medicaid works with Medicare in several ways, and Medicaid works particularly close with Medicare Part D.
Is prescription drug coverage an optional benefit?
While prescription drug coverage is an optional Medicaid benefit (which means individual state Medicaid programs decide how drugs are covered in that state), all states in America provide Medicaid drug coverage to eligible beneficiaries.