Can you add a Medicare supplement at any time?
You can certainly apply for a new Medigap plan during the annual Medicare open enrollment period (October 15 to December 7), but that's no different from any other time of the year.
Can I change Medicare supplement plans anytime?
You can change your Medicare Supplement Plan anytime, just be aware that you might have to answer medical questions if your outside your Open Enrollment Period.
Which is true about Medicare supplement open enrollment?
Under federal law, you have a six-month open enrollment period that begins the month you are 65 or older and enrolled in Medicare Part B. During your open enrollment period, Medigap companies must sell you a policy at the best available rate regardless of your health status, and they cannot deny you coverage.
Is Medicare open enrollment only once a year?
The Medicare Open Enrollment Period is also known as the Annual Election Period (AEP) for Medicare health and prescription drug plans. It's also called the Fall Open Enrollment Period. This time period happens only once a year.Jul 6, 2021
Do you have to renew Medicare Supplement every year?
Medicare Supplement (Medigap) Plans: You do not have to do anything annually to renew them, and there is no annual open enrollment period for Medicare Supplement plans. They have the benefit of being “guaranteed renewable”. It will continue indefinitely unless you don't pay the premium.May 16, 2018
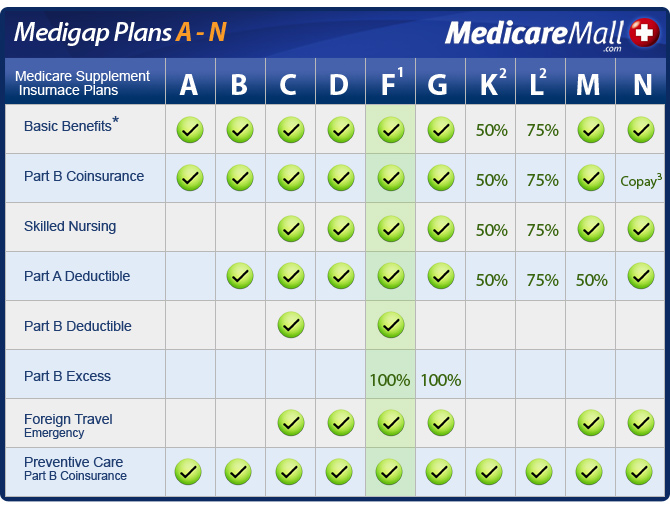
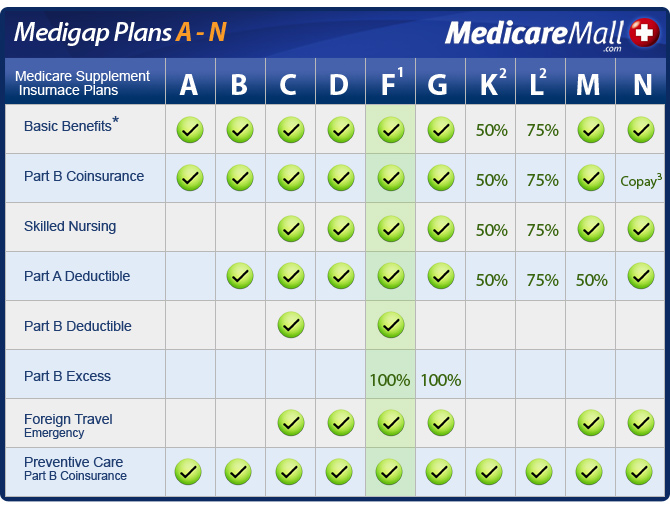
Should I switch from Plan F to Plan G?
Two Reasons to switch from Plan F to G Plan G is often considerably less expensive than Plan F. You can often save $50 a month moving from F to G. Even though you will have to pay the one time $233 for the Part B deductible on Medigap G, the monthly savings will be worth it in the long run.Sep 5, 2019
Do you really need a Medicare Supplement plan?
Original Medicare: Key takeaways For many low-income Medicare beneficiaries, there's no need for private supplemental coverage. Only 19% of Original Medicare beneficiaries have no supplemental coverage. Supplemental coverage can help prevent major expenses.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
What states are guaranteed issue for Medicare Supplement?
Only four states (CT, MA, ME, NY) require either continuous or annual guaranteed issue protections for Medigap for all beneficiaries in traditional Medicare ages 65 and older, regardless of medical history (Figure 1).Jul 11, 2018
What happens if I miss Medicare open enrollment?
If you missed your Initial Enrollment Period (IEP) and need to enroll in Medicare, you likely will have to enroll during either a Special Enrollment Period (SEP) or the General Enrollment Period (GEP).
How long before you turn 65 do you apply for Medicare?
3 monthsGenerally, you're first eligible starting 3 months before you turn 65 and ending 3 months after the month you turn 65. If you don't sign up for Part B when you're first eligible, you might have to wait to sign up and go months without coverage. You might also pay a monthly penalty for as long as you have Part B.
Does Medicare coverage start the month you turn 65?
For most people, Medicare coverage starts the first day of the month you turn 65. Some people delay enrollment and remain on an employer plan. Others may take premium-free Part A and delay Part B. If someone is on Social Security Disability for 24 months, they qualify for Medicare.
What is the open enrollment period for Medicare?
Medicare Supplement Insurance (Medigap) has a six-month open enrollment period (OEP). Your open enrollment period begins when you are both: 1 65 years old and 2 Enrolled in Medicare Part B
When does Medigap OEP start?
If you get Medicare Part B before you turn 65 , your Medigap OEP starts the first day of the month you turn 65. If you delay enrolling in Medicare Part B until after you turn 65, your Medigap OEP automatically starts the month you enroll in Medicare Part B.
How long do you have to wait to switch Medigap?
You are allowed to switch your Medigap insurance policy within your 6-month OEP. You do not have to wait for coverage to begin (although there may be a waiting period for coverage of a pre-existing condition).
What are the benefits of Medigap OEP?
Benefits of buying Medigap during open enrollment. Purchasing a Medicare Supplement Insurance policy during the Medigap OEP provides several consumer protections. During the OEP, you have the following protections: Medigap insurance companies cannot deny you coverage. Insurers cannot increase premium costs because of your health when you purchase ...
What is Medicare Supplement Open Enrollment Period?
What is Medicare Supplement Open Enrollment? Medicare Supplement Open Enrollment Period is a once in a lifetime window that allows you to enroll in any Medigap plan without answering health questions.
How long does Medicare open enrollment last?
Applying outside your open enrollment window can result in higher premiums, as well as restrict your coverage options. This window only lasts for six months for each new beneficiary, unless you delay enrollment into Part B due to having other creditable coverage.
What happens if you miss your Medigap open enrollment period?
When you miss your Medigap Open Enrollment Period and are denied coverage, there are alternative options. If you have a serious health condition that causes a Medigap carrier not to accept you, you should be able to enroll in a Medicare Advantage plan.
Why do people delay enrolling in Medicare Supplement?
For some; they choose to delay enrolling in Part B due to still working and having creditable coverage with their employer. When they do retire and enroll in Part B, they will initiate their Medicare Supplement Open Enrollment Period.
Does timing affect Medigap coverage?
Timing can affect how much you pay for coverage; how easy coverage is to obtain, and it can significantly determine the options available to you. The Megiap OEP is the only time you’ll ever get that allows you to enroll in any Medigap letter plan. You’ll be able to avoid having to answer any health questions.
Which states have open enrollment?
Some states have unique open enrollment rules, like Connecticut and California. In California, they have a birthday rule that allows you to enroll days surrounding your birthday without answering health questions. In Connecticut, they have a year-round open enrollment window for all beneficiaries.
Can you get insurance if you enroll in one time?
If they enroll as soon as their first eligible, during the one-time individual open enrollment window, these health problems will not prevent them from getting coverage.
When does Medicare open enrollment end?
The Medicare Advantage Open Enrollment Period starts January 1 and ends March 31 every year. During this period, you can switch Medicare Advantage plans or leave a Medicare Advantage plan and return to Original Medicare.
When is the best time to enroll in Medicare Supplement?
If you have Original Medicare and would like to enroll in a Medicare Supplement Insurance plan (also called Medigap), the best time to sign up is during your six-month Medigap Open Enrollment Period .
How long does Medicare initial enrollment last?
Your Initial Enrollment period lasts for seven months : It begins three months before you turn 65.
How long does Medicare last?
It includes your birth month. It extends for another three months after your birth month. If you are under 65 and qualify for Medicare due to dis ability, the 7-month period is based around your 25th month of disability benefits.
What happens if you don't sign up for Medicare?
If you don't sign up during your Initial Enrollment Period and if you aren't eligible for a Special Enrollment Period , the next time you can enroll in Medicare is during the Medicare General Enrollment Period.
How long does it take to switch back to Medicare?
If you sign up for a Medicare Advantage plan during your Initial Enrollment Period, you can change to another Medicare Advantage plan or switch back to Original Medicare within the first 3 months that you have Medicare.
Can you qualify for a special enrollment period?
Depending on your circumstances, you may also qualify for a Special Enrollment Period (SEP). Medicare Special Enrollment Periods can happen at any time during the year. You may qualify for a Special Enrollment Period for a number of reasons, which can include:
When will Medicare open enrollment start in 2022?
Medicare open enrollment for 2022 coverage starts on October 15, 2021, and continues through December 7. Learn how you can change your Medicare coverage outside of the fall open enrollment period.
What is Medicare's general enrollment period?
Medicare’s general enrollment period is for people who didn’t sign up for Medicare Part B when they were first eligible, and who don’t have access to a Medicare Part B special enrollment period. It’s also for people who have to pay a premium for Medicare Part A and didn’t enroll in Part A when they were first eligible.
How much will Medicare cost in 2021?
The standard Part B premium for 2021 is $148.50 per month. The increase in the Part B premiums was limited by the short-term government spending bill that was signed into law on October 1, 2020. The Part B premium for most enrollees was $144.60/month in 2020, and the spending bill capped the increase for 2021 at a quarter of what it would otherwise have been. Earlier in 2020, the Medicare Trustees Report had projected a Part B premiums of $153.30 per month for most enrollees in 2021. The actual price that people pay can also also be limited by the Social Security cost of living adjustment (COLA) that beneficiaries receive, but the 1.3% COLA for 2021 was adequate to allow the full standard Part B premium to be deducted from most beneficiaries’ Social Security checks.
How much is coinsurance for skilled nursing in 2021?
After the first 20 days, your skilled nursing facility coinsurance in 2021 is $185.50 per day for days 21-100 (after that, Medicare no longer covers skilled nursing facility charges, so you’ll pay the full cost). Supplemental coverage, including Medigap plans, is designed to pay the Part A coinsurance on your behalf.
What is the Medicare Advantage Plan 2021?
$7,550 is the upper limit; the average Medicare Advantage plan tends to have an out-of-pocket cap below the maximum that the government allows.
How much is Part A coinsurance for 2021?
2021 Part A coinsurance: $371 per inpatient day (days 61-90 in the benefit period for which the deductible applied; up from $352 per day in 2020) $742 per inpatient day for day 91 and beyond during the benefit period (up from $704 per day in 2020).
When does Medicare coverage take effect?
If you enroll during the general enrollment period, your coverage will take effect July 1. Learn more about Medicare’s general enrollment period. Back to top.
Can I Qualify For A New Guaranteed Issue Medicare Supplement If I Dont Like My Current One
Disliking your policy is not enough to qualify for a new guaranteed issue window. However, you can qualify for a new GI window if you show proof that your insurer either did not follow the rules or attempted to mislead you in some way. If this occurs, you can drop your policy and obtain a new policy with your guaranteed issue right.
If You Have Certain Health Issues
You cant be denied or charged more for coverage if you apply during your Medigap open enrollment period. But after that six-month period ends, insurers are allowed to collect information about your health and use it to decide whether to accept or deny your application.
How Is Pricing Calculated With A Guaranteed Issue Medicare Supplement
As previously stated, the guaranteed issue window grants you the same benefits as the open enrollment. This means that insurers must provide the best possible prices for your circumstances. That said, not every Medigap plan is priced the same way. There are three basic pricing models for Medicare supplements:
Cant Get A Medigap Policy Try Medicare Advantage
If no insurer will sell you a Medigap policy, you have an option. Medicare Advantage is another private health plan that can save you money. Plans have a maximum limit on out-of-pocket costs, typically $5,000. Some plans even have no monthly premium.
What If I Missed My Medicare Supplement Open Enrollment Period
In the past, Medicare has not been proactive about notifying people turning 65 about this Medicare Supplement Open Enrollment window. It has been, to some degree, up to each individual to research and understand this. Because of this, we encounter many people who have missed their open enrollment period.
You Do Not Check Your Annual Notice Of Change
Medicare Advantage plans and Part D plans are run by insurance companies. The federal government requires them to cover certain services. That said, they can change what other services they cover and who provides them.
You Joined An Advantage Or Programs Of All
If, during your first year of Medicare eligibility, you joined an MA or PACE plan and want to switch to Original Medicare within 12 months, you qualify for guaranteed issue under trial rights. Guidelines include:
Important Enrollment Periods
There are several enrollment periods associated with Medicare that you should familiarize yourself with. Below, we give a brief description of each to help you get the most from your Medicare coverage.
Medicare Initial Enrollment Period
If you're new to Medicare, you can sign up for Medicare Part A and Part B during your Initial Enrollment Period, which is the seven-month period that:
General Enrollment Period
If you don’t sign up for Medicare during your Initial Enrollment Period, you can sign up during the Medicare General Enrollment Period. This period runs annually from January 1 to March 31.
How to enroll in Medicare Supplement?
There are some situations when you may still be able to enroll in a Medicare Supplement insurance plan with guaranteed issue. Those situations may include, but aren’t limited to: 1 Your Medigap insurance company goes bankrupt or misled you. 2 Your Medigap coverage ends through no fault of your own. 3 You’re enrolled in Original Medicare and an employer-sponsored group plan, and your employer coverage is ending. 4 You’re enrolled in a Medicare SELECT plan (a type of Medigap plan that uses provider networks), and you move out of your plan’s service area. 5 You’re enrolled in a Medicare Advantage plan and move out of the plan’s service area, or your Medicare Advantage plan leaves the Medicare program. 6 You enrolled in a Medicare Advantage plan at age 65 when you were first eligible for Medicare Part A, but changed your mind within the first year and want to return to Original Medicare. 7 You dropped your Medigap plan to enroll in a Medicare Advantage plan for the first time, but changed your mind within the first year and want to return to Original Medicare.
What is Medicare Supplement Insurance?
That’s where Medicare Supplement insurance comes in. Also known as Medigap, Medicare Supplement insurance plans work alongside your Original Medicare coverage to help fill in some of those coverage gaps. These plans may pay for certain costs ...
How long is the Medicare Part B period?
This is the six-month period that starts on first day of the month that you are both 65 or older and enrolled in Medicare Part B. Throughout this period, you can enroll in any Medigap plan offered in your service area with guaranteed issue.
Does Medigap end?
Your Medigap coverage ends through no fault of your own. You’re enrolled in Original Medicare and an employer-sponsored group plan, and your employer coverage is ending. You’re enrolled in a Medicare SELECT plan (a type of Medigap plan that uses provider networks), and you move out of your plan’s service area.
Can you switch Medigap plans?
If you’re already enrolled in a Medigap plan, you may not be able to switch plans with guaranteed issue (except in certain situations). Without guaranteed-issue rights, you may be subject to medical underwriting and charged higher premiums based on your health status.
Can you still enroll in Medicare Supplement with guaranteed issue?
Other situations when you may have guaranteed-issue rights. There are some situations when you may still be able to enroll in a Medicare Supplement insurance plan with guaranteed issue. Those situations may include, but aren’t limited to: Your Medigap insurance company goes bankrupt or misled you.
What is a select Medicare policy?
Medicare Select. A type of Medigap policy that may require you to use hospitals and, in some cases, doctors within its network to be eligible for full benefits. . If you buy a Medicare SELECT policy, you have rights to change your mind within 12 months and switch to a standard Medigap policy.
How long does it take for a pre-existing condition to be covered by Medicare?
Coverage for the pre-existing condition can be excluded if the condition was treated or diagnosed within 6 months before the coverage starts under the Medigap policy. After this 6-month period, the Medigap policy will cover the condition that was excluded. When you get Medicare-covered services, Original Medicare.
When to buy Medigap policy?
Buy a policy when you're first eligible. The best time to buy a Medigap policy is during your 6-month Medigap Open Enrollment Period. You generally will get better prices and more choices among policies. During that time you can buy any Medigap policy sold in your state, even if you have health problems. This period automatically starts the first ...
Can you shorten the waiting period for a pre-existing condition?
It's possible to avoid or shorten waiting periods for a. pre-existing condition. A health problem you had before the date that new health coverage starts. if you buy a Medigap policy during your Medigap open enrollment period to replace ".
Can you get Medicare if you are 65?
Some states provide these rights to all people with Medicare under 65. Other states provide these rights only to people eligible for Medicare because of disability or only to people with ESRD. Check with your State Insurance Department about what rights you might have under state law.
Can you charge more for a Medigap policy?
Charge you more for a Medigap policy. In some cases, an insurance company must sell you a Medigap policy, even if you have health problems. You're guaranteed the right to buy a Medigap policy: When you're in your Medigap open enrollment period. If you have a guaranteed issue right.