When marketing UnitedHealthcare Medicare Advantage plans to consumers, which of the following must an agent do? Review and complete an SOA form with each consumer after a personal/individual (e.g., in-home or telephonic) marketing appointment. Provide current marketing materials that have been approved by CMS and UnitedHealthcare.
What are the marketing guidelines for Medicare Advantage?
May 14, 2021 · Which of the following must you not do when marketing UnitedHealthcare Medicare Advantage or Prescription Drug Plans to consumers? Which of the following must you not do when marketing UnitedHealthcare Medicare Advantage or Prescription Drug Plans to consumers? Categories English. Leave a Reply Cancel reply.
Can a consumer elect to join a different Medicare Advantage plan?
A Medicare Advantage marketing plan allows you to reach patients at all stages of the process, but it can be tricky to do effectively and ethically. Why you want more Medicare Advantage patients When patients turn 65, they have a 7-month period—three months before, during and after their birth month—to select a Medicare plan.
What are the Medicare marketing guidelines for sponsors?
Annual Election Period (AEP) is a time when: Consumers can elect to join a Medicare Advantage Plan or switch to a different plan. Dino, an agent, received a phone call on September 29 from a consumer interested in Medicare Advantage plans for the new plan year. Dino proceeded to verify the consumer's Medicare eligibility, describe the costs and benefit coverage of the plan, and …
How do private Medicare insurance companies market their plans?
As an agent, you MUST NOT do which of the following when marketing UHC Medicare Advantage plans to consumers? A) Use providers or provider groups to distribute printed information comparing benefits of different health plans without approval B) Review and complete the Enrollment Application with consumers
When must a marketing sales event be reported to UnitedHealthcare?
It needs to be reported to UnitedHealthcare prior to advertising and not less than 7 calendar days prior to the date of the event.
How Should agent Erin respond when consumer Mrs Rose notices that the presented MA plan has a star rating of 2 stars?
How should agent Erin respond when consumer Mrs. Rose notices that the presented MA Plan has a Star Rating of 2 stars? Erin should tell Mrs. Rose that the plan has received a "Below Average" rating.
In which of the following situations can telephonic contact be made with a Medicare eligible consumer quizlet?
In which of the following situations can telephonic contact be made with a Medicare eligible consumer? When the consumer consented to be contacted for sales activities, subsequent telephonic contact has not yet occurred, and that the permission has not yet expired.
Which of the following is not considered unsolicited contact with a Medicare eligible consumer according to CMS?
Which of the following is not considered unsolicited contact with a Medicare eligible consumer according to CMS regulations and UnitedHealthcare's rules, policies, and procedures? Mailing a marketing brochure to the consumer via postal mail.
When marketing UnitedHealthcare Medicare Advantage plans to consumers which of the following must an agent do?
The individual must be legally authorized in the state in which the consumer resides to act on behalf of the consumer (e.g., Power of Attorney). Advantage plans to consumers, which of the following must an agent do? Provide current marketing materials that have been approved by CMS and UnitedHealthcare.
What is the purpose of UnitedHealthcare SCO plan care management program?
Care management programs identify gaps in care for dozens of employee conditions using data from medical claims, lab results, pharmacy, biometric screenings, health assessments and more.
Which of the following must a consumer have to be eligible to enroll in UnitedHealthcare SCO?
UnitedHealthcare Senior Care Options (UnitedHealthcare SCO) is available to people who are 65 and older. You must be entitled to Medicare Part A and enrolled in Medicare Part B and MassHealth Standard to enroll in our Medicare Advantage Special Needs Plan. You also need to live in the service area.
Which activities are permitted at an Medicare educational event?
Medicare Educational event rules: advertising You are allowed to advertise educational events through most of the usual methods such as flyers, newspapers, radio, email and direct mail. When marketing them it needs to say meetings will be for “educational” purposes.Jan 7, 2021
What type of events must an agent report to UnitedHealthcare?
-Agents must report formal and informal marketing/sales events only to UnitedHealthcare.
What is considered unsolicited contact with a Medicare eligible consumer?
Unsolicited Contact: The Center for Medicare and Medicaid Services (CMS) states that agents cannot make direct unsolicited contact. This is anyone who has NOT given explicit permission to contact.Feb 28, 2019
Which of the following is considered by CMS to be a sales and marketing event?
What Does CMS Consider a Sales Event or Appointment? An activity will be considered a sales event or appointment if it is designed to persuade potential enrollees to choose a specific plan (or set of plans), according to CMS.Mar 1, 2018
What is an informal marketing sales event?
Informal marketing/sales events are conducted with a less structured presentation or in a less formal environment. They typically utilize a table, kiosk or a recreational vehicle (RV) that is manned by a plan sponsor representative who can discuss the merits of the plan's products.Oct 28, 2016
What are the Medicare marketing guidelines?
The Marketing guidelines reflect CMS' interpretation of the marketing requirements and related provisions of the Medicare Advantage and Medicare Prescription Drug Benefit rules (Chapter 42 of the Code of Federal Regulations, Parts 422 and 423).
Can Medicare Advantage and Prescription Drug Plans use one document?
The guidelines allow organizations offering both Medicare Advantage and Prescription Drug Plans the ability to reference one document when developing marketing materials.
What is Medicare Advantage Marketing Plan?
A Medicare Advantage marketing plan allows you to reach patients at all stages of the process, but it can be tricky to do effectively and ethically.
What are some examples of Medicare marketing guidelines?
For example: Events promoting a particular plan must be properly labeled as sales/marketing events rather than educational events.
How to avoid losing Medicare patients?
You can avoid losing your patients when they turn 65 by participating in the best Medicare Advantage plans, and making sure that your patients are aware they have options. Point patients to better plans.
Why do people choose Medicare Advantage?
That’s why millions of people choose a private Medicare Advantage plan as their 65th birthday approaches or during the Annual Election Period (also known as AEP or open enrollment)—to fill in those gaps and prevent a major procedure from leading to bankruptcy. A Medicare Advantage marketing plan allows you to reach patients at all stages ...
Do providers need to remain neutral about Medicare?
Providers do need to remain neutral about most aspects of choosing a Medicare plan. Still, you can and should keep patients informed of all their options and ensure they are able to make the right decisions for their health. There are plenty of ways to reach out to patients who may be considering a Medicare Advantage plan:
Can Medicare Advantage be private?
Typically, patients consider a private Medicare Advantage plan after realizing the out-of-pocket expense involved with original Medicare, which can leave patients responsible for 20% of the cost of some services with no limit on out-of-pocket expenses. So why would hospitals, medical groups, IPAs, and practices need a Medicare Advantage marketing ...
Can seniors use social media?
However, with the right plan in place, you can reach future patients through…. Remember, many seniors have family members making their healthcare decisions, so don’t rule out digital and social media advertising as a way to reach those decision-makers.
What is an AEP in Medicare?
Only the marketing/sales events, both formal and informal. Annual Election Period (AEP) is a time when: Consumers can elect to join a Medicare Advantage Plan or switch to a different plan. Dino, an agent, received a phone call on September 29 from a consumer interested in Medicare Advantage plans for the new plan year.
What is the purpose of a provider group?
Use providers or provider groups to distribute printed information comparing benefits of different health plans without approval. As an agent, you have an obligation to only enroll a consumer in a product: That is suitable for the consumer's needs, goals and financial resources.
How long does it take for a consumer to contact Bethany?
Once contact is made or 9 months from the date the consumer provided permission (e.g., consumer signature date on BRC) or 90 days if on federal do not call list, whichever comes first. Consumer Gary gives his friend's telephone number and email address to agent Bethany.
When did Dino receive a call from Medicare?
Dino, an agent, received a phone call on Sept. 29 from a consumer interested in Medicare Advantage plans for the new year. Dino proceeded to verify the consumer's Medicare eligibility, describe the costs and benefit coverage of the plan, and explained that he could not accept an enrollment application until Oct. 15.
Is Janine in a 3 star plan?
Janine, currently enrolled in a 3-star plan, discovers there is a 5-star plan available where she lives. She asks her agent, Josh, to enroll her in the 5-star plan. Josh can advise Janine of each of the following except: A) Josh should tell Janine that she can change her current plan to a 5-star plan since one is available in ...
What is a D SNP?
D-SNPs are for seniors who qualify for both Medicare and Medicaid. Since 2011, D-SNP enrollment has doubled and currently exceeds 2.2 million beneficiaries, according to MedPac. Additionally, The Gorman Health Group predicts the D-SNP market will double again, exceeding 5 million, by 2021.
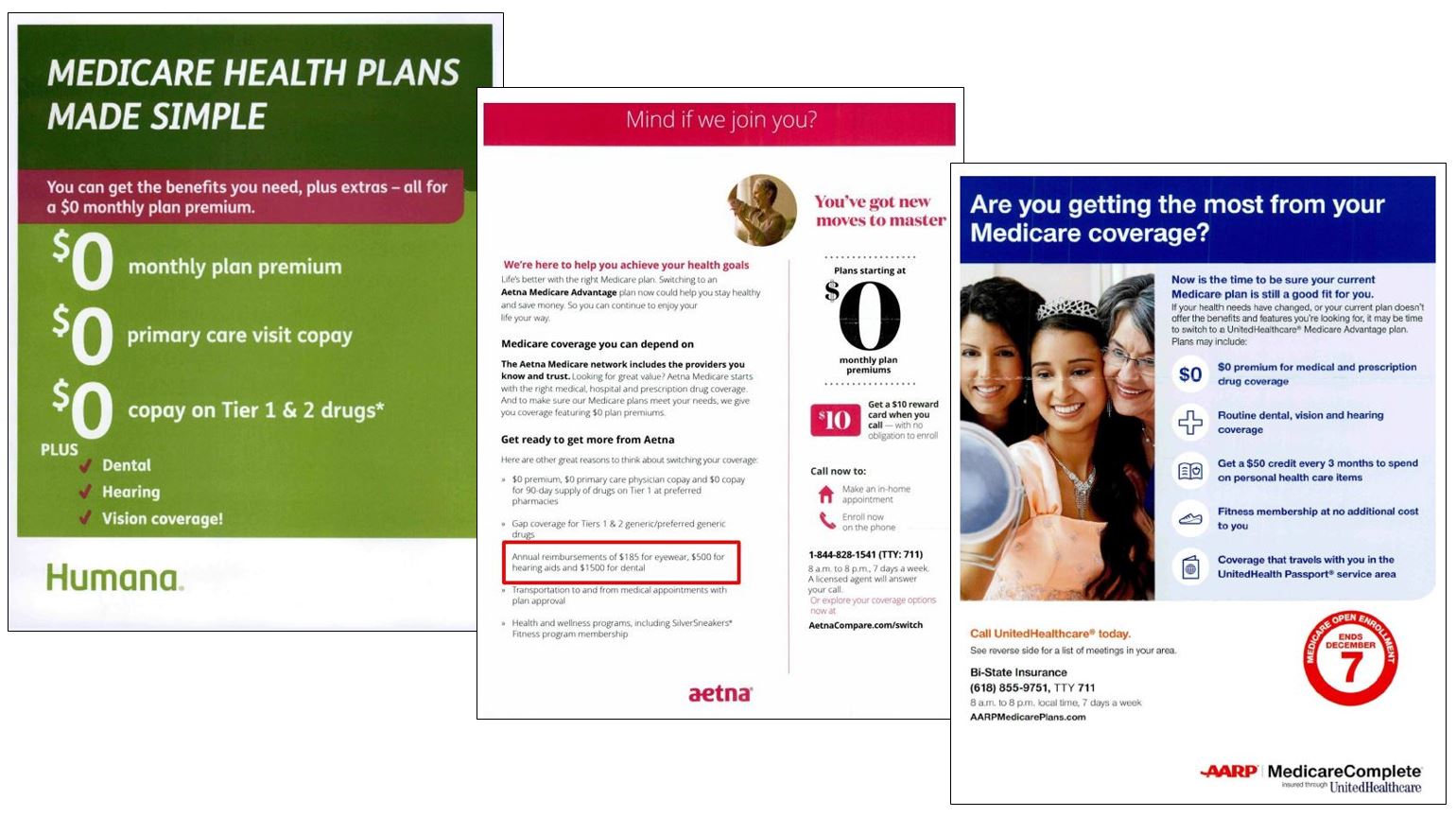
Does Humana have a Medicare card?
In the self-mailer below, Humana uses a large image of Medicare and Medicaid cards, as well as an all-caps headline which reads “Carrying these cards?”, for a simple and straightforward (and commonly used) approach, which allows recipients to self-qualify. Continuing on the back, the copy highlights the potential to get “even more benefits,” and then lists various plan benefits, starting with the $0 monthly premium, followed by aspects that are meaningful to the dual-eligible population, like “$0 for rides to your doctor,” a “monthly medication allowance,” and “dental, hearing and vision coverage.” The piece only has one call-to-action (CTA), a phone number – no BRC or URL to learn more about the plan.