What is the relationship between Medicaid and Medicare Part D?
Medicare Part D is sold by private insurance companies and provides coverage for prescription drugs. Medicaid is a publicly-funded program that provides health insurance benefits for low-income adults and children. Let’s examine the relationship between Medicaid and Medicare Part D.
What is the new rule for Medicare Advantage and Part D?
CMS is issuing a proposed rule to lower out of pocket Medicare Part D prescription drug costs and improve consumer protections, reduce disparities, and improve health equity in Medicare Advantage (MA) and Part D. An increasing number of Medicare beneficiaries receive services through MA and Part D.
Does Medicaid cover medications for Part D?
In some states, Medicaid covers additional medications for people with Part D . You will only pay a small copayment for prescriptions that are covered by Medicaid in your state. Keep in mind that all states have a Medicaid formulary.
What happens if I don't choose a part D plan?
If you have Extra Help and do not choose a Part D plan, Medicare will automatically enroll you in a benchmark Part D plan. Benchmark Part D plans have a premium below the specified amount for your state, which means that Extra Help will pay the full cost of your Part D premium.

Can Part D plans use prior authorization?
Medicare Prescription Drug (Part D) Plans very often require prior authorization to obtain coverage for certain drugs. Again, to find out plan-specific rules, contact the plan. Traditional Medicare, historically, has rarely required prior authorization.
What is the main problem with Medicare Part D?
The real problem with Medicare Part D plans is that they weren't set up with the intent of benefiting seniors. They were set up to benefit: –Pharmacies, by having copays for generic medications that are often far more than the actual cost of most of the medications.
Are there any ways to avoid the Medicare Part D donut hole?
If you find yourself paying a lot for medicines, each year, check out whether you may be eligible for several prescription savings programs. People with 'Extra Help' see significant savings on their drug plans and medications at the pharmacy, and don't fall into the donut hole.
What are the 4 phases of Medicare Part D coverage?
Throughout the year, your prescription drug plan costs may change depending on the coverage stage you are in. If you have a Part D plan, you move through the CMS coverage stages in this order: deductible (if applicable), initial coverage, coverage gap, and catastrophic coverage.
Is GoodRx better than Medicare Part D?
GoodRx can also help you save on over-the-counter medications and vaccines. GoodRx prices are lower than your Medicare copay. In some cases — but not all — GoodRx may offer a cheaper price than what you'd pay under Medicare. You won't reach your annual deductible.
Why is Medicare Part D so expensive?
Another reason some prescriptions may cost more than others under Medicare Part D is that brand-name drugs typically cost more than generic drugs. And specialty drugs used to treat certain health conditions may be especially expensive. Read more about .
What will the donut hole be in 2021?
For 2021, the coverage gap begins when the total amount your plan has paid for your drugs reaches $4,130 (up from $4,020 in 2020). At that point, you're in the doughnut hole, where you'll now receive a 75% discount on both brand-name and generic drugs.
Is Medicare going to do away with the donut hole?
The Part D coverage gap (or "donut hole") officially closed in 2020, but that doesn't mean people won't pay anything once they pass the Initial Coverage Period spending threshold. See what your clients, the drug plans, and government will pay in each spending phase of Part D.
What will the donut hole be in 2022?
In 2022, the coverage gap ends once you have spent $7,050 in total out-of-pocket drug costs. Once you've reached that amount, you'll pay the greater of $3.95 or 5% coinsurance for generic drugs, and the greater of $9.85 or 5% coinsurance for all other drugs. There is no upper limit in this stage.
How do Medicare Part D plans work?
You pay a monthly premium to an insurance carrier for your Part D plan. In return, you use the insurance carrier's network of pharmacies to purchase your prescription medications. Instead of paying full price, you will pay a copay or percentage of the drug's cost. The insurance company will pay the rest.
What is the max out-of-pocket for Medicare Part D?
The out-of-pocket spending threshold is increasing from $6,550 to $7,050 (equivalent to $10,690 in total drug spending in 2022, up from $10,048 in 2021).
What are two options for Medicare consumers to get Part D prescription drug coverage assuming they meet all eligibility requirements )? Select 2?
There is no other way a Medicare consumer could get Part D prescription drug coverage. They could enroll in a Medicare Supplement Insurance Plan. They could enroll in a Medicare Advantage Plan or other Medicare health plan that includes prescription drug coverage.
What drugs are excluded from Medicare?
Drugs excluded from Medicare coverage by law that may be covered by your state’s Medicaid program include: Drugs for: Anorexia, weight loss, or weight gain. Fertility. Cosmetic purposes or hair growth. Relief of cold symptoms (like a cough or stuffy nose)
Do you have to pay a copayment for medicaid?
You will only pay a small copayment for prescriptions that are covered by Medicaid in your state. Keep in mind that all states have a Medicaid formulary. For more information on the Medicaid formulary in your state, ask your pharmacist or contact your local Medicaid office.
Does Medicare cover extra help?
If you have Medicare and Medicaid (dually eligible), your drugs are usually covered by Part D and Extra Help. In cases like those described below, Medicaid may cover drugs that Medicare does not. In many states, Medicaid covers some of the drugs that are excluded from Medicare coverage by law.
Does medicaid cover fluoride?
Relief of cold symptoms (like a cough or stuffy nose) Prescription vitamins and minerals (except prenatal vitamins and fluoride preparations) In some states, Medicaid covers additional medications for people with Part D . You will only pay a small copayment for prescriptions that are covered by Medicaid in your state.
What is the Medicare and Medicaid program?
Another Medicare and Medicaid program is PACE, or Programs of All-Inclusive Care for the Elderly. PACE helps older Medicare beneficiaries to seek health care within their community, in their home and at PACE facilities. Some of the things that can be covered by PACE include: Adult day primary care. Dental care.
How old do you have to be to get medicaid?
Be at least 65 years old or having a qualifying disability. Be a U.S. citizen or permanent legal resident. Be eligible for benefits through Social Security or the Railroad Retirement Board. Generally speaking, Medicaid provides health insurance to low-income individuals and families, children and pregnant women.
What is partial dual eligibility?
Partial dual eligibility includes those who receive assistance from Medicaid in order to help pay for Medicare costs such as premiums, coinsurance or deductibles. Partial dual eligibles fall into one of four categories of eligibility for Medicare Savings Programs.
What is QMB in Medicare?
Qualified Medicare Beneficiary (QMB) Program. This program helps pay for Medicare Part A and Part B premiums, deductibles, coinsurance and copayments. Eligibility requires: Income of no more than $1,061 per month for an individual in 2019, or $1,430 per month for a married couple.
What is a special needs plan?
A Medicare special needs plan is a certain type of Medicare Advantage plan that is designed for people with specific health conditions or circumstances. A D-SNP is built for the specific needs of dual eligibles. All Medicare SNPs (including Medicare D-SNPs) provide prescription drug coverage.
What is dual eligible?
Full dual eligible refers to those who receive full Medicaid benefits and are also enrolled in Medicare. People who are full dual eligible typically receive Supplemental Security Income (SSI) benefits, which provide cash assistance for basic food ...
What is a dual SNP?
If you are Medicare dual eligible, you may qualify for a Medicare D-SNP (Dual Special Needs Plan), which is a type of Medicare Advantage plan. 61.9 million Americans are Medicare beneficiaries. 1 In 2019, more than 12 million Americans were dually eligible for Medicare and Medicaid and are enrolled in both programs. 2.
How to get prescription drug coverage
Find out how to get Medicare drug coverage. Learn about Medicare drug plans (Part D), Medicare Advantage Plans, more. Get the right Medicare drug plan for you.
What Medicare Part D drug plans cover
Overview of what Medicare drug plans cover. Learn about formularies, tiers of coverage, name brand and generic drug coverage. Official Medicare site.
How Part D works with other insurance
Learn about how Medicare Part D (drug coverage) works with other coverage, like employer or union health coverage.
What is a copayment for Medicare?
A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor's visit or prescription drug. for each drug. If you don't join a drug plan, Medicare will enroll you in one to make sure you don't miss a day of coverage.
What is Medicare program?
A Medicare program to help people with limited income and resources pay Medicare prescription drug program costs , like premiums, deductibles, and coinsurance. with your prescription drug costs. If you don't join a plan, Medicare will enroll you in one to make sure you don't miss a day of coverage.
Do you have to have a Medicare drug plan to get tricare?
Most people with TRICARE entitled to Part A must have Part B to keep TRICARE drug benefits. If you have TRICARE, you don’t need to join a Medicare drug plan.
Can you keep a medicaid policy?
Medigap policies can no longer be sold with prescription drug coverage, but if you have drug coverage under a current Medigap policy, you can keep it. If you join a Medicare drug plan, your Medigap insurance company must remove the prescription drug coverage under your Medigap policy and adjust your premiums.
Can you join a Medicare plan without a penalty?
, you'll have a special enrollment period to join a Medicare drug plan without a penalty when COBRA ends.
Does Medicare help with housing?
, you won't lose your housing assistance. However, your housing assistance may be reduced as your prescription drug spending decreases.
Does Medicare pay for prescription drugs?
Your drug costs are covered by Medicare. You'll need to join a Medicare drug plan for Medicare to pay for your drugs. In most cases, you'll pay a small amount for your covered drugs. If you have full coverage from Medicaid and live in a nursing home, you pay nothing for covered prescription drugs.
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
What is dual eligible?
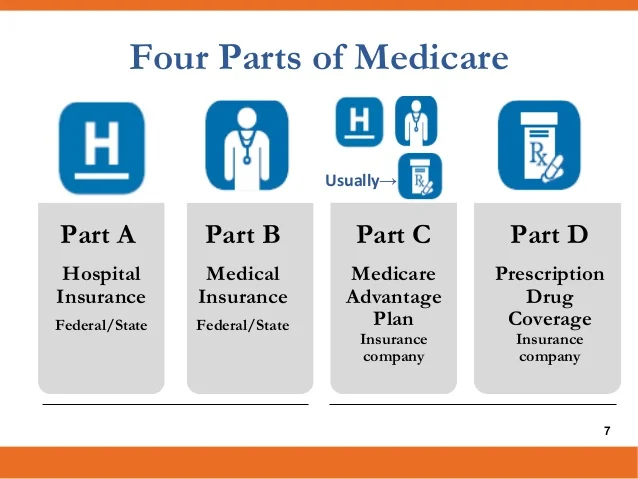
Definition: Dual Eligible. To be considered dually eligible, persons must be enrolled in Medicare Part A, which is hospital insurance, and / or Medicare Part B, which is medical insurance. As an alternative to Original Medicare (Part A and Part B), persons may opt for Medicare Part C, which is also known as Medicare Advantage.
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
How old do you have to be to qualify for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old. For persons who are disabled or have been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis), there is no age requirement. Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
How to apply for medicaid?
How to Apply. To apply for Medicare, contact your local Social Security Administration (SSA) office. To apply for Medicaid, contact your state’s Medicaid agency. Learn about the long-term care Medicaid application process. Prior to applying, one may wish to take a non-binding Medicaid eligibility test.
Does Medicare cover out-of-pocket expenses?
Persons who are enrolled in both Medicaid and Medicare may receive greater healthcare coverage and have lower out-of-pocket costs. For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses. Medicaid does cover some expenses that Medicare does not, such as personal care assistance in the home and community and long-term skilled nursing home care (Medicare limits nursing home care to 100 days). The one exception, as mentioned above, is that some Medicare Advantage plans cover the cost of some long term care services and supports. Medicaid, via Medicare Savings Programs, also helps to cover the costs of Medicare premiums, deductibles, and co-payments.
How long does it take for Medicare to start Part D?
In either case, your Part D coverage should begin within two months of your enrollment in Extra Help. During that period, Medicare may enroll you in the Limited Income Newly Eligible Transition (LI NET) program to give you temporary coverage.
What is benchmark Medicare?
Benchmark Part D plans have a premium below the specified amount for your state, which means that Extra Help will pay the full cost of your Part D premium. Medicare will send you a notice telling you which plan it enrolled you in and what your costs are.
What do you need to know before enrolling in a Part D plan?
The most important preparation you can do before finding a Part D plan is recording information about your medications.
When is the best time to sign up for Part D?
If you don’t have creditable drug coverage or health insurance from a current employer, the best time to sign up for Part D is during your 7-month initial enrollment period (IEP) to avoid penalties. Under your IEP, you have a 7-month window that opens 3 months before you turn 65 and closes at the end of the 3rd month following your birthday month.
How long does an open enrollment period last?
Typically a SEP lasts for 63 days.
How does dosage affect Part D?
Your dosage can affect your final cost or enact certain plan restrictions depending on the Part D plan. The frequency of the medication. The number of pills you take also affects the cost, so double check how often you take your medication and write it down. Once you have these recorded, you’ll be able to compare plans, apples-to-apples.
Is Medicare Part D a good program?
Although Medicare is not without its faults, one thing is clear: Medicare Part D has been a successful program. With nearly 70% of all beneficiaries enrolled in Part D, this optional add-on to Original Medicare is a popular way to lower drug costs. 1. But before diving into the deep end of Part D plans, you’ll want to perform due diligence ...