In order to purchase a Medicare Supplement
Medigap
Medigap refers to various private health insurance plans sold to supplement Medicare in the United States. Medigap insurance provides coverage for many of the co-pays and some of the co-insurance related to Medicare-covered hospital, skilled nursing facility, home health care, ambulance, durable medical equipment, and doctor charges. Medigap's name is derived from the notion that it exists to …
When can I enroll in a Medicare supplement plan?
When can I enroll in a Medicare Supplement Plan? When newly eligible for Medicare, you enter a seven-month Initial Enrollment Period (IEP) which begins three months before your 65th birthday and ends three months after the month of your birthday.
Do you need Medicare supplement insurance (Medigap)?
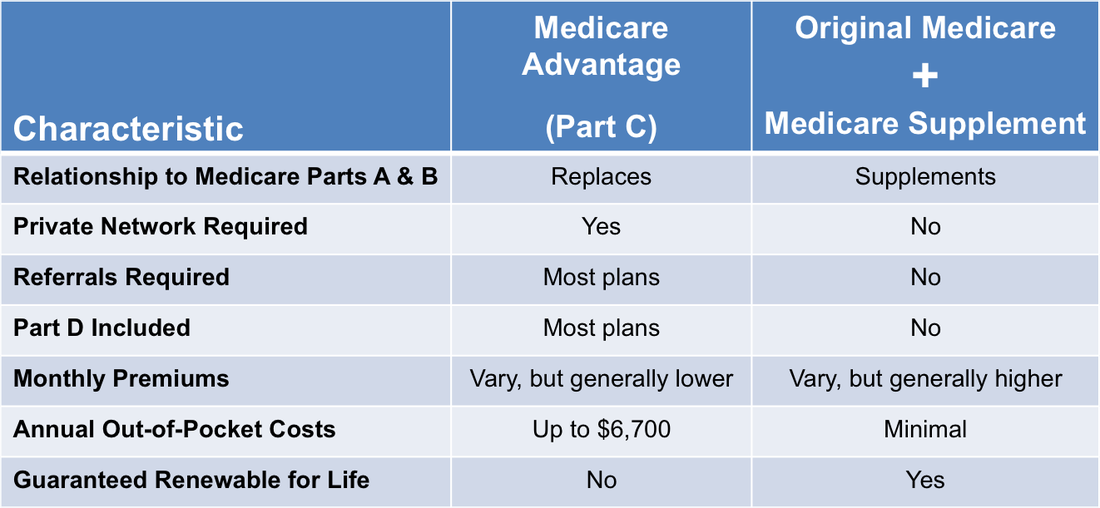
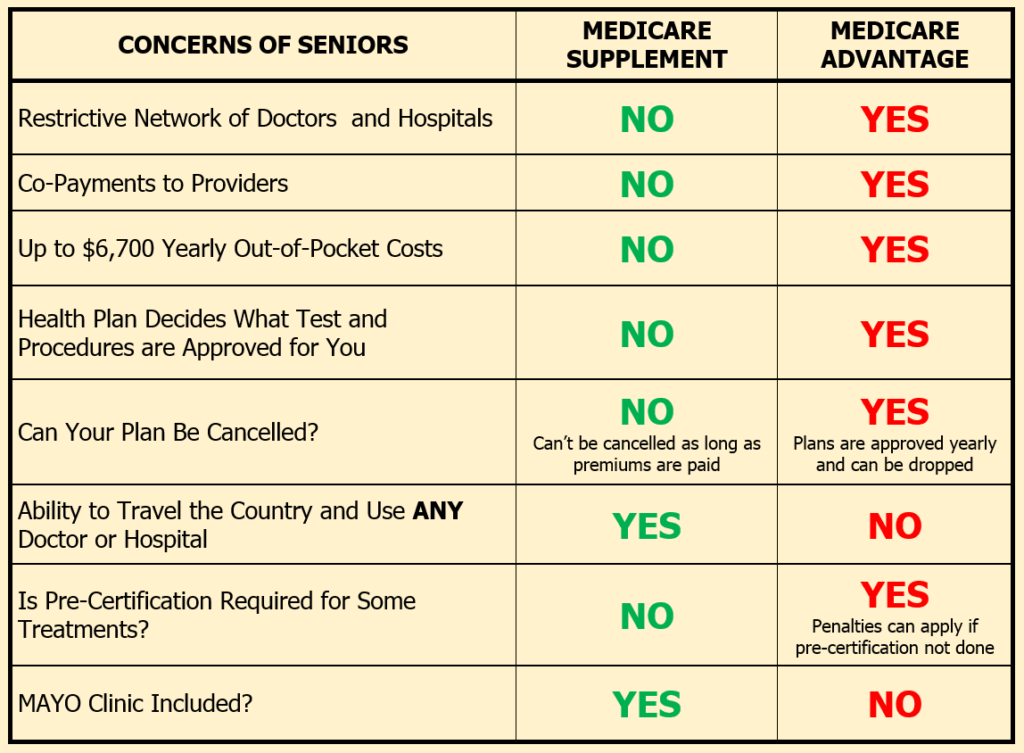
Some people need to get additional coverage, like Medicare drug coverage or Medicare Supplement Insurance (Medigap). Use this information to help you compare your coverage options and decide what coverage is right for you. Original Medicare includes Medicare Part A (Hospital Insurance) and Part B (Medical Insurance).
What are supplemental insurance plans for Medicare?
Supplement insurance plans are sold by some private insurance providers in the United States. Not all companies have them, or sell all available plans, so you may have to look for one in your area. These plans help Original Medicare beneficiaries pay for some of the out-of-pocket health care costs left unpaid by Medicare.
Can I buy or Change my Medicare supplement plan outside of enrollment?
At the end of the trial, you choose the one plan that is right for your needs. You may be able to buy or change your Medicare Supplement Plan outside of your six-month Medigap Open Enrollment Period, if you have a “guaranteed issue right” – meaning an insurance company can’t refuse to sell you a Medigap policy – in the following situations:
What is the deadline to choose Medicare plan?
When you first become eligible for Medicare, you can join a plan. Open Enrollment Period. From October 15 – December 7 each year, you can join, switch, or drop a plan. Your coverage will begin on January 1 (as long as the plan gets your request by December 7).
Can you change Medicare Supplement plans anytime you want?
As a Medicare beneficiary, you can change supplements at any time. As a result, there's no guarantee an application will be accepted if switched outside the designated Open Enrollment Period. An application may be “medically underwritten”.
When can someone enroll in a Medicare Supplement without the chance for denial premium increase or exclusions due to pre existing conditions?
six monthsOpen Enrollment You have six months to sign up for a plan. Insurance companies cannot deny coverage or charge more for a pre-existing condition during your open enrollment period.
Is it too late to get a Medicare Supplement plan?
If you are under 65 and have Medicare, you can apply for a Medicare Supplement plan at any time. However, in order to be eligible for Medicare when are you are under 65, you generally must have a disability or serious health condition.
Do you have to renew Medicare Supplement every year?
Medicare Supplement (Medigap) Plans: You do not have to do anything annually to renew them, and there is no annual open enrollment period for Medicare Supplement plans. They have the benefit of being “guaranteed renewable”. It will continue indefinitely unless you don't pay the premium.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
What pre-existing conditions are not covered?
Health insurers can no longer charge more or deny coverage to you or your child because of a pre-existing health condition like asthma, diabetes, or cancer, as well as pregnancy. They cannot limit benefits for that condition either.
Is it necessary to have supplemental insurance with Medicare?
For many low-income Medicare beneficiaries, there's no need for private supplemental coverage. Only 19% of Original Medicare beneficiaries have no supplemental coverage. Supplemental coverage can help prevent major expenses.
How long can an insurer exclude coverage for a pre-existing condition on a Medicare Supplement?
within 6 monthsCoverage for the pre-existing condition can be excluded if the condition was treated or diagnosed within 6 months before the coverage starts under the Medigap policy. After this 6-month period, the Medigap policy will cover the condition that was excluded.
Can I switch from Medicare Advantage to Medicare Supplement?
Once you've left your Medicare Advantage plan and enrolled in Original Medicare, you are generally eligible to apply for a Medicare Supplement insurance plan. Note, however, that in most cases, when you switch from Medicare Advantage to Original Medicare, you lose your “guaranteed-issue” rights for Medigap.
What is the best supplemental insurance for Medicare?
Best Medicare Supplement Insurance Companies of 2022Best Overall: Mutual of Omaha.Best User Experience: Humana.Best Set Pricing: AARP.Best Medigap Coverage Information: Aetna.Best Discounts for Multiple Policyholders: Cigna.
Can Medigap insurance be denied for pre-existing conditions?
Be aware that under federal law, Medigap policy insurers can refuse to cover your prior medical conditions for the first six months. A prior or pre-existing condition is a condition or illness you were diagnosed with or were treated for before new health care coverage began.