Can you add a Medicare supplement at any time?
You can certainly apply for a new Medigap plan during the annual Medicare open enrollment period (October 15 to December 7), but that's no different from any other time of the year.
What is the open enrollment period for Medicare Supplements?
Under federal law, you have a six-month open enrollment period that begins the month you are 65 or older and enrolled in Medicare Part B. During your open enrollment period, Medigap companies must sell you a policy at the best available rate regardless of your health status, and they cannot deny you coverage.
Can a Medicare supplement plan be purchased at any time of the year?
If you're in good health and comfortable answering medical questions, you can apply to change Medigap plans at any time of the year. Medicare Advantage plans and Medicare Part D prescription drug plans can only be changed during certain times of year, but Medicare supplements are different.Jan 26, 2021
Is it too late to get supplemental insurance?
The best time to buy a Medigap policy is the 6-month period that starts the first day of the month you're 65 or older and enrolled in Part B. For example, if you turn 65 and are enrolled in Part B in June, the best time for you to buy a Medigap policy is from June to November.
Does Medicare coverage start the month you turn 65?
For most people, Medicare coverage starts the first day of the month you turn 65. Some people delay enrollment and remain on an employer plan. Others may take premium-free Part A and delay Part B. If someone is on Social Security Disability for 24 months, they qualify for Medicare.
What are the four prescription drug coverage stages?
Throughout the year, your prescription drug plan costs may change depending on the coverage stage you are in. If you have a Part D plan, you move through the CMS coverage stages in this order: deductible (if applicable), initial coverage, coverage gap, and catastrophic coverage.Oct 1, 2021
When can I change my Medicare Supplement plan for 2022?
Yes, at any time you can switch from a Medicare Advantage to a Medicare Supplement plan. You have 12 months from when you first enrolled in an Advantage plan to switch back to Original Medicare and pick up a Medigap plan with Guaranteed Issue.
How long before you turn 65 do you apply for Medicare?
3 monthsGenerally, you're first eligible starting 3 months before you turn 65 and ending 3 months after the month you turn 65. If you don't sign up for Part B when you're first eligible, you might have to wait to sign up and go months without coverage. You might also pay a monthly penalty for as long as you have Part B.
Do you have to renew Medicare Supplement every year?
Medicare Supplement (Medigap) Plans: You do not have to do anything annually to renew them, and there is no annual open enrollment period for Medicare Supplement plans. They have the benefit of being “guaranteed renewable”. It will continue indefinitely unless you don't pay the premium.May 16, 2018
How long does it take to get Medicare Part B after?
Most Medicare provider number applications are taking up to 12 calendar days to process from the date we get your application. Some applications may take longer if they need to be assessed by the Department of Health. We assess your application to see if you're eligible to access Medicare benefits.Dec 10, 2021
Is Medigap the same as supplemental?
Are Medigap and Medicare Supplemental Insurance the same thing? En español | Yes. Medigap or Medicare Supplemental Insurance is private health insurance that supplements your Medicare coverage by helping you pay your share of health care costs. You have to buy and pay for Medigap on your own.
Do you really need a Medicare Supplement plan?
Original Medicare: Key takeaways For many low-income Medicare beneficiaries, there's no need for private supplemental coverage. Only 19% of Original Medicare beneficiaries have no supplemental coverage. Supplemental coverage can help prevent major expenses.
When Am I Eligible For Medicare Supplement Coverage?
Because Medicare Supplement policies complement your Original Medicare coverage, you must be enrolled in Part A and Part B to be eligible for this...
How Can Enrollment Periods Affect My Eligibility For Medicare Supplement Plans?
The best time to enroll in a Medicare Supplement plan is generally during your Medicare Supplement Open Enrollment Period—for most people, this per...
Am I Eligible For A Medicare Supplement Plan If I’M Under Age 65?
Federal law does not require insurance companies to sell Medicare Supplement policies to people under 65, but many states do have this requirement....
Am I Eligible For A Medicare Supplement Plan If I Have A Medicare Advantage Plan?
Medicare Supplement policies don’t work with Medicare Advantage plans. If you decide to switch from Original Medicare to a Medicare Advantage plan,...
Am I Eligible For A Medicare Supplement Plan If I Have Coverage Through Medicaid?
While some beneficiaries may be eligible for both Medicare and Medicaid benefits (also known as “dual eligibles”), Medicaid typically doesn’t work...
What is a select Medicare policy?
Medicare Select. A type of Medigap policy that may require you to use hospitals and, in some cases, doctors within its network to be eligible for full benefits. . If you buy a Medicare SELECT policy, you have rights to change your mind within 12 months and switch to a standard Medigap policy.
When to buy Medigap policy?
Buy a policy when you're first eligible. The best time to buy a Medigap policy is during your 6-month Medigap Open Enrollment Period. You generally will get better prices and more choices among policies. During that time you can buy any Medigap policy sold in your state, even if you have health problems. This period automatically starts the first ...
How long does it take for a pre-existing condition to be covered by Medicare?
Coverage for the pre-existing condition can be excluded if the condition was treated or diagnosed within 6 months before the coverage starts under the Medigap policy. After this 6-month period, the Medigap policy will cover the condition that was excluded. When you get Medicare-covered services, Original Medicare.
What is a copayment?
A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor's visit or prescription drug. .
Can you charge more for a Medigap policy?
Charge you more for a Medigap policy. In some cases, an insurance company must sell you a Medigap policy, even if you have health problems. You're guaranteed the right to buy a Medigap policy: When you're in your Medigap open enrollment period. If you have a guaranteed issue right.
Can Medigap refuse to cover out-of-pocket costs?
A health problem you had before the date that new health coverage starts. . In some cases, the Medigap insurance company can refuse to cover your. out-of-pocket costs. Health or prescription drug costs that you must pay on your own because they aren’t covered by Medicare or other insurance.
Can you shorten the waiting period for a pre-existing condition?
It's possible to avoid or shorten waiting periods for a. pre-existing condition. A health problem you had before the date that new health coverage starts. if you buy a Medigap policy during your Medigap open enrollment period to replace ".
How long does Medicare Supplement open enrollment last?
How can enrollment periods affect my eligibility for Medicare Supplement plans? The best time to enroll in a Medicare Supplement plan is generally during your Medicare Supplement Open Enrollment Period —for most people, this period starts the month that you turn 65 and have Medicare Part B, and goes for six months.
How long do you have to wait to get Medicare Supplement?
Keep in mind that even though a Medicare Supplement insurance company cannot reject your enrollment for health reasons, the company is allowed to make you wait up to six months before covering your pre-existing conditions.
How long is a trial period for Medicare Advantage?
Trial rights allow you to join a Medicare Advantage plan for a one-year trial period if you are enrolling in Medicare Part C for the first time. If you’re not happy with the plan, you can return to Original Medicare anytime within the first 12 months.
Can you use Medicare Supplement Plan with Medicare Supplement?
While some beneficiaries may be eligible for both Medicare and Medicaid benefits (also known as “dual eligibles”), Medicaid typically doesn’t work with Medicare Supplement plans. You can only use your Medicare Supplement plan to pay for costs in Original Medicare.
Can you change your Medicare Supplement plan if it goes bankrupt?
For example, if your Medicare Supplement insurance company goes bankrupt or misleads you, you may be able to change Medicare Supplement plans with guaranteed issue.
Can you get Medicare Supplement if you have health issues?
This is when you can get any Medicare Supplement plan that’s available in your area, regardless of any health issues you may have. The insurance company can’t charge you more if you have health problems or deny you coverage because of pre-existing conditions.
Does Medigap cover prescriptions?
Since Medigap plans don’t include prescription drug benefits, if you’re enrolled in Original Medicare and want help with prescription drug costs, you can get this coverage by enrolling in a stand-alone Medicare Prescription Drug Plan.
How long does Medicare Part D coverage last?
Medicare Part D prescription drug coverage has the same initial enrollment period of the seven months around your 65th birthday as Medicare parts A and B, but the penalty is different. The late enrollment penalty is applied if you go 63 or more days without credible prescription drug coverage after becoming eligible for Medicare. The penalty is calculated by multiplying 1% of the "national base beneficiary premium" ($32.74 in 2020) by the number of months you didn't have prescription drug coverage after Medicare eligibility and rounding to the nearest 10 cents. This amount is added to the Medicare Part D plan you select each year. And as the national base beneficiary premium increases, your penalty also grows.
What is Medicare Supplement Insurance?
Medicare Supplement Insurance plans can be used to pay for some of Medicare's cost-sharing requirements and sometimes services traditional Medicare doesn't cover. The Medicare Supplement Insurance plans' enrollment period is different than the other parts of Medicare. It's a six-month period that begins when you are 65 or older and enrolled in Medicare Part B. During this open enrollment period, private health insurance companies are required by the government to sell you a Medicare Supplement Insurance plan regardless of health conditions.
How to enroll in Medicare Supplement?
The Medicare enrollment period is: 1 You can initially enroll in Medicare during the seven-month period that begins three months before you turn age 65. 2 If you continue to work past age 65, sign up for Medicare within eight months of leaving the job or group health plan to avoid penalties. 3 The six-month Medicare Supplement Insurance enrollment period begins when you are 65 or older and enrolled in Medicare Part B. 4 You can make changes to your Medicare coverage during the annual open enrollment period, from Oct. 15 to Dec. 7. 5 Medicare Advantage Plan participants can switch plans from Jan. 1 to March 31 each year.
How much is the late enrollment penalty for Medicare?
The late enrollment penalty is applied if you go 63 or more days without credible prescription drug coverage after becoming eligible for Medicare. The penalty is calculated by multiplying 1% of the "national base beneficiary premium" ($32.74 in 2020) by the number of months you didn't have prescription drug coverage after Medicare eligibility ...
What happens if you don't sign up for Medicare?
If you don't sign up for Medicare during this initial enrollment period, you could be charged a late enrollment penalty for as long as you have Medicare. The Medicare enrollment period is: You can initially enroll in Medicare during the seven-month period that begins three months before you turn age 65. If you continue to work past age 65, sign up ...
How long does it take to get Medicare if you are 65?
If you continue to work past age 65, sign up for Medicare within eight months of leaving the job or group health plan to avoid penalties. The six-month Medicare Supplement Insurance enrollment period begins when you are 65 or older and enrolled in Medicare Part B. You can make changes to your Medicare coverage during the annual open enrollment ...
When can I sign up for Medicare if I don't have Medicare?
If you don't enroll in Medicare during the initial enrollment period around your 65th birthday, you can sign up during the general enrollment period between Jan. 1 and March 31 each year for coverage that will begin July 1. However, you could be charged a late enrollment penalty when your benefit starts. Monthly Part B premiums increase by 10% ...
How long does it take to apply for Medicare Supplement?
When to apply for a Medicare Supplement plan. Here's the quick answer: Most people should apply for a Medigap plan within six months of signing up for Part B. Medigap open enrollment begins when you sign up for Medicare Part B (at age 65) and lasts for six months. If you defer Part B coverage past age 65 because of health coverage ...
Can you keep Medicare and Medigap together?
Be sure to keep your Medicare and Medigap cards together in a safe place. Your Medigap plan will be guaranteed renewable if you apply within your window of guaranteed issue rights. Guaranteed renewable means that as long as you continue to pay your premiums, you’ll keep your plan for as long as you’d like.
Does Medigap guarantee issue rights?
As you can see, Medigap guaranteed issue rights are incredibly valuable. Outside your open enrollment period, there are a few other scenarios where you have these rights as well. Typically these situations apply to you when you lose your existing coverage or after you try out Medicare Advantage.
Who is Alex Enabnit?
Alex Enabnit. Licensed Insurance Agent and Medicare Expert Writer. December 12, 2019. Medicare can cover a wide range of medical costs, but like anything else, it’s not perfect. We would all like a bit more coverage than Original Medicare can offer, especially when we know we'll be in more need of the benefits later in life.
Is eligibility.com a Medicare provider?
Eligibility.com is a DBA of Clear Link Technologies, LLC and is not affiliated with any Medicare System Providers.
What is the phone number for Medicare Supplement?
Call UnitedHealthcare at 1-866-408-5545 (TTY 711) , weekdays, 7 a.m. to 11 p.m., and Saturday, 9 a.m. to 5 p.m., Eastern Time.
What does OEP mean for Medicare?
During this six-month OEP, you are guaranteed acceptance – meaning you have a right to buy any Medicare supplement plan sold in your state. There may be other situations in which you may be guaranteed acceptance. For example, if you’ve delayed retirement and are enrolling in Medicare beyond your 65th birthday, or if coverage from another Medicare ...
When is the best time to buy a Medicare Supplement Plan?
The best time to buy a Medicare Supplement plan is during your six-month Medigap Open Enrollment Period (OEP). This starts the first day of the month in which you are age 65 or older and enrolled in Part B. During this six-month OEP, you are guaranteed acceptance – meaning you have a right to buy any Medicare supplement plan sold in your state.
Does AARP pay royalty fees?
AARP endorses the AARP Medicare Supplement Insurance Plans, insured by UnitedHealthcare Insurance Company. UnitedHealthcare Insurance Company pays royalty fees to AARP for the use of its intellectual property. These fees are used for the general purposes of AARP. AARP and its affiliates are not insurers. AARP does not employ or endorse agents, ...
Is AARP an insurer?
These fees are used for the general purposes of AARP. AARP and its affiliates are not in surers. AARP does not employ or endorse agents, brokers or producers. You must be an AARP member to enroll in an AARP Medicare Supplement Plan.
What should my carrier agent do?
Once you have selected a carrier, your agent should help you with when to apply. If you are in your open enrollment window or a guaranteed issue window, an agent can help you submit an application that is guaranteed to be accepted. Your agent will be able to show you entire sections of the application that you can skip.
Is it easier to get Medicare supplement?
Applying for a Medicare supplement is easier than you think. While applying for Medigap may seem overwhelming at first, there are a few simple steps you can follow. This will ensure that you apply for the right Medigap policy for you. It will also help you have the best chance to get approved. Here are our suggestions:
How does Medicare work with my job-based health insurance when I stop working?
Once you stop working, Medicare will pay first and any retiree coverage or supplemental coverage that works with Medicare will pay second.
When & how do I sign up for Medicare?
You can sign up anytime while you (or your spouse) are still working and you have health insurance through that employer. You also have 8 months after you (or your spouse) stop working to sign up.
Do I need to get Medicare drug coverage (Part D)?
Prescription drug coverage that provides the same value to Medicare Part D. It could include drug coverage from a current or former employer or union, TRICARE, Indian Health Service, VA, or individual health insurance coverage.
How to apply for Medicare Supplement?
What you'll need to apply: 1 Your Medicare card 2 Your banking information and a voided check if you want to sign up for automatic payment withdrawal 3 Your Social Security number 4 2021 Medicare Supplement Outline of Coverage (PDF) 5 2021 Medicare Supplement Application Form (PDF) 6 2021 Medicare Supplement Dental Vision Hearing Application Form (PDF)
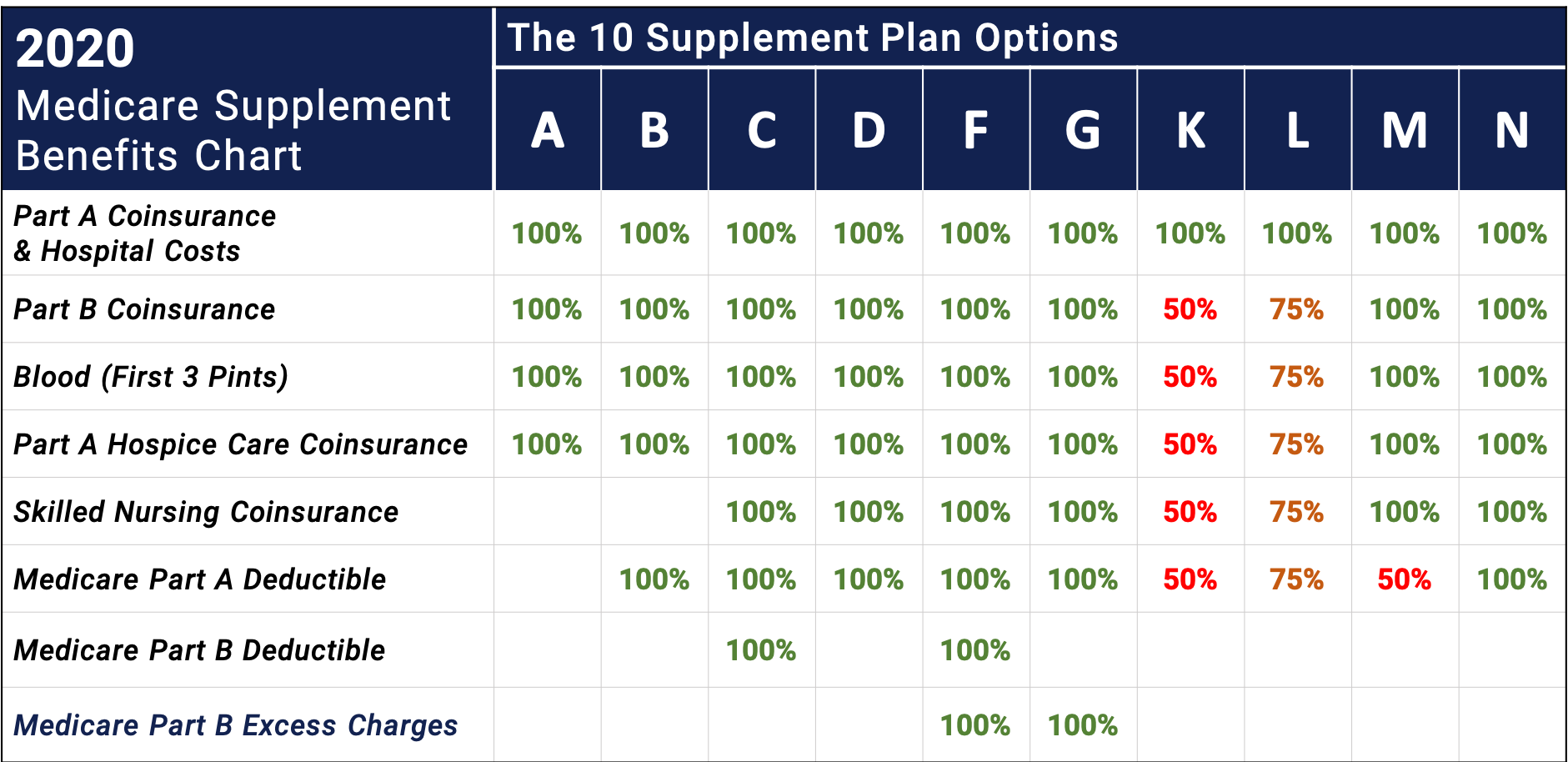
When will Medicare stop covering Part B?
Medicare supplement plans that cover the Part B deductible (Plans C, F, and high‑deductible F) will no longer be available for individuals who turned 65 or become eligible for Medicare on or after January 1, 2020.
Is Blue Cross Medicare endorsed by the government?
This is a solicitation of insurance. We may contact you about buying insurance. Blue Cross Medicare Supplement plans aren't connected with or endorsed by the U.S. government or the federal Medicare program. If you're currently enrolled in Plan A or Plan C, you can stay with your plan as long as you pay your premium.
Does Blue Cross Blue Shield of Michigan accept Medicare?
or its territories that accepts Medicare. You don't have to use our network. Blue Cross Blue Shield of Michigan administers Blue Cross Medicare Supplement plans.
