When will I receive my Medicare card?
Medicare.gov. Medicare Questions on Open Enrollment. Medigap (Medicare supplement) policies. Missouri Department of Social Services - MO HealthNet (also known as Medicaid) Missouri Medicaid Audit & Compliance. Missouri Rx Plan (provides pharmacy benefits to eligible Missourians enrolled in Medicare Part D) Missouri Senior Medicare Patrol Project.
When will Medicaid expansion take effect in Missouri?
Sep 16, 2018 · To qualify for Medicare, you must be either a United States citizen or a legal permanent resident of at least five continuous years. Residents may be enrolled automatically at age 65 if they already receive benefits through the Social Security Administration (SSA) or the Railroad Retirement Board (RRB).
When do you have to apply for Medicare initial enrollment period?
FSD will provide MO HealthNet coverage for individuals between the ages of 19 and 64 who have a positive COVID-19 diagnosis and meet current MHABD eligibility guidelines, including income and resources. Questions regarding the entry of COVID-19 MHN coverage may be sent via email to [email protected].
How do I get Medicare benefits in Missouri?
Medicaid expansion extends coverage to adults under age 65 with household incomes up to 138% of the poverty level. In 2022, that amounts to about $18,754 for a single individual, and $38,295 for a household of four (children were already eligible for Medicaid at higher income levels). This is eventually expected to result in 275,000 Missouri ...
What is the income limit for Missouri Medicare?
Income eligibility: The income limit is $904 a month if single and $1,222 a month if married. (Note that a higher income limit – of $1,064 a month if single and $1,437 if married – applies to applicants who are blind.)Oct 4, 2020
What are the Medicaid guidelines for Missouri?
Adults under the age of 65 with household incomes up to 138% of the federal poverty level are now eligible for Missouri Medicaid. In 2021, this amounts to about $17,774 for an individual or $24,039 for a household of two. Unsure if you're eligible? Use the Medicaid Eligibility Calculator to find out.
What is the timely filing limit for Missouri Medicaid?
Timely Filing Criteria - Original Submission MO HealthNet Claims: Claims from participating providers that request MO HealthNet reimbursement must be filed by the provider and received by the fiscal agent or state agency within 12 months from the date of service.
What is the look back period for Medicaid in Missouri?
Missouri has a 5-year Medicaid Look-Back Period that immediately precedes one's Medicaid application date. This is a period in which Medicaid checks to ensure no assets were gifted or sold under fair market value. If this has been done, Medicaid assumes it was to meet Medicaid's asset limit.Mar 28, 2022
What is the difference between Medicare and Medicaid?
Medicare is a federal program that provides health coverage if you are 65+ or under 65 and have a disability, no matter your income. Medicaid is a state and federal program that provides health coverage if you have a very low income.
Is Medicaid free for seniors?
You may qualify for free or low-cost care through Medicaid based on income and family size. In all states, Medicaid provides health coverage for some low-income people, families and children, pregnant women, the elderly, and people with disabilities.
Is Missouri HealthNet the same as Medicaid?
MO HealthNet is the Medicaid program for Missouri. MO HealthNet provides health insurance coverage for those with very low incomes and assets.
Does Missouri Medicaid require prior authorization?
Prior authorization is not required for emergency or urgent care. Out-of-network physicians, facilities and other health care providers must request prior authorization for all procedures and services, excluding emergent or urgent care.Apr 1, 2021
What is a Medicaid spend down in Missouri?
What is Spend Down? MO HealthNet for the Elderly, Blind, and Disabled with a Spend Down allows consumers who have income above the income level for MO HealthNet for Disabled (Medicaid) to qualify for coverage. The Spend Down amount is the amount of income that is above the income maximum.
Can Medicaid take your house in Missouri?
In those circumstances Missouri Medicaid cannot place a lien on the home. However, if the applicant is single or something happens and the spouse or dependent relative ceases to occupy the home, Missouri Medicaid can and will place a lien on the home.Jan 18, 2019
What is the income limit for food stamps in Missouri?
Who is eligible for this program?Household Size*Maximum Income Level (Per Year)1$16,9882$22,8883$28,7884$34,6884 more rows
What does Medicaid look back rule pertain to?
Medicaid's Look-Back Period Explained Medicaid's look-back period is meant to prevent Medicaid applicants from giving away assets or selling them under fair market value to meet Medicaid's asset limit. All asset transfers within the look-back period are reviewed.Dec 14, 2021
About Medicare in Missouri
Beneficiaries in Missouri have two options when it comes to how to get their Medicare benefits. The first is Original Medicare, Part A and Part B....
Medicare Coverage in Missouri
Certain types of Medicare insurance are only available through Medicare-approved health insurance companies. This includes not only Medicare Advant...
Local Medicare Resources For Missouri
1. Medicare Savings Programs in Missouri: Medicare beneficiaries with low incomes may be able to get help paying for out-of-pocket costs like Medic...
How to Apply For Medicare in Missouri
The Original Medicare enrollment process is the same in Missouri as in any other state. To qualify for Medicare, you must be either a United States...
How much money can you make to qualify for Medicaid in Missouri?
All Medicaid-eligible populations are subject to income limits (as we’ll discuss in a moment, some populations are also subject to asset limits). I...
What is the asset limit for Medicaid in Missouri?
For the groups described above, only an income limit applies. But for Missouri Medicaid applicants whose eligibility is based on their status as ag...
How does Medicaid provide assistance to Medicare beneficiaries in Missouri?
Many Medicare beneficiaries receive help through Medicaid with the cost of Medicare premiums, co-pays, deductibles, and services Medicare doesn’t c...
What is Medicare Part A?
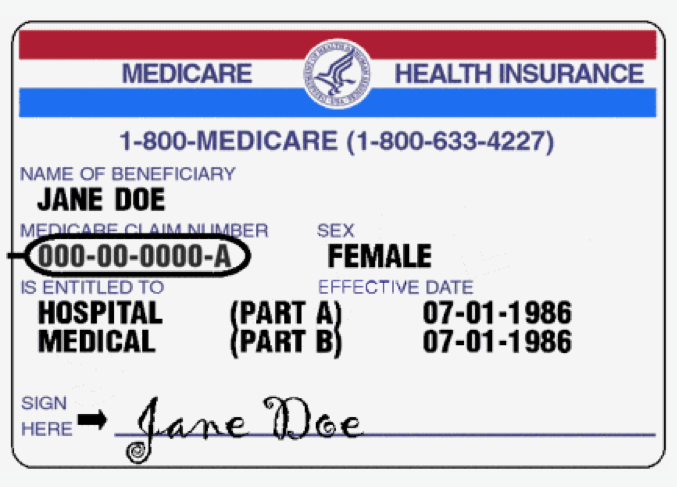
Medicare Part A covers inpatient care you get in a hospital, skilled nursing facility, or hospice setting. Medicare Part B covers outpatient care, including (but not limited to) doctor visits, durable medical equipment, preventive services, and ambulance transportation. Missouri beneficiaries may decide to enroll in a Medicare Advantage plan, ...
What is Medicare in Missouri?
Beneficiaries in Missouri have two options when it comes to how to get their Medicare benefits. The first is Original Medicare, Part A and Part B. This is the federally-run health insurance program for those age 65 and older and younger residents with certain disabilities or conditions.
What is Medicare Supplement?
Medicare Supplement: Also known as Medigap, these plans cover out-of-pocket health-care costs that Original Medicare does not, such as deductibles, copayments, and coinsurance. Some of these plans also include coverage for emergency health care in foreign countries. Most states, including Missouri, offer up to 10 standardized plan types, ...
How long do you have to be a resident of Missouri to get Medicare?
To qualify for Medicare, you must be either a United States citizen or a legal permanent resident of at least five continuous years.
Does Missouri have Medicare Advantage?
Missouri beneficiaries may decide to enroll in a Medicare Advantage plan, also called Medicare Part C, through a Medicare-approved insurance company. These plans must cover the same benefits as Original Medicare (with the exception of hospice care), but may include additional benefits such as routine vision and dental services, ...
How many standardized plans are there in Missouri?
Most states, including Missouri, offer up to 10 standardized plan types, and each kind of plan is marked with a letter. Plans of the same letter offer the same benefits, regardless of location or the insurance company you purchase from. For example, benefits for Plan G sold in Missouri would be the same as for Plan G sold in California.
Is Medicare available in Missouri?
Certain types of Medicare insurance are only available through Medicare-approved health insurance companies. This includes not only Medicare Advantage plans, but also prescription drug coverage and supplemental coverage. Here are the types of Medicare plan options you may have available as a Missouri beneficiary: ...
What age does FSD cover?
FSD will provide MO HealthNet coverage for individuals between the ages of 19 and 64 who have a positive COVID-19 diagnosis and meet current MHABD eligibility guidelines, including income and resources.
How long does it take to get a family support call?
Family Support Division will call the client within 3 days of receiving the application at the phone number listed on the application. If possible the interview will be completed during this phone call. If this call is missed or the interview cannot be completed, the client can call back at 855-823-4908 to complete the interview.
Does FSD enter bills in March?
FSD still will enter the bills for March and then at the first of each month FSD will manually enter spend down met with bills through the emergency period. Example: Wally is enrolled in automatic withdrawal.
Can you get refunded if you pay spend down?
If the spend down is paid, it will not be refunded. If a client is enrolled in automatic withdrawal, payment will continue to come out each month. The client can opt out of automatic payments, but will have to re-enroll again later. Example: Kim meets her spend down using bills on March 12th.
Does Family Support end with a check?
with a check, money order, or cashiers check. Family Support division will not end coverage if the spend down is not met. The spend down will not need to be paid at a later date . Coverage will begin with the first month the spend down is met and continue each month with no end date while the emergency is in place.
How much will Medicaid be available in 2021?
In 2021, that amounts to about $17,774 for a single individual, and $36,570 for a household of four (children are already eligible for Medicaid at higher income levels).
What is the income threshold for CHIP 2021?
For a household of three in 2021, that amounts to just under $33,000 in annual income. Children above the Medicaid income thresholds are eligible for CHIP if their household incomes are up to 300% of poverty.
How many signatures are needed for Medicaid expansion in Missouri?
Advocates spent the summer determining the feasibility of Medicaid expansion by ballot initiative in Missouri, and announced in September 2019 that they would commit to gathering the 172,000 signatures necessary for the measure to appear on the ballot.
How many people are in the coverage gap in Missouri?
For now, 127,000 people remain in the coverage gap in Missouri — unable to qualify for Medicaid because the state still has not expanded eligibility for Medicaid coverage, and unable to qualify for premium subsidies in the exchange/marketplace because they earn less than the poverty level.
Which states have lower Medicaid eligibility caps?
Only Texas and Alabama have lower Medicaid eligibility caps, at 18%. As the ACA was written, it called for Medicaid expansion in every state for residents with incomes up to 133% of poverty (138% with the built-in 5% income disregard). But in 2012, the Supreme Court ruled that states could not be penalized for opting out of expansion, ...
When will Medicaid be expanded?
Constitutional amendment to expand Medicaid was approved by voters in August 2020 election. The Medicaid expansion ballot measure passed in August 2020 by a margin of about 53 to 47. It called for the state to submit a Medicaid expansion state plan amendment to the federal government by March 2021, and for Medicaid expansion to take effect by July ...
Is Missouri expanding Medicaid?
Although the federal government began providing funding to expand Medicaid in 2014, Missouri is one of 13 states that has thus far rejected Medicaid expansion. The MO HealthNet program (Missouri Medicaid) still has the same strict eligibility standards that applied before the Affordable Care Act was enacted.
What is RBM in medical?
conjunction with Xerox and MedSolutions (MSI), implemented a new quality-based Radiology Benefit Management Program (RBM). The RBM is an expansion of the existing precertification process previously used for MRIs and CTs of the brain, head, chest and spine. As of July 19, 2010, certain radiologic procedures require precertification and are processed using clinical guidelines that are available at http://medsolutions.com/documents/guidelines/guidelines.php. The guidelines are not intended to supersede or replace sound medical judgment, but instead should facilitate the identification of the most appropriate imaging procedure based upon the participant’s clinical condition.
What is a PT in MO?
Physical therapy (PT) is a MO HealthNet covered service for participants under age 21 or in the categories of assistance for pregnant women, blind participants or nursing facility residents . Use CPT procedure codes in the 97000 range for PT evaluation. If physical therapy is provided for a participant under 21 years of age as a result of a screening, enter code “A1” in fields 18-24 of the UB-04 claim form or the appropriate field(s) on the electronic claim form to indicate that it is an EPSDT/HCY service.
What is the 5th digit of 630?
630 631 633 range 640-649 range with a fifth digit of 0, 1, 2 or 3 651-676 range with a fifth digit of 0, 1, 2 or 3 677
What is the through date of service in field 6?
The through date of service in field 6 is included in the covered days, if the patient status code in field 17 is equal to "30- still a patient."
How to access MO HealthNet eligibility?
Providers can access MO HealthNet participant eligibility files via the Web site. Functions include eligibility verification by participant ID, casehead ID and child's date of birth, or Social Security number and date of birth. Eligibility verification can be performed on an individual basis or in a batch file. Individual eligibility verification occurs in real-time basis similar to the Interactive Voice Response System, which means a response is returned immediately. Batch eligibility verifications are returned to the user within 24 hours.
What is the MO HealthNet number?
The MO HealthNet fax line for non-emergency service or equipment exception requests only is (573) 522-3061; the fax line to obtain a drug prior authorization is (573) 636-6470. Do not use either of these numbers for requests for pre-certifications of MRI, MRA, CT, CTA, PET, ultrasound and cardiac imaging studies procedures.
Can a denied claim be resubmitted?
If there is a denied claim in the MO HealthNet emomed system, then the claim can be resubmitted as a New Claim. A denied claim can also be resubmitted by choosing Timely Filing, Copy Claim-original, or Copy Claim-advanced.
What is CSRA in Missouri?
This, in Medicaid speak, is called the Community Spouse Resource Allowance (CSRA) and is intended to prevent spousal impoverishment. The CSRA does not extend to non-applicant spouses of regular Medicaid applicant spouses. It’s important to be aware that Missouri has a 5-year Medicaid Look-Back Period.
How much is the spousal allowance for 2021?
From January 2021 – December 2021, it is $3,259.50 / month. This spousal allowance rule is meant to ensure non-applicant spouses have sufficient funds with which to live. To be very clear, an income allowance is not permitted for married couples with one spouse applying for regular Medicaid.
What income is counted for Medicaid?
Examples include employment wages, alimony payments, pension payments, Social Security Disability Income, Social Security Income, IRA withdrawals, and stock dividends.
What is MMMNA in Medicaid?
Relevant to married couples with one spouse applying for home and community based services via a Medicaid waiver or nursing home Medicaid, there is a Minimum Monthly Maintenance Needs Allowance (MMMNA). This is the minimum amount of monthly income to which the non-applicant spouse is entitled.
What are countable assets?
Countable assets include cash, stocks, bonds, investments, credit union, savings, and checking accounts, and real estate in which one does not reside. However, for Medicaid eligibility, there are many assets that are considered exempt (non-countable).
When only one spouse of a married couple is applying for nursing home Medicaid or a HCBS waiver, is
When only one spouse of a married couple is applying for nursing home Medicaid or a HCBS Medicaid waiver, only the income of the applicant is counted. Said another way, the income of the non-applicant spouse is disregarded.
What is the income limit for blind people in 2021?
For those who are blind, the income limits are slightly higher. As of April 2021, the income limit for a single blind applicant is $1,074 / month , and for a blind married couple with both spouses as applicants, the monthly income limit is $1,452.
What is a stand alone Medicare plan?
Stand-alone Medicare prescription drug plan (Medicare Part D) – you might want this type of plan if you need prescription drug coverage. You need Part A or Part B to qualify. If you don’t enroll during your Medicare Initial Enrollment Period (IEP), you might have to wait to sign up.
What is Medicare Advantage?
Medicare Advantage (Medicare Part C) – this program gives you an alternative way to get your Medicare Part A and Part B benefits (many plans also include prescription drug benefits too). You need Part A and Part B to qualify, and then the plan (instead of the government) manages those benefits for you.
When do you need to enroll in Medicare Supplement?
You need Part A and Part B to qualify. Usually the best time to enroll is during your Medicare Supplement Open Enrollment Period. That 6-month period starts the month you’re both 65 or older, and enrolled in Part B.
When does IEP start?
So if your 65th birthday is in November, your IEP runs from August through February. Your IEP is different if you’re not yet 65, but you qualify for Medicare by disability.
Is Medicare Part A or B?
You might be automatically enrolled in Medicare Part A and Part B (Original Medicare). But if you want to sign up for other Medicare coverage, right about when you’re first eligible for Medicare might be a good time to enroll. If you’re not already getting Social Security retirement benefits when you turn 65, you generally won’t be automatically ...
Do you have to take action if you are automatically enrolled in Medicare?
But even if you’re automatically enrolled in traditional Medicare, you do have to take action if you want other Medicare coverage.
Is Medicare Part A premium free?
Enroll in Medicare Part A as soon as they’re eligible. Even if your employer plan has hospital coverage, Part A is premium-free for most people. If your employer plan has hospital coverage, and you have a hospital stay, your plan and Medicare Part A will coordinate benefits to work out payment of your hospital costs.
What is conditional payment?
A conditional payment is a payment Medicare makes for services another payer may be responsible for.
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare. When Medicare began in 1966, it was the primary payer for all claims except for those covered by Workers' Compensation, ...
Why is Medicare conditional?
Medicare makes this conditional payment so that the beneficiary won’t have to use his own money to pay the bill. The payment is “conditional” because it must be repaid to Medicare when a settlement, judgment, award or other payment is made. Federal law takes precedence over state laws and private contracts.
How long does ESRD last on Medicare?
Individual has ESRD, is covered by a GHP and is in the first 30 months of eligibility or entitlement to Medicare. GHP pays Primary, Medicare pays secondary during 30-month coordination period for ESRD.
What are the responsibilities of an employer under MSP?
As an employer, you must: Ensure that your plans identify those individuals to whom the MSP requirement applies; Ensure that your plans provide for proper primary payments whereby law Medicare is the secondary payer; and.
What is the purpose of MSP?
The MSP provisions have protected Medicare Trust Funds by ensuring that Medicare does not pay for items and services that certain health insurance or coverage is primarily responsible for paying. The MSP provisions apply to situations when Medicare is not the beneficiary’s primary health insurance coverage.
What age does GHP pay?
Individual is age 65 or older, is covered by a GHP through current employment or spouse’s current employment AND the employer has 20 or more employees (or at least one employer is a multi-employer group that employs 20 or more individuals): GHP pays Primary, Medicare pays secondary. Individual is age 65 or older, ...
