G-codes are used to report a beneficiary’s functional limitation being treated and note whether the report is on the beneficiary’s current status, projected goal status, or discharge status. There are 42 functional G-codes that are comprised of 14 functional code sets with three types of codes in each set.
What are G codes used for Medicare?
- Physical Therapist – signified by GP
- Occupational Therapist – signified by GO
- Speech-Language Pathologist – signified by GN (GN??)
Does Medicaid require G codes?
No. G-codes are no longer mandatory—for PQRS or for FLR—and PTs, OTs, and SLPs no longer have to include them on Medicare claims. Providers are also no longer able to use G-codes to report Quality measures for MIPS. Don’t face Medicare compliance alone.
What are G codes in medical billing?
- Create clear, detailed documentation during each patient’s episode of care.
- Audit your clinic’s documentation process regularly to ensure defensibility.
- File your claims in a timely manner.
- Stay current on reporting regulations, requirements, and legislation.
Are G codes billable?
The Centers for Medicare & Medicaid Services (CMS) established non-payable G-codes for reporting on claims for Medicare Part B beneficiaries receiving therapy services. Each non-payable G-code listed on the claim form must be accompanied with a severity/complexity modifier.
Does Medicare require G codes?
Note: Due to CY 2019 Physician Fee Schedule (PFS) rulemaking, effective for dates of service on or after January 1, 2019, Medicare no longer requires the functional reporting of nonpayable HCPCS G-codes and severity modifiers − adopted to implement section 3005(g) of MCTRJCA − on claims for therapy services.
What are G HCPCS codes used for?
G codes are national codes assigned by CMS to identify professional healthcare procedures and services that may not have assigned CPT® codes.
Are G codes required for Medicare in 2021?
The Centers for Medicare & Medicaid Services (CMS) has finalized its new add-on code for visit complexity, which should be a financial boon to primary care doctors. All family physicians should be aware of the code, G2211, and use it appropriately on a frequent basis starting in 2021.
What is G0463 used for?
HCPCS Code G0463 is used for all FACILITY evaluation and management visits, regardless of the intensity of service provided.
Can G-codes be billed to Medicare Advantage plans?
New. Yes, most MA plans will allow both the G0402/438/439 and age appropriate wellness exam at the same visit as long as the documentation meets the requirements for each. We are getting reimbursed for both.
Are G codes CPT codes?
Temporary G codes are assigned to services and procedures that are under review before being included in the CPT coding system. Payment for these services is under the jurisdiction of the local carriers.
Does Medicaid use G codes?
Revision Date (Medicaid): 1/1/2021 The G codes differ based on the number of drug classes including metabolites tested. Only one code from the G code range may be reported per date of service. Codes 80320-80377 or 83992 shall not be reported on the same date of service as codes G0480-G0483.
How do you bill for phone encounters?
The following codes may be used by physicians or other qualified health professionals who may report E/M services:99441: telephone E/M service; 5-10 minutes of medical discussion.99442: telephone E/M service; 11-20 minutes of medical discussion.99443: telephone E/M service, 21-30 minutes of medical discussion.
When can you bill G0463?
CPT code G0463 will be reported by the physician when service renders at the hospital outpatient clinic visit for assessment and management of a patient.
What is G0463 billing code?
HCPCS code G0463 for Hospital outpatient clinic visit for assessment and management of a patient as maintained by CMS falls under Miscellaneous Services .
Does Medicare cover CPT code G0463?
Ordinarily, when a patient is seen at a HOPD clinic, the hospital bills Medicare for a clinic visit using HCPCS code G0463. This fee covers the hospital's administrative expenses associated with the visit.
Medicare G Code Confusion
Let’s start with the easy stuff and progress on up through Medicare G code confusion:
Medicare G Code Confusion – More Confusion with Modifiers
Ok, now to add a new wrinkle in the Medicare G code confusion, here are the G modifiers, not to be confused with the G codes. When the therapy caps were mandated in the Balanced Budget Act of 1997 CMS required all disciplines to enter a modifier indicating therapy type by the GP, GO or GN modifier.
Clearing Up Medicare G Code Confusion – Play Book
What’s a provider to do? More importantly what is everyone that is involved in this process to do? Ban the terminology “G code”, call everything by its name, PQRS, FLR, unattended electrical stimulation and therapy discipline modifiers.
Spotlight
The Functional Reporting requirements of reporting the functional limitation nonpayable HCPCS G-codes and severity modifiers on claims for therapy services and the associated documentation requirements in medical records have been discontinued, effective for dates of service on and after January 1, 2019.
Functional Reporting
Functional Reporting gathers data on beneficiaries’ functional limitations during the therapy episode of care as reported by therapy providers and practitioners furnishing physical therapy (PT), occupational therapy (OT) and speech-language pathology (SLP) services.
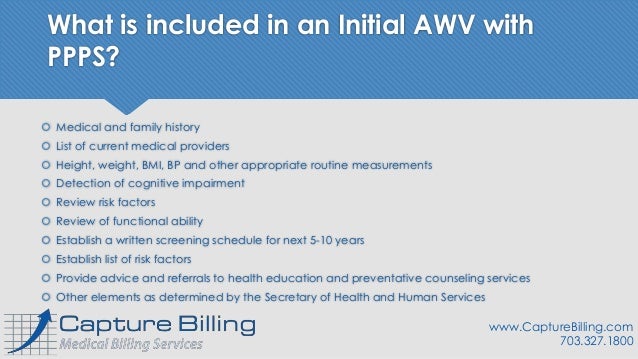
What is the HCPCS code for a wellness visit?
This exam is billed using HCPCS code G0402. An Annual Wellness Visit code of G0438 should not be used — and will be denied — because the patient is eligible for the Welcome to Medicare visit during the first year of enrollment. For more information on the Welcome to Medicare visit go-to CMS.
Is 99397 covered by Medicare?
Preventative Medicine codes 99387 and 99397, better known to offices as Complete Physical Exams or Well Checks for 65 and older, still remain a non-covered, routine service from Medicare. The Well Woman Exam codes G0101 and Q0091 are covered services.
What is a G8442?
Patient not eligible for pain assessment for documented reasons. G8442: Documentation that patient is not eligible for a pain assessment. Pain assessment documented, follow-up plan not documented, patient not eligible/appropriate.
What is a measure group?
Measures groups are a subset of four or more PQRS measures that have a particular clinical condition or focus in common. All applicable measures within a group must be reported for each patient within the sample that meets the required criteria (such as age or gender). G Codes are reported by the Registry.
