Medical and hospital services arising from non-covered services are covered when determined to be reasonable and necessary. When a member is admitted to the hospital for a non-covered service: Complications of non-covered procedures develop after the member has been formally discharged from the hospital providing the non-covered service.
What services are not covered under Medicare Part?
Some of the items and services Medicare doesn't cover include: Services that include medical and non-medical care provided to people who are unable to perform basic activities of daily living, like dressing or bathing. Long-term supports and services can be provided at home, in the community, in assisted living, or in nursing homes.
What are medical non covered services?
This benefit, referred to as non-emergency medical transportation or NEMT ... Members still call the same number to schedule a ride for covered services. Members will still have access to online ...
What dental services are not covered by Medicare?
The following two categories of services are excluded from coverage: A primary service (regardless of cause or complexity) provided for the care, treatment, removal, or replacement of teeth or structures directly supporting teeth, e.g., preparation of the mouth for dentures, removal of diseased teeth in an infected jaw. A secondary service that is related to the teeth or structures directly supporting the teeth unless it is incident to and an integral part of a covered primary service that ...
What is Medicare notice of non coverage?
What does Notice of Medicare non-coverage mean? If you are enrolled in a Medicare Advantage Plan, a Notice of Medicare Non-Coverage (NOMNC) is a notice that tells you when care you are receiving from a home health agency (HHA), skilled nursing facility (SNF), or comprehensive outpatient rehabilitation facility (CORF) is ending and how you can contact a Quality …

When should I issue a Medicare non coverage notice?
The NOMNC must be delivered at least two calendar days before Medicare covered services end or the second to last day of service if care is not being provided daily. Note: The two day advance requirement is not a 48 hour requirement.
Can I bill Medicare for non-covered services?
Under Medicare rules, it may be possible for a physician to bill the patient for services that Medicare does not cover. If a patient requests a service that Medicare does not consider medically reasonable and necessary, the payer's website should be checked for coverage information on the service.
What is the purpose of the notice of Medicare non coverage?
A Notice of Medicare Non-Coverage (NOMNC) is a notice that indicates when your care is set to end from a home health agency (HHA), skilled nursing facility (SNF), comprehensive outpatient rehabilitation facility (CORF), or hospice.
What is a Medicare non coverage form?
Informs beneficiaries of their discharge when their Medicare covered services are ending. Issued by: Centers for Medicare & Medicaid Services (CMS)
What is the difference between a covered service and a non-covered service?
Whether or not a service is covered is dependent upon your insurance policy. For example, Medicare will pay for an annual physical exam as part of a covered service. However, Medicare does not pay for normal dental procedures. Non-covered services are services patients are responsible for paying on their own.
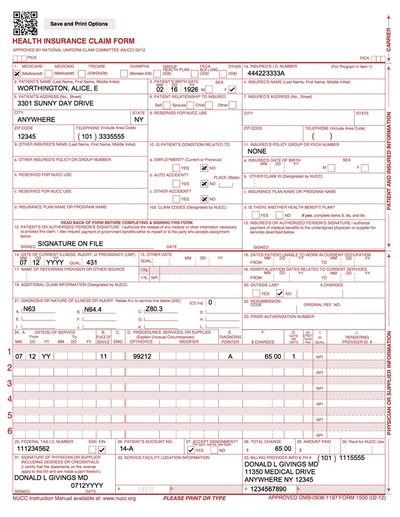
What Medicare form is used to show charges to patients for potentially non-covered services?
(Medicare provides a form, called an Advance Beneficiary Notice (ABN), that must be used to show potentially non-covered charges to the patient.)
Is an ABN required for non covered services?
Non-covered services do not require an ABN since the services are never covered under Medicare. While not required, the ABN provides an opportunity to communicate with the patient that Medicare does not cover the service and the patient will be responsible for paying for the service.
When must you provide a DENC to a patient?
The DENC must be provided no later than close of business of the day of the QIO's notification. Providers may include their business logo and contact information on the top of the DENC.
What is an Advance Beneficiary Notice of Non Coverage?
The Advance Beneficiary Notice of Noncoverage (ABN), Form CMS-R-131, is issued by providers (including independent laboratories, home health agencies, and hospices), physicians, practitioners, and suppliers to Original Medicare (fee for service - FFS) beneficiaries in situations where Medicare payment is expected to be ...
Who is responsible for issuing Nomnc?
A Medicare health provider must give an advance, completed copy of the Notice of Medicare Non-Coverage (NOMNC) to enrollees receiving skilled nursing, home health (including psychiatric home health), or comprehensive outpatient rehabilitation facility services, no later than two days before the termination of services.
How do you explain ABN to patients?
An ABN is a written notice from Medicare (standard government form CMS-R-131), given to you before receiving certain items or services, notifying you: Medicare may deny payment for that specific procedure or treatment. You will be personally responsible for full payment if Medicare denies payment.
Does Medicare Part A use ABN?
Medicare inpatient hospitals and skilled nursing facilities (SNFs) use other approved notices for Part A items and services when notice is required in order to shift potential financial liability to the beneficiary; however, these facilities must use the ABN for Part B items and services.
What are non covered services?
Medicare Non-covered Services. There are two main categories of services which a physician may not be paid by Medicare: Services not deemed medically reasonable and necessary. Non-covered services. In some instances, Medicare rules allow a physician to bill the patient for services in these categories. Understanding these rules and how ...
When Medicare or another payer designates a service as “bundled,” does it make separate payment for the pieces of the
When Medicare or another payer designates a service as “bundled,” it does not make separate payment for the pieces of the bundled service and does not permit you to bill the patient for it since the payer considers payment to already be included in payment for another service that it does cover. Coordination of Benefits.
What is pre-emptive communication?
Pre-emptive communication through a voluntary ABN can prevent negative patient perceptions of your practice and facilitate collections. These modifiers are not required by Medicare, but do allow for clean claims processing and billing to the patient.
What is an ABN for Medicare?
If a Medicare patient wishes to receive services that may not be considered medically reasonable and necessary, or you feel Medicare may deny the service for another reason, you should obtain the patient’s signature on an Advance Beneficiary Notice (ABN).
What does the -GX modifier mean?
The -GX modifier indicates you provided the notice to the beneficiary that the service was voluntary and likely not a covered service. -GY – Item or service statutorily excluded, does not meet the definition of any Medicare benefit or for non-Medicare insurers, and is not a contract benefit.
Is it reasonable to ask for a service from Medicare?
Medically Reasonable and Necessary. A patient may ask for a service that Medicare does not consider medically reasonable and necessary under the circumstances. For instance, the patient wants the service more frequently than Medicare allows or for a diagnosis that Medicare does not cover.
Do commercial insurance companies have similar coverage guidelines?
Commercial insurance companies and some Medicaid payers will have similar types of information about their coverage guidelines on their websites. Stay up-to-date on these policies for your local payers to ensure claims are processed as medically reasonable and necessary.
Does Medicare cover exceptions?
This booklet outlines the 4 categories of items and services Medicare doesn’t cover and exceptions (items and services Medicare may cover). This material isn’t an all-inclusive list of items and services Medicare may or may not cover.
Does Medicare cover personal comfort items?
Medicare doesn’t cover personal comfort items because these items don’t meaningfully contribute to treating a patient’s illness or injury or the functioning of a malformed body member. Some examples of personal comfort items include:
Does Medicare cover non-physician services?
Medicare normally excludes coverage for non-physician services to Part A or Part B hospital inpatients unless those services are provided either directly by the hospital/SNF or under an arrangement that the hospital/SNF makes with an outside source.
Does Medicare cover dental care?
Medicare doesn’t cover items and services for the care, treatment, filling, removal, or replacement of teeth or the structures directly supporting the teeth, such as preparing the mouth for dentures, or removing diseased teeth in an infected jaw. The structures directly supporting the teeth are the periodontium, including:
Can you transfer financial liability to a patient?
To transfer potential financial liability to the patient, you must give written notice to a Fee-for-Service Medicare patient before furnishing items or services Medicare usually covers but you don’ t expect them to pay in a specific instance for certain reasons, such as no medical necessity .
How long is a Medicare extended treatment notice valid?
A single notice for an extended course of treatment is only valid for 1 year. If the extended course of treatment continues after 1 year, issue a new notice.
How long does it take for Medicare to refund a claim?
Medicare considers refunds timely within 30 days after you get the Remittance Advice from Medicare or within 15 days after a determination on an appeal if you or the beneficiary file an appeal.
When do you issue a reduction notice?
Reductions occur when a component of care decreases (for example, frequency or service duration). Do not issue the notice every time there is a reduction in care. If a reduction occurs and the beneficiary wants to continue getting care no longer considered medically reasonable and necessary, you must issue the notice before the beneficiary gets the noncovered care.
Is an ABN valid for Medicare?
An ABN is valid if beneficiaries understand the meaning of the notice. Where an exception applies, beneficiaries have no financial liability to a non-contract supplier furnishing an item included in the Competitive Bidding Program unless they sign an ABN indicating Medicare will not pay for the item because they got it from a non-contract supplier and they agree to accept financial liability.
Does Medicare cover frequency limits?
Some Medicare-covered services have frequency limits. Medicare only pays for a certain quantity of a specific item or service in each period for a diagnosis. If you believe an item or service may exceed frequency limits, issue the notice before furnishing the item or service to the beneficiary.
Does Medicare cover exceptions?
This booklet outlines the 4 categories of items and services Medicare doesn’t cover and exceptions (items and services Medicare may cover). This material isn’t an all-inclusive list of items and services Medicare may or may not cover.
Does Medicare cover personal comfort items?
Medicare doesn’t cover personal comfort items because these items don’t meaningfully contribute to treating a patient’s illness or injury or the functioning of a malformed body member. Some examples of personal comfort items include:
Does Medicare cover non-physician services?
Medicare normally excludes coverage for non-physician services to Part A or Part B hospital inpatients unless those services are provided either directly by the hospital/SNF or under an arrangement that the hospital/SNF makes with an outside source.
Does Medicare cover dental care?
Medicare doesn’t cover items and services for the care, treatment, filling, removal, or replacement of teeth or the structures directly supporting the teeth, such as preparing the mouth for dentures, or removing diseased teeth in an infected jaw. The structures directly supporting the teeth are the periodontium, including:
Can you transfer financial liability to a patient?
To transfer potential financial liability to the patient, you must give written notice to a Fee-for-Service Medicare patient before furnishing items or services Medicare usually covers but you don’ t expect them to pay in a specific instance for certain reasons, such as no medical necessity .
What are the categories of Medicare?
The four categories are: Services denied as bundled or included in the basic allowance of another service; and.
What is denied as bundled or included in the basic allowance of another service?
Services denied as bundled or included in the basic allowance of another service; and. Services reimbursable by other organizations or furnished without charge. With respect to the first category, services that are not medically reasonable and necessary to the patient’s overall diagnosis and treatment are not covered.
Is no fault insurance covered by Medicare?
In relation to category four, some services are reimbursable under automobile, no-fault or liability insurance, or workers’ compensation programs and, therefore, are not covered by Medicare.
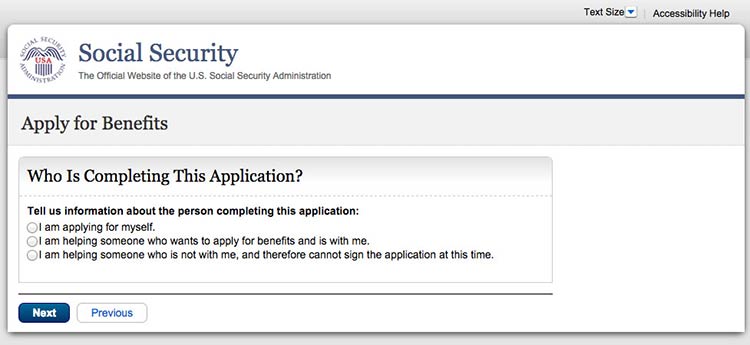
What is mandatory claim submission?
Due to mandatory claim submission, providers must file claims on behalf of Medicare beneficiaries for non-covered services. This allows the claim to process and provide the beneficiary the necessary information to submit to other insurers. Claims billed for non covered services will reflect patient liability for the charges.
What are excluded items and services?
Excluded items and services: Items and services furnished outside the U.S. Items and services required as a result of war. Personal comfort items and services. Routine services and appliances.
What is considered medically necessary?
To be considered medically necessary, items and services must have been established as safe and effective. That is, the items and services must be: Consistent with the symptoms or diagnosis of the illness or injury under treatment.
What is a secondary payer?
Services reimbursable under automobile, no-fault, or liability insurance or workers’ compensation (Medicare secondary payer). Items and services authorized or paid for by a government entity. Items and services for which the patient, another individual, or an organization has no legal obligation to pay for or furnish.
What does "not furnished" mean in medical terms?
Not furnished in a setting (such as inpatient care at a hospital or skilled nursing facility (SNF), outpatient care through a hospital or physician’s office, or home care) appropriate to the patient’s medical needs and condition.
Does Medicare cover medical care?
What you need to know. Medica re does not cover items and services that are not reasonable and necessary for the diagnosis or treatment of an illness or injury or to improve the functioning of a malformed body member. Section 1862 (a) (1) of the Social Security Act is the basis for denying payment for types of care, or specific items, ...
Can you get paid for medical procedures that have not been approved by the FDA?
Program payment, therefore, may not be made for medical procedures and services performed using devices that have not been approved for marketing by the FDA or for those not included in an FDA-approved Investigational Device Exemption trial.