When reporting modifier 27, report with condition code G0 when multiple medical visits occur on the same day in the same revenue centers. As is true for any modifier, the use of modifiers –25 and –27 must be substantiated in the patient’s medical record.
Full Answer
What is condition code G0 and how do I report it?
Aug 10, 2019 · • Claims for separate and distinct medical visits for the same beneficiary on the same date and by the same provider must have condition code G0 (zero). • Without this code subsequent claims will deny. • Denied lines will receive the edit “0110 – Date bundling not allowed” for subsequent claims that do not have condition code G0.
When to use a condition code for Medicare claims?
Feb 05, 2019 · On the first claim, report the first ER visit (revenue code 045X plus E/M code) with all ancillary services rendered on that day. On the second claim, report only the unrelated ER visit (revenue code 045X plus E/M code) with condition code G0 and modifier 27. All other charges are reported on the first claim. Proper reporting of condition code G0 allows for proper payment …
What is a condition code 04 for Medicare?
180.4 - Proper Reporting of Condition Code G0 (Zero) 180.5 - Proper Reporting of Condition Codes 20 and 21 180.6 - Emergency Room (ER) Services That Span Multiple Service Dates 180.7 - Inpatient-only Services 190 – Payer Only Codes Utilized by Medicare 200 - Special Services for OPPS Billing 200.1 - Billing for Corneal Tissue
When should Hospitals bill HCPCS code g0378?
Medicare Managed Care Manual Chapter 16b: Special Needs Plans . Table of Contents (Rev, 100, Issued 01-17-2014) Transmittals for Chapter 16b. 10 - Introduction. 10.1 - General. 10.2 - Statutory and Regulatory History. 20 - Description of SNP Types. 20.1 - Chronic Condition SNPs (C-SNPs) 20.1.1 - General. 20.1.2 - List of Chronic Conditions

What is the G0 modifier used for?
Modifier G0 Use to identify telehealth services furnished for purposes of diagnosis, evaluation, or treatment of symptoms of an acute stroke.May 26, 2021
What is G0 condition code?
Hospitals should report condition code G0 on FLs 24-30 when multiple medical visits occurred on the same day in the same revenue center but the visits were distinct and constituted independent visits.Jan 10, 2019
What are UB04 condition codes?
CMS1450/UB04 Fields: 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, and 28 are places for Condition Codes. The provider enters the corresponding code (in numerical order) to describe any conditions or events that apply to the billing period.
Does condition code 44 apply to managed Medicare?
The standard answer that is usually offered in response to this question is that CMS does not require MA plans to use condition code 44, but the MA plans rather are free to set their own requirements on hospitals.Nov 28, 2014
What are the condition codes?
Condition codes refer to specific form locators in the UB-04 form that demand to describe the conditions applicable to the billing period. It is important to note that condition codes are situational. These codes should be entered in an alphanumeric sequence.Dec 17, 2021
What are the condition codes for Medicare?
Condition codesCondition CodeDescriptionD5Cancel to correct Medicare Beneficiary ID number or provider IDD6Cancel only to repay a duplicate or OIG overpaymentD7Change to make Medicare the secondary payerD8Change to make Medicare the primary payer7 more rows•Oct 13, 2021
What is the function of condition codes?
Condition codes are extra bits kept by a processor that summarize the results of an operation and that affect the execution of later instructions. These bits are often collected together in a single condition or indicator register (CR/IR) or grouped with other status bits into a status register (PSW/PSR).
What is an A6 condition code for Medicare?
Special ProgramCodeDescriptionA6Pneumococcal pneumonia and influenza vaccines paid at 100%.A9Second opinion for surgery.AJPayer responsible for co-payment.ANPreadmission screening not required.11 more rows•Dec 21, 2020
What is a condition code 21?
Condition code 21 indicates services are noncovered, but you are requesting a denial notice in order to bill another insurance or payer source. These claims are sometimes called "no-pay bills" because they are submitted with only noncovered charges on them.Sep 27, 2018
When would you use condition code 43?
Condition Code 43 may be used to indicate that Home Care was started more than three days after discharge from the Hospital and therefore payment will be based on the MS-DRG and not a per diem payment.Nov 17, 2015
What is the purpose of other 44 codes?
Condition codes 44 and W2 both allow hospitals to recover some reimbursement for incorrect inpatient orders; however, they require different processes and, depending on the situation, may generate a slightly different payment.Sep 15, 2016
What is the 3 midnight rule?
Under current law, beneficiaries must have a hospital inpatient stay of at least three days in order to qualify for Medicare coverage SNF benefits; however, more and more patients are being coded under observation status, and access to post-acute SNF care is diminishing.May 1, 2014
When does the CMS contract end?
The contract must include the full CMS contract cycle, which begins on January 1 and ends on December 31. The MA organization may also contract with additional LTC facilities throughout the CMS contract cycle.
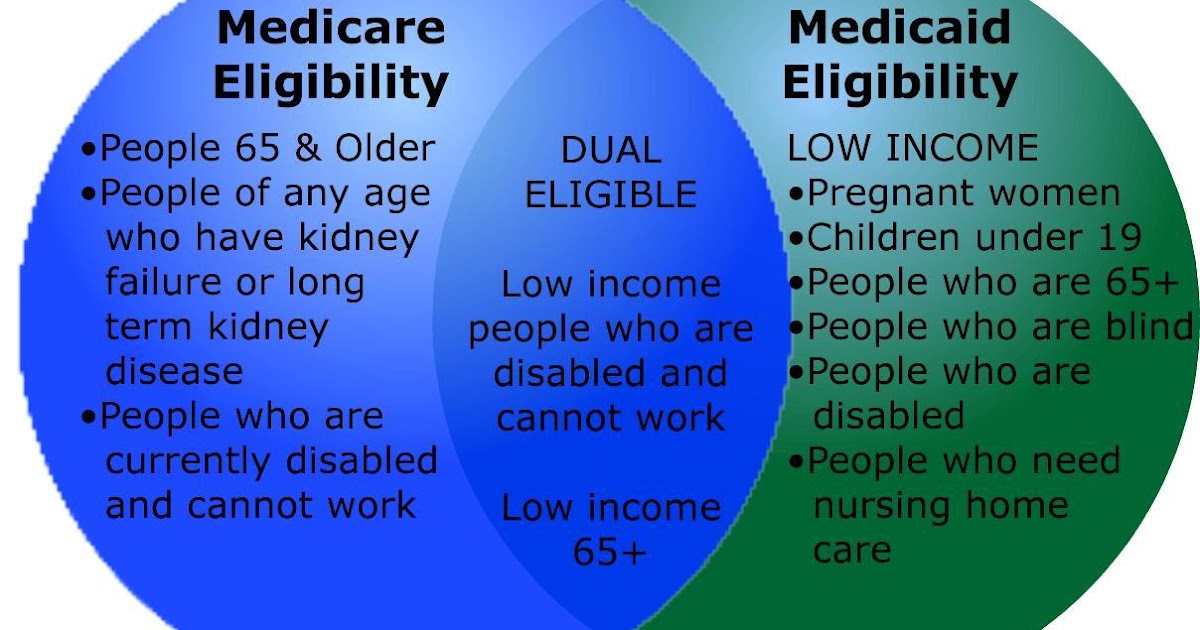
What is the loss of eligibility for D-SNP?
Loss of eligibility is most often associated with D-SNP enrollment because, unlike chronic and disabling conditions that are the bases for special needs status for enrollment into C-SNPs and I-SNPs, a D-SNP enrollee’s eligibility for enrollment is based on his/her dual eligibility for Medicare and Medicaid. Medicaid eligibility is subject to changes due to variation in the enrollee’s income from one month to another or to changes in the State’s criteria for eligibility. Thus, a dual eligible enrollee of a D-SNP may become ineligible for the plan due to the loss of his/her Medicaid eligibility for a period of time that may be one, or more months in duration.
What is a special needs CCP?
The Medicare Modernization Act of 2003 (MMA) established an MA CCP that was specifically designed to provide targeted care to individuals with unique special needs. In the MMA, Congress identified "special needs individuals" as: 1) institutionalized beneficiaries; 2) dual eligibles; and/or, 3) individuals with severe or disabling chronic conditions, as specified by CMS. MA CCPs that are established to provide services to these special needs individuals are called “Specialized MA plans for Special Needs Individuals,” or SNPs. 42 CFR Section 422.2 defines special needs individuals and specialized MA plans for special needs individuals. SNPs were first offered in 2006. The MMA gave the SNP program the authority to operate until December 31, 2008.
What does SNP need to do if an I-SNP enrollee changes residence?
If an I-SNP enrollee changes residence, the SNP must document that it is prepared to implement a CMS-approved MOC at the enrollee’s new residence, or in another SNP contracted LTC setting that provides an institutional level of care.
What is an I-SNP?
I-SNPs that serve residents of long-term care (LTC) facilities must own, operate, or have a contractual arrangement with the LTC facility that includes adherence toof its approved I-SNP MOC. Contract requirements are described below:
What does marketing materials and outreach for new enrollment indicate?
Marketing materials and outreach for new enrollment must clearly indicate that enrollment is limited to the targeted population for the particular SNP type. Further guidance on marketing within a health care setting and other SNP marketing policies is available in Chapter 3 of the
What is an all dual D-SNP?
An all-dual D-SNP enrolls beneficiaries who are eligible for Medicare Advantage and who are entitled to medical assistance under a State/Territorial plan under Title XIX of the Act. An all-dual D-SNP must enroll all categories of dual eligible individuals, including those with comprehensive Medicaid benefits as well as those with more limited cost sharing.
What does GAO recommend CMS?
GAO recommends that CMS take steps to obtain quality information on the experiences of dual-eligible beneficiaries who have been default enrolled into D-SNPs. The Department of Health and Human Services concurred with the recommendation.
What is dual eligible Medicare?
Dual-eligible beneficiaries are Medicare beneficiaries who are also enrolled in the Medicaid program in their state. In certain states, they may receive both types of benefits through private managed care plans. As of January 2019, about 386,000 such individuals were enrolled in both a private Medicare plan known as a dual-eligible special needs ...
What is managed care plan?
Managed-care plans or Advantage plans bundles all health-care coverage under one neat plan. MA plans decide on rate amounts, making prices different from plan to plan. Processing payments are done through the private plan, not Medicare.
What is Medicare Advantage 2021?
Updated on March 19, 2021. Medicare managed care plans are an alternative to Original Medicare. Otherwise known as Medicare Advantage plans with many plan types, most are either HMOs or PPOs. Managed-care plans provide benefits for gaps in Parts A and B coverage. These alternative health-care plans make up Part C of Medicare.
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare. You can also find her over on our Medicare Channel on YouTube as well as contributing to our Medicare Community on Facebook.
Can seniors travel internationally?
Coverage is not available when traveling internationally. Seniors often live in northern states for the summer and come winter, they head south. The better known as snow-birds may find they’re out-of-network for half of the year. Enrolling in a Medicare Supplement plan may be a better option for these individuals.
Is Medicare Supplement the same as Managed Care?
Managed-care plans and Medicare Supplement plans are not the same. This misconception is common. Both provide additional benefits to Original Medicare. However, they serve two totally different purposes. Managed-care plans or Advantage plans bundles all health-care coverage under one neat plan.
What is indemnity health insurance?
Before HMOs, PPOs, and others, Indemnity plans were the main plans to choose from. Indemnity plans pre-determine the percentage of what they consider a reasonable and customary charge for certain services. Carriers pay a percentage of charges for a service and the member pays the remainder.
Is Medicare managed care affordable?
Medicare managed care plans can provide some relief . Enrolling in the right plan for you is key to making health-care more affordable. The number of Medicare beneficiaries enrolling in managed care plans is on the rise. Instead of working alongside Medicare-like Medigap insurance, Advantage plans replace Original Medicare.
What are the requirements for CMS?
CMS set four requirements for this process: the patient must still be a patient in the hospital, the hospital must not have submitted a claim, the attending physician must agree with the determination and notification to the physician, and the concurrence must be documented in the medical record.
What is the MA plan?
The Medicare Managed Care Manual, Chapter 4, section 10.2 specifies that MA plans “must provide their enrollees with all basic benefits covered under original Medicare” but also states that “MA plans need not follow original Medicare claims processing procedures.
Who is Ronald Hirsch?
Ronald Hirsch, MD, is vice president of the Regulations and Education Group at Accretive Physician Advisory Services at Accretive Health. Dr. Hirsch’s career in medicine includes many clinical leadership roles at healthcare organizations ranging from acute care hospitals and home health agencies to long-term care facilities and group medical practices. In addition to serving as a medical director of case management and medical necessity reviewer throughout his career, Dr. Hirsch has delivered numerous peer lectures on case management best practices and is a published author on the topic. He is a member of the American Case Management Association and a Fellow of the American College of Physicians.