When did Medicare start and why?
When did Medicare start and why? In July 1965, under the leadership of President Lyndon Johnson, Congress enacted Medicare under Title XVIII of the Social Security Act to provide health insurance to people age 65 and older, regardless of income or medical history. When did Medicare become law? July 30, 1965
What happens when you need both Medicare and Medicaid?
When you visit a facility that takes both coverages, Medicare pays first. Medicaid can pick up copays and coinsurance payments. Medicaid can give you assistance in paying your Medicare premiums. In most instances, if you have dual coverage through Medicare and Medicaid, you’ll automatically enroll in a Medicare Savings Program (MSP).
When did Medicare and Medicaid come in to effect?
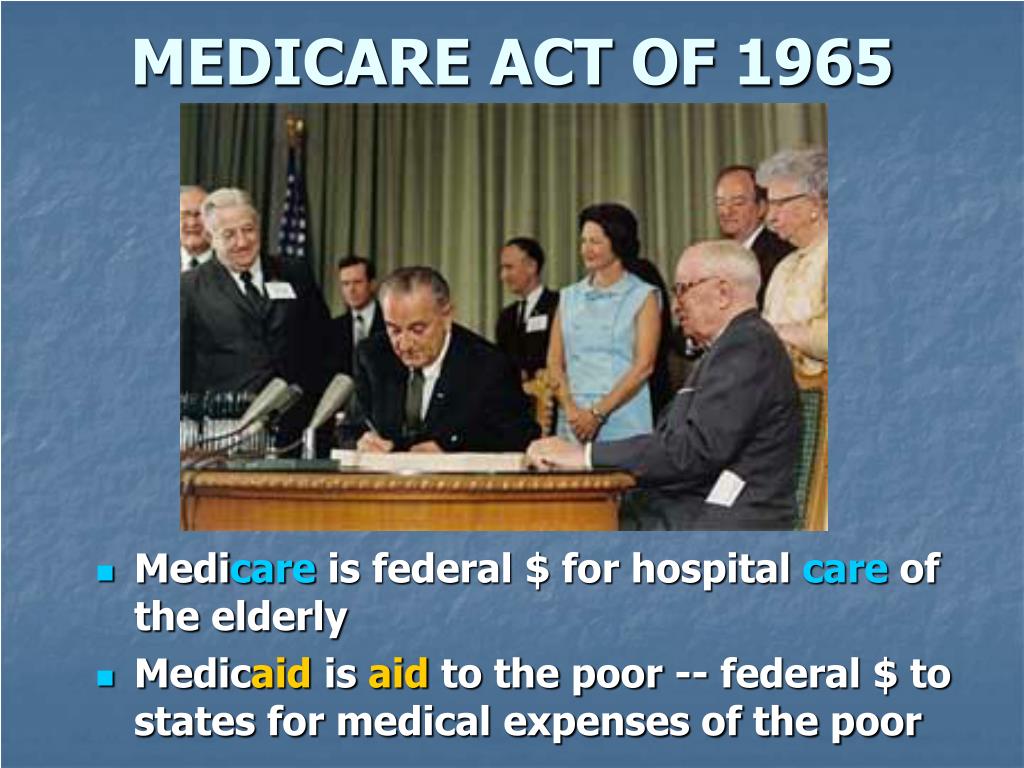
On July 30, 1965, President Lyndon B. Johnson signed into law legislation that established the Medicare and Medicaid programs. For 50 years, these programs have been protecting the health and well-being of millions of American families, saving lives, and improving the economic security of our nation.
Who started Medicare and Medicaid?
President Lyndon B. Johnson signed the bill creating Medicare and Medicaid in 1965, with former President Harry S. Truman, who had tried to establish national health insurance, seated at right. When it was created more than a half century ago, Medicaid almost escaped notice.

When did Medicare program start?
July 30, 1965On July 30, 1965, President Lyndon Johnson traveled to the Truman Library in Independence, Missouri, to sign Medicare into law. His gesture drew attention to the 20 years it had taken Congress to enact government health insurance for senior citizens after Harry Truman had proposed it.
Were Medicare and Medicaid created at the same time?
On July 30, 1965, President Lyndon B. Johnson signed into law the Social Security Act Amendments, popularly known as the Medicare bill. It established Medicare, a health insurance program for the elderly, and Medicaid, a health insurance program for the poor.
When and why was Medicare created?
The Medicare program was signed into law in 1965 to provide health coverage and increased financial security for older Americans who were not well served in an insurance market characterized by employment-linked group coverage.
What program brought the US Medicare and Medicaid?
On July 30, 1965, President Lyndon B. Johnson signed the Social Security Amendments of 1965 into law. With his signature he created Medicare and Medicaid, which became two of America's most enduring social programs.
Why was 1965 such an important year for policy issues?
On July 30, 1965, President Lyndon B. Johnson signed into law legislation that established the Medicare and Medicaid programs. For 50 years, these programs have been protecting the health and well-being of millions of American families, saving lives, and improving the economic security of our nation.
What was Medicaid in the 1960s?
In 1965, the passage of the Social Security Amendments, popularly known as Medicare and Medicaid, resulted in one basic program of health insurance for persons aged 65 and older, and another program providing health insurance for people with limited income funded by state and federal sources, respectively.
When Medicare was created in 1966 which individual was entitled to the program?
a comprehensive federal insurance program was established by congress in 1966 to give people 65 years and older financial assistance with medical expenses.
When did Medicare become effective?
1966In 1966, Medicare's coverage took effect, as Americans age 65 and older were enrolled in Part A and millions of other seniors signed up for Part B. Nineteen million individuals signed up for Medicare during its first year.
Who was the first person to enroll in Medicare?
At the bill-signing ceremony President Johnson enrolled President Truman as the first Medicare beneficiary and presented him with the first Medicare card. This is President Truman's application for the optional Part B medical care coverage, which President Johnson signed as a witness.
Why did the American medical Association oppose Medicare in the 1950s and 1960s?
Said Edward Annis, MD, the AMA president who led the anti-Medicare fight in the early 1960s, "The AMA believed that anybody in this nation who needed medical care should have it when they need it for as long as they need it, whether they could pay for it or not." He and others of like mind predicted Medicare would be a ...
Which president started Social Security and Medicare?
Meeting this need of the aged was given top priority by President Lyndon B. Johnson's Administration, and a year and a half after he took office this objective was achieved when a new program, "Medicare," was established by the 1965 amendments to the social security program.
Who created the CHIP program?
On April 8, 1997, Senators Kennedy and Hatch introduced S. 525, the “Child Health Insurance and Lower Deficit Act (CHILD). This legislation amended the Public Health Service Act to create a new grant program for states to purchase private health insurance for children.
When did Medicare become assured?
Even as the passage of Medicare became assured late in 1964 and in 1965, the legislation remained fluid, with important matters related to consumer choice and the basic design of the program in constant flux. Changing Concepts of Health Insurance. Progressive Era.
How many people had health insurance in 1940?
More than one-half of the hospital patients in America entered with some form of health insurance (the percentage had been 9 percent in 1940); in that same year, more than 40 million people had some form of private insurance to pay for doctors' bills.
What was the cost of medical care in 1911?
Rubinow (1916)cited a 1911 American study conducted for the Commission on Industrial Diseases that showed the amount of lost wages as $366 million and the expenses for medical care as $285 million. Hence, what later came to be called temporary disability insurance took precedence over health insurance.
What would happen if national health insurance had passed?
If national health insurance had passed in this era, it would have provided health care for people of all ages (Poen, 1979). National health insurance, which formerly had been linked with the States and the unemployment insurance program, now became associated with the old-age insurance or the Social Security program.
Why was social reform not on the Federal Government?
At the time, the focus of social reform was on the State and not the Federal Government for reasons related to the weight of precedent, the constitutional constraints on Federal activity, and the heterogeneous conditions across the American continent.
When did Javits and Lindsay's ideas become part of the Social Security bill?
Both Javits' and Lindsay's ideas were incorporated in the administration's Social Security proposals at the end of 1964 and the beginning of 1965. The Javits “complementary private insurance” notion remained in the bill that the administration presented to Congress in 1965.
When did Lyndon Johnson sign the Social Security Act?
Copyright notice. This article has been cited byother articles in PMC. Abstract. On July 30 , 1965 , President Lyndon B. Johnson signed the Social Security Amendments of 1965 into law. With his signature he created Medicare and Medicaid, which became two of America's most enduring social programs. The signing ceremony took place in Independence, ...
When did medicaid become law?
Authorized by Title XIX of the Social Security Act, Medicaid was signed into law in 1965 alongside Medicare. All states, the District of Columbia, and the U.S. territories have Medicaid programs designed to provide health coverage for low-income people. Although the Federal government establishes certain parameters for all states to follow, each state administers their Medicaid program differently, resulting in variations in Medicaid coverage across the country.
When did the Affordable Care Act start?
Affordable Care Act. Beginning in 2014, the Affordable Care Act provides states the authority to expand Medicaid eligibility to individuals under age 65 in families with incomes below 133 percent of the Federal Poverty Level (FPL) and standardizes the rules for determining eligibility and providing benefits through Medicaid, ...
What is the basic health program?
The Basic Health Program was enacted by the Affordable Care Act and provides states the option to establish health benefits cover programs for low-income residents who would otherwise be eligible to purchase coverage through the Health Insurance Marketplace, providing affordable coverage and better continuity of care for people whose income fluctuates above and below Medicaid and CHIP levels.
How much of the federal poverty level is covered by CHIP?
All states have expanded children's coverage significantly through their CHIP programs, with nearly every state providing coverage for children up to at least 200 percent of the Federal Poverty Level (FPL).
When will Medicaid phase down?
Beginning in 2014 coverage for the newly eligible adults will be fully funded by the federal government for three years. It will phase down to 90% by 2020.
When did the Children's Health Insurance Program start?
Children's Health Insurance Program. The Children's Health Insurance Program (CHIP) was signed into law in 1997 and provides federal matching funds to states to provide health coverage to children in families with incomes too high to qualify for Medicaid, but who can't afford private coverage. All states have expanded children's coverage ...
What is CMCS in health care?
The Center for Medicaid and CHIP Services (CMCS) serves as the focal point for all national program policies and operations related to Medicaid, the Children's Health Insurance Program (CHIP), and the Basic Health Program (BHP). These critical health coverage programs serve millions of families, children, pregnant women, adults without children, ...
Teach with this document
This document is available on DocsTeach, the online tool for teaching with documents from the National Archives. Find teaching activities that incorporate this document, or create your own online activity.
Transcript
To provide a hospital insurance program for the aged under the Social Security Act with a supplementary medical benefits program and an extended program of medical assistance, to increase benefits under the Old-Age, Survivors, and Disability Insurance System, to improve the Federal-State public assistance programs, and for other purposes.
When did Medicare start?
But it wasn’t until after 1966 – after legislation was signed by President Lyndon B Johnson in 1965 – that Americans started receiving Medicare health coverage when Medicare’s hospital and medical insurance benefits first took effect. Harry Truman and his wife, Bess, were the first two Medicare beneficiaries.
When did Medicare expand home health?
When Congress passed the Omnibus Reconciliation Act of 1980 , it expanded home health services. The bill also brought Medigap – or Medicare supplement insurance – under federal oversight. In 1982, hospice services for the terminally ill were added to a growing list of Medicare benefits.
How much was Medicare in 1965?
In 1965, the budget for Medicare was around $10 billion. In 1966, Medicare’s coverage took effect, as Americans age 65 and older were enrolled in Part A and millions of other seniors signed up for Part B. Nineteen million individuals signed up for Medicare during its first year. The ’70s.
How much will Medicare be spent in 2028?
Medicare spending projections fluctuate with time, but as of 2018, Medicare spending was expected to account for 18 percent of total federal spending by 2028, up from 15 percent in 2017. And the Medicare Part A trust fund was expected to be depleted by 2026.
What is the Patient Protection and Affordable Care Act?
The Patient Protection and Affordable Care Act of 2010 includes a long list of reform provisions intended to contain Medicare costs while increasing revenue, improving and streamlining its delivery systems, and even increasing services to the program.
How many people will have Medicare in 2021?
As of 2021, 63.1 million Americans had coverage through Medicare. Medicare spending is expected to account for 18% of total federal spending by 2028. Medicare per-capita spending grew at a slower pace between 2010 and 2017. Discussion about a national health insurance system for Americans goes all the way back to the days ...
What was Truman's plan for Medicare?
The plan Truman envisioned would provide health coverage to individuals, paying for such typical expenses as doctor visits, hospital visits, ...
Abstract
Editor's Note: As a follow-up to the precedinarticle first published in the October 1965 issue (see page 461), Richard G. Frank, Ph.D., offers an analysis of the evolving Medicare and Medicaid programs and their impact on public mental health care.
The programs
The Medicare program was created under title 18 of the Social Security Act. Elderly and some disabled beneficiaries (those enrolled in Social Security Disability Insurance) are automatically enrolled in part A of Medicare, which pays for hospital care.
Medicare, Medicaid, and the economics of mental health care
The creation of the Medicare and Medicaid programs served to put into motion a set of forces that would encourage the emergence of markets for mental health care and the privatization of mental health service delivery. It would also, in the coming years, repeatedly raise the issue of exceptionalism for mental health.
Parity
Parity today is often argued in terms of equalization of the rules used to cover and pay for general medical and mental health services. In practice the application of the idea of parity often involves a more complicated set of criteria. The development of the Medicare program illustrates this point.
The policy impacts today
The mental health community understood that the creation of Medicare and Medicaid would be important for psychiatry and the larger society. What was less well understood was the impact that these policies would have on the structure of the delivery system and the role of government in mental health care.
Acknowledgments
The author gratefully acknowledges financial support from the John D. and Catherine T. MacArthur Foundation. He thanks Nicole Pignatiello for excellent research assistance and Haiden Huskamp, Ph.D., for helpful comments.
When did Medicare Part D start?
Medicare Part D went into effect on January 1, 2006. Anyone with Part A or B is eligible for Part D, which covers mostly self-administered drugs. It was made possible by the passage of the Medicare Modernization Act of 2003. To receive this benefit, a person with Medicare must enroll in a stand-alone Prescription Drug Plan (PDP) or public Part C health plan with integrated prescription drug coverage (MA-PD). These plans are approved and regulated by the Medicare program, but are actually designed and administered by various sponsors including charities, integrated health delivery systems, unions and health insurance companies; almost all these sponsors in turn use pharmacy benefit managers in the same way as they are used by sponsors of health insurance for those not on Medicare. Unlike Original Medicare (Part A and B), Part D coverage is not standardized (though it is highly regulated by the Centers for Medicare and Medicaid Services). Plans choose which drugs they wish to cover (but must cover at least two drugs in 148 different categories and cover all or "substantially all" drugs in the following protected classes of drugs: anti-cancer; anti-psychotic; anti-convulsant, anti-depressants, immuno-suppressant, and HIV and AIDS drugs). The plans can also specify with CMS approval at what level (or tier) they wish to cover it, and are encouraged to use step therapy. Some drugs are excluded from coverage altogether and Part D plans that cover excluded drugs are not allowed to pass those costs on to Medicare, and plans are required to repay CMS if they are found to have billed Medicare in these cases.
When did Medicare+Choice become Medicare Advantage?
These Part C plans were initially known in 1997 as "Medicare+Choice". As of the Medicare Modernization Act of 2003, most "Medicare+Choice" plans were re-branded as " Medicare Advantage " (MA) plans (though MA is a government term and might not even be "visible" to the Part C health plan beneficiary).
What is CMS in healthcare?
The Centers for Medicare and Medicaid Services (CMS), a component of the U.S. Department of Health and Human Services (HHS), administers Medicare, Medicaid, the Children's Health Insurance Program (CHIP), the Clinical Laboratory Improvement Amendments (CLIA), and parts of the Affordable Care Act (ACA) ("Obamacare").
How much does Medicare cost in 2020?
In 2020, US federal government spending on Medicare was $776.2 billion.
What is Medicare and Medicaid?
Medicare is a national health insurance program in the United States, begun in 1965 under the Social Security Administration (SSA) and now administered by the Centers for Medicare and Medicaid Services (CMS). It primarily provides health insurance for Americans aged 65 and older, ...
How is Medicare funded?
Medicare is funded by a combination of a specific payroll tax, beneficiary premiums, and surtaxes from beneficiaries, co-pays and deductibles, and general U.S. Treasury revenue. Medicare is divided into four Parts: A, B, C and D.
How many people have Medicare?
In 2018, according to the 2019 Medicare Trustees Report, Medicare provided health insurance for over 59.9 million individuals —more than 52 million people aged 65 and older and about 8 million younger people.
When did Medicare Part D become law?
On December 8, 2003 the bill became law. On January 21, 2005 CMS established the final rules.
When did HMOs get Medicare?
The Health Maintenance Organization (HMO) Act of 1973 authorized federal Medicare payments to HMOs. In 1982, the Tax Equity and Fiscal Responsibility Act created a more meaningful alliance with Medicare making it more attractive for HMOs to contract with Medicare.
What are the changes to Medicare?
The Medicare Prescription Drug Improvement and Modernization Act of 2003 (MMA 2003), signed by President George W. Bush, resulted in the most significant changes to Medicare since the program’s inception. The act preserved and strengthened the Original Medicare program, added preventive benefits, and provided extra help to people with low income and limited assets. In addition to significant material changes affecting the program and benefits, a number of other nomenclature adjustments were made: 1 The traditional fee-for-service Medicare program, consisting of Part A and Part B, was renamed Original Medicare; 2 The Medicare Part C program, Medicare + Choice, was renamed Medicare Advantage (MA), which greatly expanded choices of private health plans to Medicare beneficiaries; 3 And, for the first time, a new voluntary outpatient prescription drug plan benefit was introduced under the name Medicare Part D (PDP).
What was the Social Security Amendment?
On July 30, 1965, as part of his “Great Society” program, President Lyndon B. Johnson signed into law the Social Security Amendment of 1965. This new law established the Medicare and Medicaid programs, which were designed to deliver health care benefits to the elderly and the poor.
What is Medicare Part C?
Medicare Part C, also know as Medicare Advantage, serves as an alternative to traditional Part A and Part B coverage. Under the Part C option, beneficiaries can chose to enroll in a Medicare Advantage plan and receive care from a private insurance company that contracts with Medicare.
How many people are covered by Medicare?
Currently, Medicare covers 47 million people, including 30 million people age 65 and older and 8 million people under age 65 with a permanent disability. Medicare is a social insurance program, like Social Security, that offers health coverage to eligible individuals, regardless of income or health status.
When did Medicare expand to include Lou Gehrig's disease?
In 2001, eligibility expanded further to cover people with Lou Gehrig’s disease. The Medicare program has two components: Hospital Insurance ...
