
When did hospice care become part of Medicaid?
In 1986, the Medicare Hospice Benefit was enacted, and states were given the option to include hospice in their Medicaid programs. Hospice care was made available to terminally ill nursing home residents as well.
Does Medicare Advantage cover hospice care?
Once you start getting hospice care, your hospice benefit should cover everything you need related to your terminal illness, even if you remain in a Medicare Advantage Plan (like an HMO or PPO) or other Medicare health plan. After your hospice benefit starts, you can still get covered services for conditions not related to your terminal illness.
Does the Omnibus Reconciliation Act (Obra 1990) cover hospice?
Passage of the Omnibus Reconciliation Act (OBRA 1990) establishes an unlimited fourth election period for the Medicare Hospice Benefit (final rule published 6/12/91). The Commission on the Future Structure of Veterans Health Care (Mission Commission) releases a report recommending inclusion of hospice care in the veteran’s benefit package.
When does hospice care start and end?
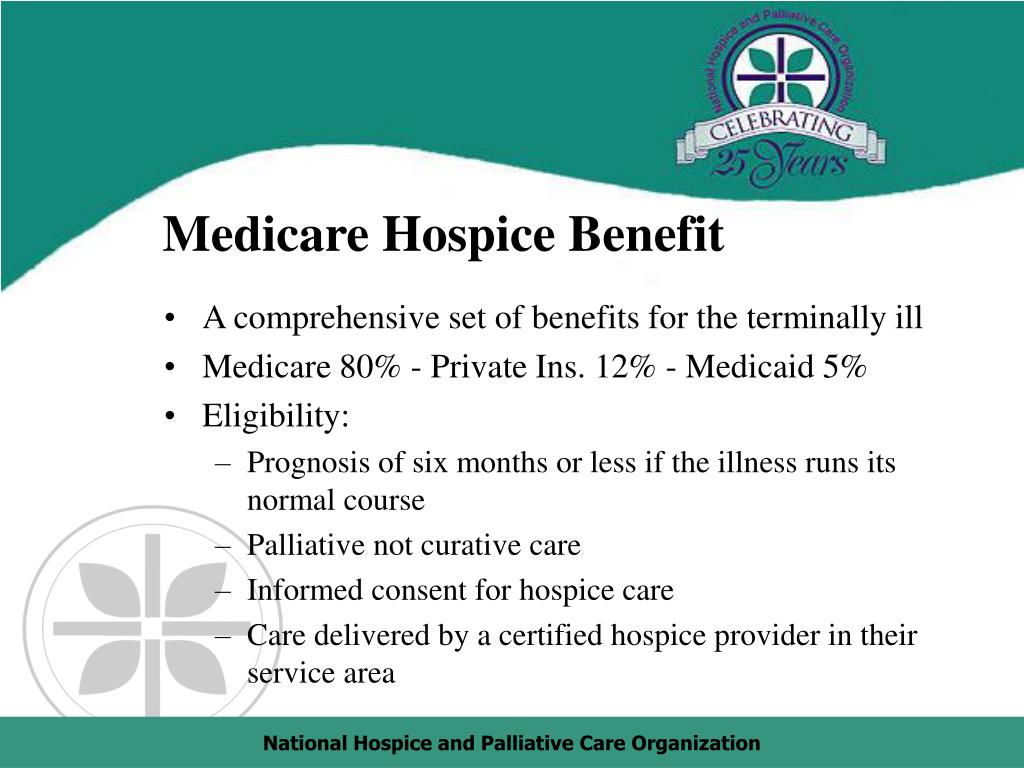
A benefit period starts the day you begin to get hospice care, and it ends when your 90-day or 60-day benefit period ends. At the start of the first 90-day benefit period, your hospice doctor and your regular doctor (if you have one) must certify that you’re terminally ill (with a life expectancy of 6 months or less).
When did hospice care become a standard of care?
19931993. Hospice is included as a nationally guaranteed benefit under President Clinton's health care reform proposal.
When did end of life care begin?
Palliative care got its start as hospice care, often delivered by caregivers at religious institutions. Dame Cicely Saunders, a British physician, founded the first formal hospice in 1948 specifically to care for patients with terminal illnesses.
When did the hospice movement start?
1967The modern hospice movement started in the UK in 1967 under the impulse of Cicely Saunders. She introduced a holistic person-centred approach to end-of-life care, aiming to address patients' physical, psychological and spiritual needs (Milićević, 2002) .
When did hospice start in USA?
1970sThese symptoms can be physical, emotional, spiritual or social in nature. The concept of hospice as a place to treat the incurably ill has been evolving since the 11th century. Hospice care was introduced to the United States in the 1970s in response to the work of Cicely Saunders in the United Kingdom.
Who started the hospice movement?
Dame Cicely SaundersDame Cicely Saunders died peacefully on Thursday 14 July 2005 at St Christopher's Hospice in south London, the world-famous hospice that she founded in the 1960s, and the birthplace of the modern hospice movement.
When did the term palliative care start?
In 1973, Balfour Mount, a urological surgeon from Canada, visited. He went back and founded a unit in his hospital, the Royal Victoria Hospital in Montreal, and he gave the name 'Palliative Care' to our specialty.
Why did the hospice movement start?
The inspiration for the modern hospice came from Dame Cicely Saunders. She had started work as a volunteer nurse in 1948 and, over the next decade, trained as a doctor to understand the issues surrounding care of the dying.
Has hospice care changed over the past several decades?
Has hospice care changed over the past several decades? No, hospice care has increasingly relied on intensive, high-tech medical procedures.
Who started the first hospice in the US?
Florence WaldFlorence Wald, whose vision of bringing the terminally ill peace of mind and, to whatever extent possible, freedom from pain led to the opening of the first U.S. palliative-care hospice, died Nov. 8 at her Branford, Conn., home. She was 91.
Is hospice care free in the USA?
Patients with a terminal illness do not usually have to pay for hospice care. Currently, most hospice patients have their costs covered by Medicare, through the Medicare Hospice Benefit. Learn more about the Medicare Hospice Benefit. Medicaid also pays for hospice care in most states.
How has hospice changed over the years?
Consistent with reports regarding the increase in the number of for-profit hospices in the U.S. in the past decade,1,18 the number of individuals cared for by for-profit hospices more than tripled while the increase in the number of individuals cared for by nonprofit hospices increased 49% during the past decade.
What is the difference between end of life care and palliative care?
Palliative care is available when you first learn you have a life-limiting (terminal) illness. You might be able to receive palliative care while you are still receiving other therapies to treat your condition. End of life care is a form of palliative care you receive when you're close to the end of life.
When did the shift in the scene of death from home to hospital began?
During the 1900s, the focus of medicine began to shift from only being able to provide comfort measures to curing the underlying disease. Significant advancements in medicine, education, and technology occurred during this century and this affected the way that death was viewed.
How do doctors know how long you have left to live?
There are numerous measures – such as medical tests, physical exams and the patient's history – that can also be used to produce a statistical likelihood of surviving a specific length of time.
How do you know when death is hours away?
Skin of the knees, feet, and hands may become purplish, pale, grey, and blotchy or mottled. These changes usually signal that death will occur within days to hours.
What is hospice benefit?
Medicare Hospice Benefit. The Medicare Hospice Benefit was established in 1983 to provide Medicare beneficiaries with access to high-quality end-of-life care. Considered the model for quality care for people facing a life-limiting illness, hospice is a patient-centered, cost-effective philosophy of care that utilizes an interdisciplinary team ...
How many people received hospice care in 2016?
In 2016, an estimated 1.43 million patients received hospice services.
What is the center of hospice care?
At the center of hospice and palliative care is the belief that each of us has the right to die pain-free and with dignity, and that our families will receive the necessary support to allow us to do so.
Where do hospice patients receive care?
Patients may receive care at their place of residence (including their private residence, nursing home, or residential facility), a hospice inpatient facility, or an acute care hospital. The location of care may change depending on the nature of a patient’s disease progression, medical needs of the patient, as well as the plan of care established between the patient and the hospice. An interdisciplinary team of professionals is responsible for the care of each hospice patient, regardless of the patient’s setting. In 2014, 58.9 percent1 of hospice patients received care at their place of residence at the time of death.
How much did Medicare increase hospice reimbursement?
The passage of the Benefits Improvement and Protection Act of 2000 brings a five percent increase in the Medicare hospice reimbursement rates.
What was the National Hospice Foundation's public service campaign in 2000?
2000. The National Hospice Foundation launches a public service campaign of TV ads across the U.S. ; one of these ads wins the prestigious ADDY Award. U.S. Senate holds two major hearings on end-of-life care and discusses barriers to access under the Medicare hospice benefit.
How much is the NHPCO grant?
National Hospice and Palliative Care Organization celebrates its 25th anniversary. NHPCO gives a grant of $100,000 to the Veterans Health Administration to begin the Veterans Administration Hospice and Palliative Care (VAHPC) initiative.
What is the National Hospice Organization?
National Hospice Organization (NHO) is established to promote the concept of hospice care.
How long do hospice patients live?
Research published in the Journal of Pain and Symptom Management reports that hospice patients live an average of 29 days longer than similar patients who did not have hospice care.
Where are the hospice regulations published?
Initial Medicare Hospice Regulations are published in the Federal Register. Regulations establish the four levels of care and outline the cost components of the routine home care rate.
Where is the first symposium on hospice care?
The first National Symposium on Hospice Care is convened in New Haven, Connecticut.
When did the hospice payment reforms take effect?
Section 3132 of the Affordable Care Act of 2010 (ACA) provided the Secretary of HHS discretion to implement hospice payment reform after October 1, 2013. In the hospice notice of proposed rulemaking (NPRM) for FY 2016, CMS has proposed a change in hospice payment to better align the payment with the visit intensity profile ...
When was hospice established?
The Medicare hospice benefit was established in 1983 to provide palliative care and support services to terminally ill patients and their families. The benefit is intended for beneficiaries with a life expectancy of six months or less if the illness runs its normal course.
How many hospice patients use RHC?
As Table 6 indicates, RHC services are provided to most hospice enrollees while the other services are provided with substantially lower frequency. Overall, 87% of hospice episodes use RHC services, and 68% use only RHC services. Both CHC and IRC services are used with the lowest frequency across all diagnoses.
How many hospice episodes are there in a year?
The number of hospice episodes in a year has grown over time from over 400,000 in 2000 to 1.3 million in 2013. The start of a hospice episode is defined as the date of election and the end is defined as the date of death or live discharge. More importantly from the perspective of how the benefit is used, the percent of Medicare decedents who die in hospice care has more than doubled from 22% to 46% during those fiscal years (Table 3). The percent of decedents using hospice is slightly higher for beneficiaries enrolled in Medicare Advantage (MA) than for those in the traditional fee for service (FFS) program. When an MA beneficiary elects hospice care, the traditional Medicare program makes the payments to the hospice as well as covering any care unrelated to the terminal illness.
What does Medicare pay for hospice?
Once a Medicare beneficiary elects the hospice benefit, Medicare will pay for: 1) covered hospice services provided by a participating hospice and 2) other Medicare covered services unrelated to the terminal illness. There are four levels of hospice care each with a prospective per diem rate. The most common level of care provided is routine home care (RHC) which is provided on a typical day, and accounts for approximately 95% of all hospice days paid. Second, continuous home care (CHC) can be provided during a crisis. Third, inpatient respite care (IRC) enables a respite or break for the family or caregiver for a hospice patient at home. Fourth, general inpatient care (GIC) may be provided for a condition that cannot be treated in another setting. RHC, GIC and IRC levels of care are all paid at a constant per diem rate, regardless of whether services or visits are provided each day or the level of intensity provided by each visit discipline. The CHC per-diem payment level varies by the number of hours provided each day.
What is hospice benefit?
Hospiceprovides support for beneficiaries who may choose to die at home, surrounded by family andfriends.
How long did hospice episodes last in 2013?
By 2000, 54% of patients had diagnoses other than cancer, and in 2013 that number had grown to 74%. Mean episode length was 123 days in 2013 as compared with 76 days in 2000 (not in the Table). Alzheimer’s/dementia patients exhibit longer average stays; and a higher percent of these stays exceed 180 days relative to patients with other diagnoses.
What is hospice care?
hospice. A special way of caring for people who are terminally ill. Hospice care involves a team-oriented approach that addresses the medical, physical, social, emotional, and spiritual needs of the patient. Hospice also provides support to the patient's family or caregiver. care.
How long can you be in hospice care?
After 6 months , you can continue to get hospice care as long as the hospice medical director or hospice doctor recertifies (at a face-to-face meeting) that you’re still terminally ill. Hospice care is usually given in your home but may also be covered in a hospice inpatient facility. Original Medicare will still pay for covered benefits for any health problems that aren’t part of your terminal illness and related conditions, but this is unusual. When you choose hospice care, you decide you no longer want care to cure your terminal illness and/or your doctor determines that efforts to cure your illness aren't working. Once you choose hospice care, your hospice benefit will usually cover everything you need.
How long can you live in hospice?
Things to know. Only your hospice doctor and your regular doctor (if you have one) can certify that you’re terminally ill and have a life expectancy of 6 months or less. After 6 months, you can continue to get hospice care as long as the hospice medical director or hospice doctor recertifies ...
What happens when you choose hospice care?
When you choose hospice care, you decide you no longer want care to cure your terminal illness and/ or your doctor determines that efforts to cure your illness aren't working . Once you choose hospice care, your hospice benefit will usually cover everything you need.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. for inpatient respite care.
Can you stop hospice care?
As a hospice patient, you always have the right to stop hospice care at any time. Prescription drugs to cure your illness (rather than for symptom control or pain relief). Care from any hospice provider that wasn't set up by the hospice medical team. You must get hospice care from the hospice provider you chose.
Can you get hospice care from a different hospice?
You can't get the same type of hospice care from a different hospice, unless you change your hospice provider. However, you can still see your regular doctor or nurse practitioner if you've chosen him or her to be the attending medical professional who helps supervise your hospice care. Room and board.
How long can a hospice patient be on Medicare?
After certification, the patient may elect the hospice benefit for: Two 90-day periods followed by an unlimited number of subsequent 60-day periods.
What is hospice care?
Hospice is a comprehensive, holistic program of care and support for terminally ill patients and their families. Hospice care changes the focus to comfort care (palliative care) for pain relief and symptom management instead of care to cure the patient’s illness. Patients with Medicare Part A can get hospice care benefits if they meet ...
What is the coinsurance for respite care?
Respite Care Coinsurance: The patient’s daily coinsurance amount is 5% of the Medicare payment for a respite care day. The coinsurance amount may not be more than the inpatient hospital deductible for the year that the hospice coinsurance period began. This level of care includes room and board costs.
How many days does hospice respite last?
Inpatient respite care: A day the patient elects to get hospice care in an approved inpatient facility for up to 5 consecutive days to give their caregiver a rest.
How much is coinsurance for hospice?
The coinsurance amount is 5% of the cost of the drug or biological to the hospice, determined by the drug copayment schedule set by the hospice. The coinsurance for each prescription may not be more than $5.00. The patient does not owe any coinsurance when they got it during general inpatient care or respite care.
What is the life expectancy of a hospice patient?
The FTF encounter must document the clinical findings supporting a life expectancy of 6 months or less. All hospice care and services offered to patients and their families must follow an individualized written plan of care (POC) that meets the patient’s needs.
What is hospice coinsurance?
Drugs and Biologicals Coinsurance: Hospices provide drugs and biologicals to lessen and manage pain and symptoms of a patient’s terminal illness and related conditions. For each hospice-related palliative drug and biological prescription:
When was the first hospice in the US?
In 1974 , Florence Wald, two pediatricians, and a chaplain founded the first hospice in the US Connecticut Hospice in Branford, CT. That same year, Senators Frank Church and Frank E. Moss introduced legislation to provide federal funds for hospice programs. The legislation didn’t pass. It wasn’t until 1982 that Congress included a provision to create a Medicare hospice benefit as part of the Tax Equity and Fiscal Responsibility Act of 1982, but it contained a sundown provision for 1986.
Who was the first person to use hospice?
The modern usage of hospice as a place for and philosophy of end-of-life care began with the work of a British physician named Dame Cicely Saunders. Dr.
What is the name of the hospice organization in Connecticut?
In 2014, 40 years after the opening of Connecticut Hospice, the National Hospice and Palliative Care Organization (NHPCO) and its affiliates celebrated four decades of providing hospice care in the US.
Where does the word "hospice" come from?
The word ?hospice? derives from the Latin word hospes, which means both ?guest? and ?host.? Since the 11th century, the concept of hospice was adopted by the Roman Catholic tradition to refer to a place of hospitality for the sick and dying as well as for travelers and pilgrims.
Who introduced the idea of specialized care for the dying?
In 1963, during a talk at Yale University in the US, Dr. Saunders introduced the idea of specialized care for the dying, which centered on palliative care rather than treatments to cure. In the audience were doctors, nurses, chaplains, and medical students.
What is hospice care?
Background Hospice care is an approach to treatment that recognizes that the impending death of an individual warrants a change in focus from curative care to palliative care. The goal of hospice care is to help terminally ill individuals continue life with minimal disruption in normal activities while remaining primarily in the home environment. A hospice uses an interdisciplinary approach to deliver medical, social, psychological, emotional, and spiritual services through the use of a broad spectrum of professional and other care~givers with the goal of making the individual as physically and emotionally comfortable as possible. The hospice experience in the United States has placed emphasis on home care. It offers physician services, specialized nursing services, and other forms of care in the home in order to enable the terminally ill individual to remain at home in the company of family and friends as long as possible. Inpatient hospice settings have been used when the individual's pain and symptoms must be closely monitored in order to be controlled, when medical intervention is required to control pain or palliate symptoms, or when the family. needs a rest from the tedium and stress involved in caring for the individual (respite care). Section 122 of the Tax Equity and Fiscal Responsibility Act (TEFRA) of 1982 (Pub. L. 97-248, enacted on September 3, 1982) expanded the scope of Medicare benefits by authorizing coverage for hospice care for terminally
Do hospices have to be waivers?
individual makes it necessary for these decisions to be made on a case by case basis. It is our general view that the waiver required by the law is a broad one and that hospices are required to provide virtually all the care that is needed by terminally ill patients.. The example that we provided in the .proposed.regulation of a hospice's
Does hospice require 24-hour care?
Response: Although the statute requires that a hospice make all covered services available as needed on a 24- hour basis (section 1861(dd)(2)(A)(i) of the Act), we agree that the availability of certain items is especially critical and will modify the regulations at § 418.50(b) to enumerate the basic services (nursing services, physician services, and drugs and biologicals) that a hospice must routinely make available on a 24-hour a day basis. We expect that the physician available would be empowered to authorize provision of services not specified in the plan of care (for example, provision of emergency services or an unanticipated admission for inpatient care). We will continue to require that a hospice provide all other services on a 24-hour basis to the extent necessary to meet the needs of its patients but recognize that this may not be a frequent need.
Can hospices discharge terminally ill patients?
benefits had not been exhausted. Comment: Several commenters suggested that provision should be made for hospices to discharge terminally ill patients from a hospice program when their physical condition or domestic circumstances are altered in such a way that they would no longer be considered acceptable patients under the hospice's admission criteria. For example, it was suggested that if a hospice has a patient who develops unexpectedly the need for long-term inpatient care or a patient who had upon admission but no longer has a primary caregiver, the hospice could discharge the patient. Response: We do not agree with the view expressed by these commenters. A patient whose circumstances cause him or her to desire a different type of care may revoke a hospice election. However, a hospiCe may not discharge, at its discretion, a patient whose care promises to be costly or inconvenient. Once a hospice chooses to admit a Medicare beneficiary, it may not discharge the patient. If the hospice finds that the patient is no longer terminally ill, the hospice will be unable to recertify the patient and the patient
Can hospice be exclusively engaged in providing care to terminally ill patients?
The commenter recommended that the regulations state that the hospice be "exclusively" engaged in providing care to the terminally ill.
Do hospices need a physician?
was noted that a physician is needed primarily for the medical component of a hospice program not the administrative component, and that medical direction should be limited to this area.
Does a hospice have a plan of care?
Response: We accepted the comment concerning the use of a designee by the medical director and the regulations will reflect this change. We would note that a plan of care is a changing document, however, and that a hospice may choose to develop a relatively brief plan of care upon admission and revise and update it

1963
- Dame Cicely Saunders introduces the idea of specialized care for the dying to the United States in a lecture at Yale University.
1965
- Florence Wald, Dean of the Yale School of Nursing, invites Dame Cicely Saunders to become a visiting faculty member.
1969
- On Death and Dying, written by Dr. Elisabeth Kubler-Ross, identifies the five stages through which many terminally ill patients progress.
1972
- Elisabeth Kubler-Ross testifies at the first national hearings on the subject of death with dignity, conducted by the U.S. Senate Special Committee on Aging.
1974
- Florence Wald, along with two pediatricians and a chaplain, founds Connecticut Hospice in Branford, Connecticut.
- The first hospice legislation is introduced by Senators Frank Church and Frank E. Moss to provide federal funds for hospice programs. The legislation is not enacted.
1977
- The second National Symposium on Hospice Care is convened in Boonton, New Jersey.
- The third Symposium on Hospice Care is convened in Marin County, California.
1978
- National Hospice Organization (NHO) is established to promote the concept of hospice care.
- The first national NHO conference with 1000 participants is held in Washington, DC in October.
- A U.S. Department of Health, Education, and Welfare task force reports that “the hospice movement …… is a viable concept and one which holds out a means of providing more humane care for Americans...
1979
- The Health Care Financing Administration (HCFA) initiates demonstration programs at 26 hospices in 16 states to assess the cost effectiveness of hospice care and to help determine what a hospice is...
- NHO issues the first “Standards of a Hospice Program of Care,” adopted by the NHO Board of Directors in February.
- The Health Care Financing Administration (HCFA) initiates demonstration programs at 26 hospices in 16 states to assess the cost effectiveness of hospice care and to help determine what a hospice is...
- NHO issues the first “Standards of a Hospice Program of Care,” adopted by the NHO Board of Directors in February.
- Cicely Saunders is made a Dame of the British Empire.
- First hospice program established in Africa: Island Hospice, Harare, Zimbabwe.
1980
- Josefina Magno, MD, serves as the first full-time Executive Director/President of NHO. (1980 – 1982)
- The W.K. Kellogg Foundation awards a grant to the Joint Commission on Accreditation of Hospitals (JCAHO) to investigate the status of hospice and to develop standards for accreditation.
1981
- Logo is officially registered as the property of the National Hospice Organization.
- The National Hospice Education Project is set up for the sole purpose of passing Medicare hospice legislation.
- First AIDS case is defined.