Full Answer
Does Medicare share information with ACOs?
Medicare will share certain health information with ACOs working with your doctors and other health care providers about your care. The poster in your doctor’s office (or written notice) should let you know whether the doctor or ACO has asked Medicare for access to your information about the care you get through Medicare.
What is the difference between Original Medicare and ACO Medicare?
If your primary care provider participates in an ACO and you have Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance).
How much could the ACO model reduce Medicare spending?
It is estimated that the ACO model could reduce Medicare spending by up to $940 million within the first four years alone.
Do ACOs have financial accountability for Medicaid enrollees?
In current Medicare ACO initiatives, beneficiaries who are Medicare-Medicaid enrollees (also known as “dual eligible beneficiaries”) may be attributed to ACOs. Current Medicare ACOs, however, often do not have financial accountability for the Medicaid expenditures for those beneficiaries.
What is an ACO?
Accountable Care Organizations (ACOs) are one way that we’re working to better coordinate your care. If your doctor has decided to participate in an ACO and you have. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share ...
Can you be assigned to an ACO?
Only people with Original Medicare can be assigned to an ACO. You can’t be assigned to an ACO if you have a. Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice.
Can Medicare be paid by ACO?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. , like an HMO or a PPO. An ACO can't tell you which health care providers to see and can't change your Medicare. benefits.
Does Medicare share information with ACOs?
Medicare will share certain health information with ACOs working with your doctors and other health care providers about your care. The poster in your doctor’s office (or written notice) should let you know whether the doctor or ACO has asked Medicare for access to your information about the care you get through Medicare.
When did ACO start receiving Medicare?
Under the ACO Investment Model, ACOs that began participating in the Medicare Shared Savings Program on April 1, 2012, July 1, 2012, January 1, 2013, or January 1, 2014 will receive two types of payments: An upfront, variable payment: Each ACO receives a payment based on the number of its preliminarily prospectively-assigned beneficiaries.
When did ACO join the Shared Savings Program?
ACOs that joined the Shared Savings Program starting in 2012, 2013 or 2014. Here, the ACO Investment Model will help ACOs succeed in the Shared Savings Program and encourage progression to higher levels of financial risk, ultimately improving care for beneficiaries and generating Medicare savings.
What is ACO investment model?
The ACO Investment Model is an initiative developed by the Center for Medicare & Medicaid Innovation (Innovation Center) designed for organizations participating as ACOs in the Medicare Shared Savings Program (Shared Savings Program).
Does CMS give preference to ACOs?
CMS will also give preference to ACOs that provide high quality of care, ACOs that achieved their financial benchmark, ACOs that demonstrate exceptional financial need, and those that submit compelling proposals for how they will invest both their own funds and CMS funds.
Is a hospital considered an ACO?
The ACO does not include a hospital as an ACO participant or an ACO provider/supplier (as defined by the Shared Savings Program regulations), unless the hospital is a critical access hospital (CAH) or inpatient prospective payment system (IPPS) hospital with 100 or fewer beds.
Is ACO owned by a health plan?
The ACO is not owned or operated in whole or in part by a health plan. The ACO did not participate in the Advance Payment Model. During the selection process, the ACO Investment Model will target new ACOs serving rural areas and areas of low ACO penetration and existing ACOs committed to moving to higher risk tracks.
Why is Medicare important for ACOs?
As the U.S. progresses in to the long-anticipated era when the baby boomer generation enters retirement, the entire nation worries about how the country will support its skyrocketing elderly and disabled population.
How long does an ACO have to provide care?
Under the new Affordable Care Act, each ACO is required to provide care for at least 5,000 Medicare patients for a minimum of three years. It is estimated that the ACO model could reduce Medicare spending by up to $940 million within the first four years alone.
What are the rewards of ACOs?
In other words, ACOs are provided financial rewards if they keep their patients healthy.
What is an ACO patient?
An ACO's patient population primarily consists of Medicare beneficiaries. In larger and more integrated ACOs, the patient population may also include homeless and uninsured people. Patients may play a role in the healthcare they receive by participating in their ACO's decision-making processes.
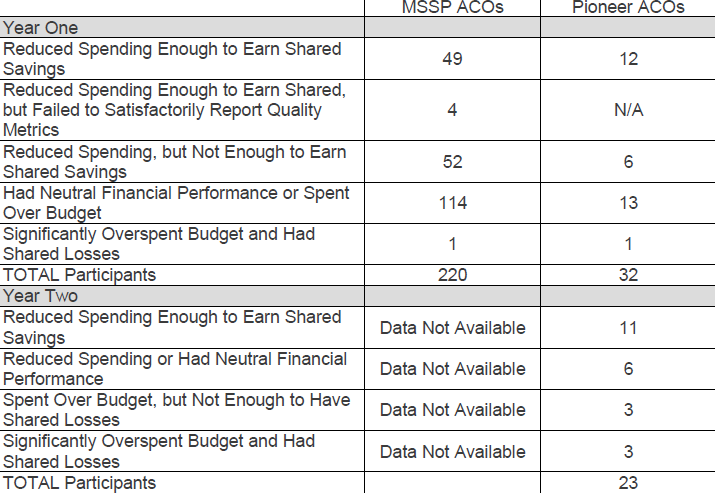
How much did Pioneer ACOs grow in 2012?
According to them, costs for more than 669,000 beneficiaries served by Pioneer ACOs grew by 0.3 percent in 2012. Costs for similar beneficiaries grew by 0.8 percent in the same period.
How long is the Medicare Shared Savings Program?
The Medicare Shared Savings Program is a three-year program during which ACOs accept responsibility for the overall quality, cost and care of a defined group of Medicare Fee-For-Services (FFS) beneficiaries. Under the program, ACOs are accountable for a minimum of 5,000 beneficiaries.
How does ACO work?
The model places a degree of financial responsibility on providers in hopes of improving care management and limiting unnecessary expenditures, while providing patients freedom to select their medical service providers. The ACO's model of fostering clinical excellence while simultaneously controlling costs depends on its ability to "incentivize hospitals, physicians, post-acute care facilities, and other providers involved to form linkages and facilitate coordination of care delivery". By increasing care coordination, ACOs were proposed to reduce unnecessary medical care and improve health outcomes, reducing utilization of acute care services. According to CMS estimates, ACO implementation as described in the Affordable Care Act was estimated to lead to an estimated median savings of $470 million from 2012–2015.
What is accountable care system?
An accountable care organization ( ACO) is a healthcare organization that ties provider reimbursements to quality metrics and reductions in the cost of care. ACOs in the United States are formed from a group of coordinated health-care practitioners.
What are the problems with ACOs?
Problems. ACOs have the potential to improve quality of care while reducing healthcare spending in a nation with high health expenditures. However, several challenges may affect the implementation and development of ACOs. First, there is a lack of specificity regarding how ACOs should be implemented.
What is an ACO?
t. e. An accountable care organization ( ACO) is a healthcare organization that ties provider reimbursements to quality metrics and reductions in the cost of care. ACOs in the United States are formed from a group of coordinated health-care practitioners. They use alternative payment models, normally, capitation.
What is an ACO in Medicare?
3022. An ACO, which can include primary care physicians, specialists, hospitals or other providers, bears responsibility jointly for the cost and quality of care delivered to a subset of Original Medicare beneficiaries. If they hit the quality targets, any savings that result are then shared among the providers, on that same token if they miss targets they can end up owing money back to Medicare.
How do ACOs get paid?
ACOs get paid based on their patients’ medical outcomes rather than on how many tests and procedures they perform. Under the Pioneer model ACOs are paid at fee-for-service rates, but then can earn payments or have to pay-back money based on patient outcomes.
When is Pioneer Model authorized?
The Pioneer Model is currently authorized through 2016 and offers an even greater transfer of risk than track 2 of MSSP. The expansion of the Pioneer Model would create an additional option for ACOs that would also require providers to accept risk.
What is PPACA Title II Part III?
PPACA Title II Part III also includes other pilot programs and innovations for new patient care models aimed at improving quality of care and keeping costs down. See a full summary of all PPACA provisions here.
What is the purpose of ACOs?
The goal of ACOs is to save Medicare money by having doctors and hospitals work together to coordinate patients’ care . Medicare hoped to save $5 billion by 2019 with the help of ACOs. They fell short of that goal, and now the Trump administration is reevaluating the necessity of ACOs.
Who is the administrator of CMS?
Seema Verma, administrator for the Centers for Medicare and Medicaid Services (CMS), said it’s wrong to have some ACOs that don’t take any blame when they fall short of their targets. “We want to put the accountability back into accountable care organizations,” she said.