When did Medicare Supplement plans became standardized?
The 1990 Medigap reform legislation sought to make it easier for consumers to compare policies, provide market stability, promote competition, and avoid adverse selection. Evidence is that the standardization of benefits has simplified consumer choice and is strongly supported by consumers and State regulators.
When were the older Medicare Supplement plans no longer for sale?
January 1, 2020As of January 1, 2020, Medigap plans sold to people new to Medicare can no longer cover the Part B deductible. Because of this, Plans C and F are no longer available to people new to Medicare on or after January 1, 2020.
Is Medicare supplemental required?
For many low-income Medicare beneficiaries, there's no need for private supplemental coverage. Only 19% of Original Medicare beneficiaries have no supplemental coverage. Supplemental coverage can help prevent major expenses.
What states do not offer Medicare Supplement plans?
Medigap plans are standardized across most states, meaning they offer the same benefits. The exceptions are Wisconsin, Minnesota and Massachusetts.
Is Plan F still available in 2022?
Once the annual deductible is met, the plan pays 100% of covered services for the rest of the year. The high-deductible Plan F is not available to new beneficiaries who became eligible for Medicare on or after January 1, 2020. 2 Plan K has an out-of-pocket yearly limit of $6,620 in 2022.Nov 18, 2021
When can I change my Medicare Supplement plan for 2022?
Yes, at any time you can switch from a Medicare Advantage to a Medicare Supplement plan. You have 12 months from when you first enrolled in an Advantage plan to switch back to Original Medicare and pick up a Medigap plan with Guaranteed Issue.
Who regulates Medicare Supplement plans?
Medicare Supplement plans are standardized and offer various benefits to help offset your healthcare cost. The California Department of Insurance (CDI) regulates Medicare Supplement policies underwritten by licensed insurance companies.
What states allow you to change Medicare Supplement plans without underwriting?
In some states, there are rules that allow you to change Medicare supplement plans without underwriting. This includes California, Washington, Oregon, Missouri and a couple others. Call us for details on when you can change your plan in that state to take advantage of the “no underwriting” rules.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
What are the disadvantages to a Medicare Advantage plan?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan; if you decide to switch to Medigap, there often are lifetime penalties.
Is Medigap plan G guaranteed issue?
Medigap Plan G is only available as a guaranteed issue plan to people who became eligible for Medicare on or after January 1st, 2020. You may still apply for Medigap Plan G through the usual methods (link to article) if you entered Medicare before 2020, but your acceptance may not be guaranteed.
Can you switch Medigap plans without underwriting?
During your Medigap Open Enrollment Period, you can sign up for or change Medigap plans without going through medical underwriting. This means that insurance companies cannot deny you coverage or charge you more for a policy based on your health or pre-existing conditions.Nov 22, 2021
When did Medicare start?
But it wasn’t until after 1966 – after legislation was signed by President Lyndon B Johnson in 1965 – that Americans started receiving Medicare health coverage when Medicare’s hospital and medical insurance benefits first took effect. Harry Truman and his wife, Bess, were the first two Medicare beneficiaries.
When did Medicare start limiting out-of-pocket expenses?
In 1988 , Congress passed the Medicare Catastrophic Coverage Act, adding a true limit to the Medicare’s total out-of-pocket expenses for Part A and Part B, along with a limited prescription drug benefit.
How much was Medicare in 1965?
In 1965, the budget for Medicare was around $10 billion. In 1966, Medicare’s coverage took effect, as Americans age 65 and older were enrolled in Part A and millions of other seniors signed up for Part B. Nineteen million individuals signed up for Medicare during its first year. The ’70s.
How much will Medicare be spent in 2028?
Medicare spending projections fluctuate with time, but as of 2018, Medicare spending was expected to account for 18 percent of total federal spending by 2028, up from 15 percent in 2017. And the Medicare Part A trust fund was expected to be depleted by 2026.
What is the Patient Protection and Affordable Care Act?
The Patient Protection and Affordable Care Act of 2010 includes a long list of reform provisions intended to contain Medicare costs while increasing revenue, improving and streamlining its delivery systems, and even increasing services to the program.
How many people will have Medicare in 2021?
As of 2021, 63.1 million Americans had coverage through Medicare. Medicare spending is expected to account for 18% of total federal spending by 2028. Medicare per-capita spending grew at a slower pace between 2010 and 2017. Discussion about a national health insurance system for Americans goes all the way back to the days ...
What was Truman's plan for Medicare?
The plan Truman envisioned would provide health coverage to individuals, paying for such typical expenses as doctor visits, hospital visits, ...
When did Medicare start discriminating against genetic information?
Another turning point for Medicare came in 2008 with the introduction of the Genetic Information Nondiscrimination Act. This act made it illegal for a health insurance plan provider to discriminate against genetic information.
What act made sure any pre-existing conditions that had exclusion from the previous policy were also excluded from the new
Under the Consolida ted Appropriations Act of 2001, these users were able to purchase new supplemental coverage. This act made sure any pre-existing conditions that had exclusion from the previous policy were also excluded from the new plan.
What was the last act passed in the nineties?
The last act to be passed in the nineties was the Omnibus Consolidated and Emergency Supplemental Appropriation Act of 1999. The most important part of this act called on the providers that paid for these specific plans. With the passing of this act, they were now subject to civil penalties.
What is the Catastrophic Coverage Act?
One of these acts was the Medicare Catastrophic Coverage Act. This act implements several restrictions to further protect consumers, such as out-of-pocket maximums and premiums. During this time, several voluntary guidelines became mandatory standards by the federal government.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). and is sold by private companies.
How many people does a Medigap policy cover?
for your Medigap policy. You pay this monthly premium in addition to the monthly Part B premium that you pay to Medicare. A Medigap policy only covers one person. If you and your spouse both want Medigap coverage, you'll each have to buy separate policies.
What is a Medigap policy?
Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
What happens if you buy a Medigap policy?
If you have Original Medicare and you buy a Medigap policy, here's what happens: Medicare will pay its share of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
What is Medicare Advantage?
Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources.
Can you cancel a Medigap policy?
This means the insurance company can't cancel your Medigap policy as long as you pay the premium. Some Medigap policies sold in the past cover prescription drugs. But, Medigap policies sold after January 1, 2006 aren't allowed to include prescription drug coverage.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Note: Medigap plans sold to people who are newly eligible for Medicare aren’t allowed to cover the Part B deductible.
When was Medicare mandatory?
Medicare is mandatory for those hired or rehired as state or local government employees after March 31, 1986. Those under a Section 218 Agreement already receive coverage for Medicare.
How long do you have to enroll in Medicare?
If you’re happy with your coverage, you can keep using it as your primary insurance and use Medicare as secondary insurance. Your Initial Enrollment Period begins three months before your sixty-fifth birthday and ends three months after you turn 65. Thus, you have seven months to enroll.
How long does it take to get Medicare if you have a disability?
People who get Social Security Disability benefits are automatically eligible for Part A. Medicare disability eligibility begins after 24 months of disability. Depending on income levels, you may have monthly premiums to pay. The amount you pay depends on your monthly income.
How long do you have to enroll in Part B?
Thus, you have seven months to enroll. If you choose to enroll after your Initial Enrollment Period ends, you could face a penalty. Or worse, delaying Part B could result in having to wait for the General Enrollment Period, which adds to the cost of your late penalty.
Can you delay Medicare after turning 65?
Yet, this means you must get employer coverage from a larger company. Now, delaying Medicare can result in Part B penalties. Also, buying Marketplace insurance after turning 65 is costly. Once Medicare eligible, you’ll lose your subsidy. So, for many, Medicare makes the most financial sense.
Is it mandatory to have Part A insurance?
Part A inpatient coverage comes at no cost to most Americans. It’s not mandatory to have Part A but if you’ve worked 40 or more quarters (ten or more years), you’ll get it premium-free. Those who qualify for free Part A should enroll once eligible.
Is Part D coverage mandatory?
Part D is not mandatory. But, drug coverage is great to have, even when you don’t have a monthly prescription. When you get a prescription for an antibiotic or another temporary drug, it’s nice to know you have coverage. If you choose to enroll at a later date, you’ll have a penalty.
What is Medicare Part A?
Medicare is a public health insurance program designed for individuals age 65 and over and people with disabilities. The program covers hospitalization and other medical costs at free or reduced rates. The hospitalization portion, Medicare Part A, usually begins automatically at age 65. Other Medicare benefits require you to enroll.
What is the national base beneficiary premium for 2021?
In 2021, the national base beneficiary premium is $33.06 and changes every year. If you have to pay the penalty, the penalty amount will be rounded to the nearest $.10, and this amount will be added to your monthly Part D premium for the rest of the time you are enrolled.
What happens if you decline Medicare?
Declining. Late enrollment penalties. Takeaway. If you do not want to use Medicare, you can opt out, but you may lose other benefits. People who decline Medicare coverage initially may have to pay a penalty if they decide to enroll in Medicare later. Medicare is a public health insurance program designed for individuals age 65 and over ...
Is there a penalty for not signing up for Medicare Part B?
If you choose not to sign up for Medicare Part B when you first become eligible, you could face a penalty that will last much longer than the penalty for Part A.
Does Medicare Advantage have penalties?
Medicare Part C (Medicare Advantage) is optional and does not have penalties on its own, but penalties may be included for late enrollment in the parts of Medicare included within your Medicare Advantage plan.
Is Medicare mandatory at 65?
While Medicare isn’t necessarily mandatory, it is automatically offered in some situations, and may take some effort to opt out of.
Is Healthline Media a licensed insurance company?
Healthline Media does not transact the business of insurance in any manner and is not licensed as an insurance company or producer in any U.S . jurisdiction. Healthline Media does not recommend or endorse any third parties that may transact the business of insurance. Last medically reviewed on May 14, 2020.
What is Medicare Supplement Insurance?
Medicare Supplement insurance is meant to limit unpleasant surprises from healthcare costs. Your health at age 65 may be no indicator of what’s to come just a few years later. You could get sick and face medical bills that devastate years of planning and preparation. Combine this with the fixed income that so many seniors find themselves on, ...
How much does Medicare Supplement cover?
Choosing Medicare Supplement insurance can help. It can cover up to 100% of out-of-pocket costs, depending on the plan. One out of every three Original Medicare beneficiaries — over 13 million seniors — have chosen to do so. 1.
What is the deductible for hospitalization in 2020?
You are responsible for the balance (or coinsurance). In 2020, the Part A deductible for hospitalization is $1,408 per benefit period and the Part B annual deductible is $198. 3. Medicare Supplement insurance is designed to help cover these out-of-pocket deductibles and coinsurance.
How long is the open enrollment period for Medicare?
The Medigap Open Enrollment Period covers six months. It starts the month you are 65 or older and are enrolled in Medicare Part B. In this period, no insurer offering supplemental insurance in your state can deny you coverage or raise the premium because of medical conditions.
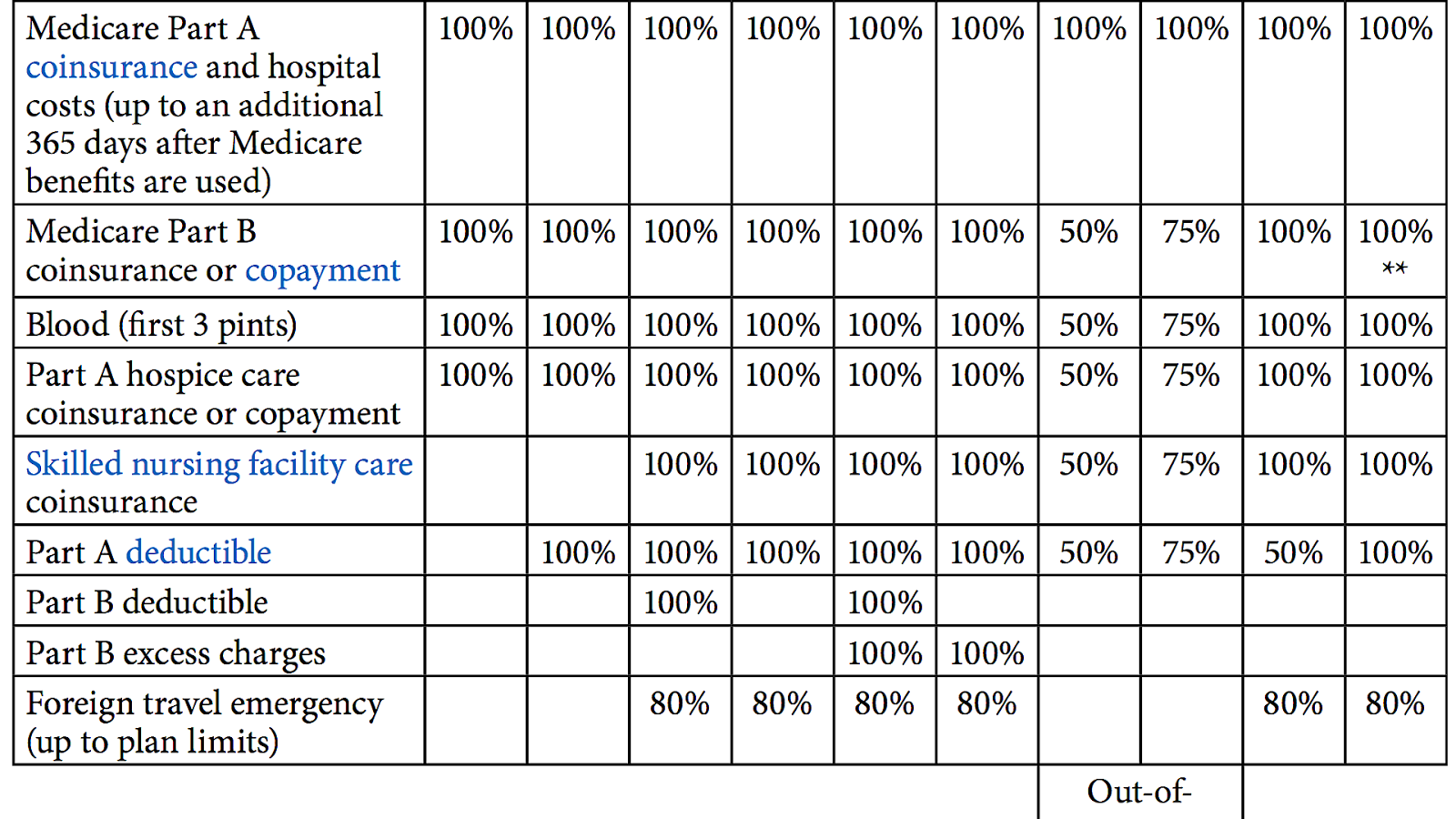
How many separate insurance plans are there?
Premiums for the same policy can vary between insurance companies. But, only the quoted price and the reputation of the insurer will vary. There are ten separate plans, labeled A through N. Two plans, C and F, are no longer offered to newly eligible beneficiaries.
Does Medicare Supplement cover all costs?
Original Medicare does not cover all costs. Medicare Supplement insurance, or Medigap, can cover what Medicare does not. Private insurance companies – vetted by the federal government – offer it to help manage out-of-pocket expenses. These policies do not add coverage.
Can you renew a Medigap policy?
You can renew your Medigap policy as long as you pay the premium. The insurer cannot use your health problems to cancel your policy or raise your premium.
What is Medicare Supplemental Insurance?
Various private health insurance plans sold to supplement Medicare in the United States. Medigap (also called Medicare supplement insurance or Medicare supplemental insurance) refers to various private health insurance plans sold to supplement Medicare in the United States. Medigap insurance provides coverage for many of the co-pays and some ...
When did Medigap take effect?
Medigap plans M and N took effect on June 1, 2010, bringing the number of offered plans down to ten from twelve. Congress passed the bill H.R. 2 on April 14, 2015, which will eliminate plans that cover the part B deductible for new Medicare beneficiaries starting Jan. 1st, 2020.
How much does Medigap cost in 2020?
Among the top-10 metro areas, the lowest cost for a male age 65 was $109-per-month available in Dallas. The highest cost was $509-per-month in Philadelphia.
Which states require Medigap insurance?
Some states such as Massachusetts, Minnesota, and Wisconsin require Medigap insurance to provide additional coverage than what is defined in the standardized Medigap plans. Some employers may provide Medigap coverage as a benefit to their retirees.
What is the most common age for Medigap?
The three ways are identified as Attained Age, Issue Age or Community Rated. The most common is Attained Age. Attained Age means that your Medigap Plan would increase at each new birthday based on the age you attain. Most of these plans do not start factoring this age increase until the 69th birthday.
Do all Medicare recipients have to have a Medigap policy?
Of these states, 25 require that Medigap policies be offered to all Medicare recipients.
Can I get Medicare if I have end stage renal disease?
Recipients of Social Security Disability Insurance (SSDI) benefits or patients with end-stage renal disease (ESRD) are entitled to Medicare coverage regardless of age, but are not automatically entitled to purchase Medigap policies unless they are at least 65.
