Medigap
Medigap refers to various private health insurance plans sold to supplement Medicare in the United States. Medigap insurance provides coverage for many of the co-pays and some of the co-insurance related to Medicare-covered hospital, skilled nursing facility, home health care, ambulance, durable medical equipment, and doctor charges. Medigap's name is derived from the notion that it exists to …
Full Answer
Do you have a right to buy a Medigap policy?
People new to Medicare on or after January 1, 2020, have the right to buy Plans D and G instead of Plans C and F. Section 3: Your Right to Buy a Medigap Policy 23 You have a guaranteed issue right if... Trial right ) You joined a Medicare
Can I Keep my Medigap policy if I join Medicare Advantage?
If you decide to keep your Medigap policy, you’ll have to pay your Medigap policy premium, but the Medigap policy can’t pay any deductibles, copayments, coinsurance, or premiums under a Medicare Advantage Plan. So, if you join a Medicare Advantage Plan, you may want to drop your Medigap policy.
Should I apply for Medigap insurance?
Once you decide on the insurance company and the Medigap policy you want, you should apply. The insurance company must give you a clearly worded summary of your Medigap policy. Make sure you read it carefully.
Can you buy a Medigap policy if you are under 65?
During this time, you can buy any Medigap policy sold in your state, even if you have health problems. If you’re under 65, you might not be able to buy a Medigap policy, or you may have to pay more. This is true even if you buy a Medigap policy in the first 6 months you have Medicare.
Does Medigap plan replace Medicare?
A Medigap policy is different from a Medicare Advantage Plan. Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
Is Medigap and Medicare Supplement the same thing?
Medigap, also known as Medicare Supplement Insurance, adds to original Medicare by filling in gaps where you aren't covered. Medigap plans usually don't cover vision, hearing, long-term care or at-home care.
Who pays for Medigap?
You pay the private insurance company a monthly premium for your Medigap plan in addition to the monthly Part B premium you pay to Medicare. A Medigap plan only covers one person. If you and your spouse both want Medigap coverage, you'll each have to buy separate policies.
How are Medigap plans funded?
Medigap is financed through beneficiary payments to private insurance firms, although retirees may have premiums paid on their behalf by their former employers. There are no government contributions toward Medigap premiums.
Can I switch from Medicare Advantage to Medigap?
Most Medicare Advantage Plans offer prescription drug coverage. , you may want to drop your Medigap policy. Your Medigap policy can't be used to pay your Medicare Advantage Plan copayments, deductibles, and premiums.
How Much Is Medigap per month?
In 2020, the average premium for Medicare supplemental insurance, or Medigap, was approximately $150 per month or $1,800 per year, according to Senior Market Sales, a full-service insurance organization.
Are Medigap premiums deducted from Social Security?
Paying for your coverage Medicare B premiums are deducted from your Social Security check, but Medigap premiums are paid directly to the private insurance carrier that provides the plan.
What is not covered by Medigap?
Medigap is extra health insurance that you buy from a private company to pay health care costs not covered by Original Medicare, such as co-payments, deductibles, and health care if you travel outside the U.S. Medigap policies don't cover long-term care, dental care, vision care, hearing aids, eyeglasses, and private- ...
Do Medigap plans have an out-of-pocket maximum?
Do Medigap Plans have an Out-of-Pocket Maximum? Medigap plans don't have a maximum out-of-pocket because they don't need one. The coverage is so good you'll never spend $5,000 a year on medical bills.
What is the difference between Medigap and Medicare Advantage?
Medigap is supplemental and helps to fill gaps by paying out-of-pocket costs associated with Original Medicare while Medicare Advantage plans stand in place of Original Medicare and generally provide additional coverage.
Who has the cheapest Medicare supplement insurance?
What's the least expensive Medicare Supplement plan? Plan K is the cheapest Medigap plan, with an average cost of $77 per month for 2022.
Who is the largest Medicare supplement provider?
AARP/United Health Group has the largest number of Medicare Supplement customers in the country, covering 43 million people in all 50 states and most U.S. territories. AARP licenses its name to insurer UnitedHealthCare, which helps make these policies so popular.
When to buy a Medigap policy
The best time to buy a Medigap Medicare Supplement Insurance (Medigap) An insurance policy you can buy to help lower your share of certain costs for Part A and Part B services (Original Medicare). policy is when you’re 65 (or older) and first get both Part A and Part B. You need both Part A and Part B to buy a Medigap policy.
How to buy a Medigap policy
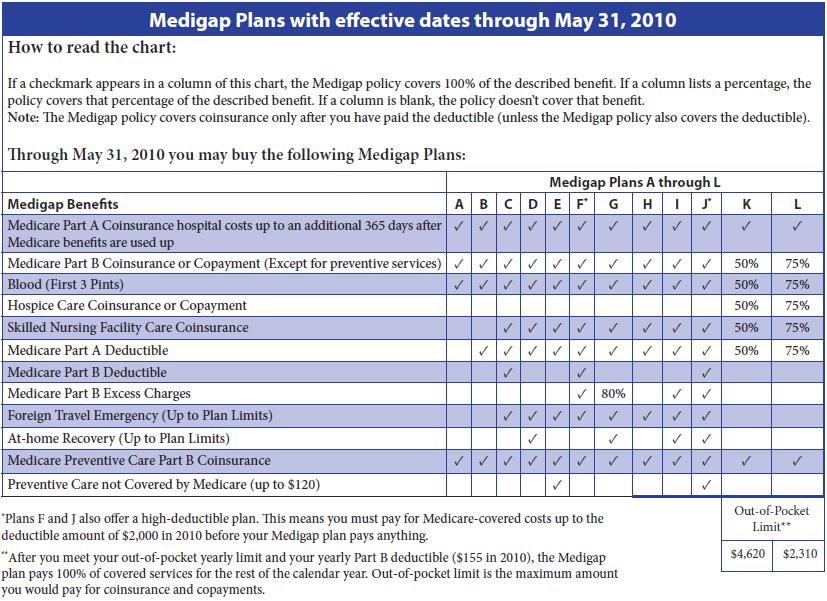
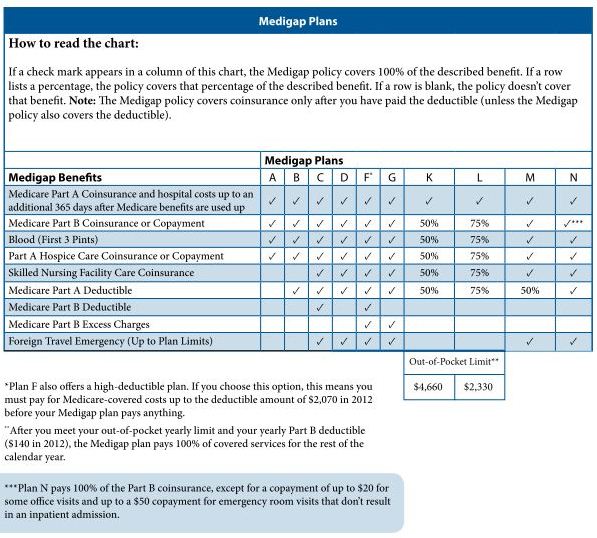
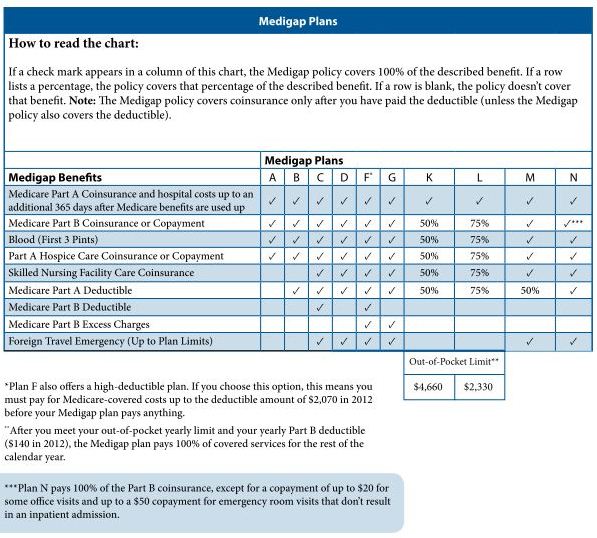
Medigap plans are standardized, and in most cases named by letters, like Plan G or Plan K.
When does Medigap coverage start?
Ask for your policy to become effective when you want coverage to start. Generally, Medigap policies begin the first of the month after you apply. If, for any reason, the insurance company won't give you the effective date for the month you want, call your State Insurance Department.
How long is the open enrollment period for Medigap?
Medigap Open Enrollment Period. A one-time only, 6-month period when federal law allows you to buy any Medigap policy you want that's sold in your state. It starts in the first month that you're covered under Part B and you're age 65 or older.
How to fill out a medical application?
Tips for filling out your application 1 Fill out the application carefully and completely, including medical questions. The answers you give will determine your eligibility for open enrollment or guaranteed issue rights (also called "Medigap protections"). 2 If your insurance agent fills out the application, check to make sure it's correct. 3 Remember that the insurance company can't ask you any questions about your family history or require you to take a genetic test. 4 If you buy a Medigap policy during your#N#Medigap Open Enrollment Period#N#A one-time only, 6-month period when federal law allows you to buy any Medigap policy you want that's sold in your state. It starts in the first month that you're covered under Part B and you're age 65 or older. During this period, you can't be denied a Medigap policy or charged more due to past or present health problems. Some states may have additional open enrollment rights under state law.#N#, the insurance company can’t use any medical answers you give to deny you a Medigap policy or change the price. 5 If you provide evidence that you're entitled to a guaranteed issue right, the insurance company can't use any medical answers you give to deny you a Medigap policy or change the price.
How to pay for insurance?
How to pay for your policy. It's best to pay by check, money order, or bank draft. Make it payable to the insurance company, not the agent. If buying from an agent, get a receipt with the insurance company's name, address, and phone number for your records. Some companies may offer electronic funds transfer.
Can you be denied a Medigap policy?
During this period, you can't be denied a Medigap policy or charged more due to past or present health problems. Some states may have additional open enrollment rights under state law. , the insurance company can’t use any medical answers you give to deny you a Medigap policy or change the price.
Step 1 – Decide which benefits you want, then decide which of the Medigap plans A–N meet your needs
Decide which benefits [glossary] you need and want while considering your current and future health care needs. You might not be able to switch policies later.
Step 4 – Buy the Medigap policy
Once you decide on the insurance company and the Medigap policy you want, you should apply. The insurance company must give you a clearly worded summary of your Medigap policy. Make sure you read it carefully. If you don't understand it, ask questions.
How to enroll in Medicare health insurance
The first step toward getting Medigap health insurance benefits is to enroll in Original Medicare. To qualify for Original Medicare, you must be at least 65 years old and a citizen or permanent legal resident of the United States. If you have a qualifying disability, you may be eligible for coverage before you turn 65.
Apply for Medicare Supplement insurance
After you enroll in Original Medicare, you can proceed to apply for a Medigap policy.
What is a Medigap policy?
Buying a Medigap policy is a smart way to get coverage for the out-of-pocket costs not covered by Original Medicare (Medicare Parts A & B). If you’re not sure whether you’re eligible to buy a Medicare Supplement insurance policy, read our eligibility page.
What happens if you don't buy Medigap?
If you don't buy during your enrollment period, you could have trouble finding a policy. If you are outside of your Medigap open enrollment period, there are some situations where you have guaranteed access to a policy.
Why do I leave my Medicare Advantage plan?
You leave a Medicare Advantage plan or Medigap policy because the company misled you or didn’t follow the rules. 1 https://www.medicare.gov/supplement-other-insurance/when-can-i-buy-medigap/when-can-i-buy-medigap.html.
How long do you have to switch health insurance?
You are able to switch plans within your 6-month open enrollment period. You do not have to wait for coverage to begin. Companies must sell you a policy during open enrollment. They cannot deny you coverage, and they cannot raise your prices because of past health problems.
Can I buy Medicare Supplement after open enrollment?
Buying after open enrollment. Technically, you can still buy Medicare Supplement insurance after your open enrollment period ends, but your health history can affect your options. At this point, it’s not guaranteed that you can buy a policy, and insurers can charge you higher rates because of your health history.
Can I buy Medigap insurance outside of open enrollment?
1 However, there are certain circumstances when you can buy outside of your open enrollment period with the same protections you'd have during the open enrollment period.
Can I buy a Medigap policy after enrollment?
These rights let you buy a Medigap policy after enrollment without penalty if: You have a Medicare Advantage plan & it’s leaving Medicare or ending coverage in your area. You have a Medicare Advantage plan & you are moving out of the plan’s service area. You have Original Medicare & you need to replace an employer health plan ...
What is Medicare Select?
Medicare Select. A type of Medigap policy that may require you to use hospitals and, in some cases, doctors within its network to be eligible for full benefits. policies that may require you to use certain providers. If you buy this type of Medigap policy, your premium may be less.
What does each insurance company decide?
Each insurance company decides how it will set the price, or. premium. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage. , for its Medigap policies. It’s important to ask how an insurance company prices its policies. The way they set the price affects how much you pay now ...
Why do premiums go up?
They may be the least expensive at first, but they can eventually become the most expensive. Premiums may also go up because of inflation and other factors.
What is medical underwriting?
medical underwriting. The process that an insurance company uses to decide, based on your medical history, whether to take your application for insurance, whether to add a waiting period for pre-existing conditions (if your state law allows it), and how much to charge you for that insurance.
Can you compare a Medigap policy?
As you shop for a Medigap policy, be sure to compare the same type of Medigap policy, and consider the type of pricing used .
What states have Medigap policies?
In Massachusetts, Minnesota, and Wisconsin, Medigap policies are standardized in a different way. Each insurance company decides which Medigap policies it wants to sell, although state laws might affect which ones they offer. Insurance companies that sell Medigap policies:
Where do you live in Medigap?
You live in Massachusetts, Minnesota, or Wisconsin. If you live in one of these 3 states, Medigap policies are standardized in a different way. You live in Massachusetts. You live in Minnesota. You live in Wisconsin.
What is coinsurance in Medicare?
Coinsurance is usually a percentage (for example, 20%). The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. (unless the Medigap policy also pays the deductible).
How much is Medicare deductible for 2020?
With this option, you must pay for Medicare-covered costs (coinsurance, copayments, and deductibles) up to the deductible amount of $2,340 in 2020 ($2,370 in 2021) before your policy pays anything. (Plans C and F aren't available to people who were newly eligible for Medicare on or after January 1, 2020.)
What is covered benefits?
benefits. The health care items or services covered under a health insurance plan. Covered benefits and excluded services are defined in the health insurance plan's coverage documents. but some offer additional benefits, so you can choose which one meets your needs.
Do insurance companies have to offer every Medigap plan?
Insurance companies that sell Medigap policies: Don't have to offer every Medigap plan. Must offer Medigap Plan A if they offer any Medigap policy. Must also offer Plan C or Plan F if they offer any plan.
Does Medicare cover Part B?
As of January 1, 2020, Medigap plans sold to new people with Medicare aren't allowed to cover the Part B deductible. Because of this, Plans C and F are not available to people new to Medicare starting on January 1, 2020.
What happens if you buy a Medigap policy before 2010?
If you bought your policy before 2010, it may offer coverage that isn't available in a newer policy. If you bought your policy before 1992, your policy: Might not be a Guaranteed renewable policy. May have a bigger Premium increase than newer, standardized Medigap policies currently being sold. expand.
How to switch Medigap insurance?
How to switch Medigap policies. Call the new insurance company and arrange to apply for your new Medigap policy. If your application is accepted, call your current insurance company, and ask for your coverage to end. The insurance company can tell you how to submit a request to end your coverage.
How long do you have to have a Medigap policy?
If you've had your Medicare SELECT policy for more than 6 months, you won't have to answer any medical questions.
How long is the free look period for Medigap?
Medigap free-look period. You have 30 days to decide if you want to keep the new Medigap policy. This is called your "free look period.". The 30- day free look period starts when you get your new Medigap policy. You'll need to pay both premiums for one month.
Can you exclude pre-existing conditions from a new insurance policy?
The new insurance company can't exclude your Pre-existing condition. If you've had your Medigap policy less than 6 months: The number of months you've had your current Medigap policy must be subtracted from the time you must wait before your new Medigap policy covers your pre-existing condition.
Does Medicare cover Part B?
As of January 1, 2020, Medigap plans sold to new people with Medicare aren't allowed to cover the Part B deductible. Because of this, Plans C and F are not available to people new to Medicare starting on January 1, 2020.
Can I keep my Medigap policy if I move out of state?
I'm moving out of state. You can keep your current Medigap policy no matter where you live as long as you still have Original Medicare. If you want to switch to a different Medigap policy, you'll have to check with your current or new insurance company to see if they'll offer you a different policy. If you decide to switch, you may have ...