In order to process a Redetermination request, we also need the following pieces of information:
- The beneficiary's name
- The Medicare Beneficiary Identifier (MBI)
- The DOS and the name of the service or item
- The name of the person filing the Redetermination request
- Send Redeterminations to the below address: J15 — Part B Correspondence CGS Administrators, LLC PO Box 20018 Nashville, TN 37202
- Medicare Redetermination Request Form
Full Answer
Where to mail Medicare appeal forms?
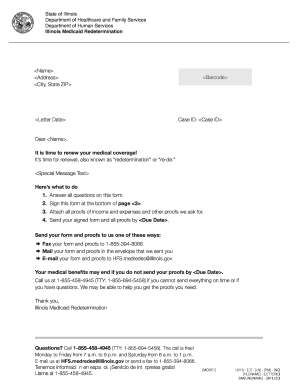
MEDICARE REDETERMINATION REQUEST FORM — 1st LEVEL OF APPEAL. Beneficiary’s name (First, Middle, Last) Medicare number . Item or service you wish to appeal . Date the service or item was received (mm/dd/yyyy) Date of the initial determination notice (mm/dd/yyyy) (please include a copy of the notice with this request)
Where do I send claims for Medicare?
There are 3 ways to file an appeal: Fill out a "Redetermination Request Form [PDF, 100 KB]" and send it to the Medicare contractor at the address listed on... Follow the instructions for sending an appeal. You must send your request for redetermination …
Where do I get the forms to file Medicare claims?
Dec 03, 2021 · To submit a Redetermination Request on paper (through the mail), follow these steps: Access the Medicare HHH Jurisdiction 15 Redetermination Request Form; Complete ALL fields of the Redetermination Form. Tip: complete the form electronically and print. Any redetermination request received that is not completed will be dismissed.
Where to send Medicare claims address?
Jul 03, 2019 · The name of the person filing the Redetermination request; Send Redeterminations to the below address: J15 — Part B Correspondence CGS Administrators, LLC PO Box 20018 Nashville, TN 37202. Medicare Redetermination Request Form; Updated: 07.03.19

What is a redetermination in Medicare?
A redetermination is a review of the claim by Medicare Administrative Contractor (MAC) personnel not involved in the initial claim determination.
How long does it take for a MAC to send a decision?
Generally, the MAC will send its decision (either in a letter, an RA, and/or an MSN) to all parties within 60 days of receipt of the request for redetermination. The decision will contain detailed information on further appeals rights, where applicable.
What is a redetermination request?
The specific item (s) and/or service (s) for which you're requesting a redetermination and the specific date (s) of service. An explanation of why you don't agree with the initial determination. If you've appointed a representative, include the name of your representative.
How to appeal a Medicare redetermination?
There are 3 ways to file an appeal: 1 Fill out a " Redetermination Request Form [PDF, 100 KB] " and send it to the Medicare contractor at the address listed on the MSN. 2 Follow the instructions for sending an appeal. You must send your request for redetermination to the company that handles claims for Medicare (their address is listed in the "Appeals Information" section of the MSN).#N#Circle the item (s) and/or services you disagree with on the MSN.#N#Explain in writing why you disagree with the decision or write it on a separate piece of paper, along with your Medicare number, and attach it to the MSN.#N#Include your name, phone number, and Medicare Number on the MSN.#N#Include any other information you have about your appeal with the MSN. Ask your doctor, other health care provider, or supplier for any information that may help your case. 3 Send a written request to the company that handles claims for Medicare (their address is listed in the "Appeals Information" section of the MSN.) Your request must include:#N#Your name and Medicare Number.#N#The specific item (s) and/or service (s) for which you're requesting a redetermination and the specific date (s) of service.#N#An explanation of why you don't agree with the initial determination.#N#If you've appointed a representative, include the name of your representative.
How long does it take to appeal a Medicare payment?
The MSN contains information about your appeal rights. You'll get a MSN in the mail every 3 months, and you must file your appeal within 120 days of the date you get the MSN.
How long does it take for Medicare to make a decision?
You can submit additional information or evidence after the filing redetermination request, but, it may take longer than 60 days for the Medicare Administrator Contractor (MAC) that processes claims for Medicare to make a decision. If you submit additional information or evidence after filing, the MAC will get an extra 14 calendar days ...
myCGS - Submit Electronically
Please note that providers have two options to submit Redetermination Requests: through the mail or through the secure web portal, myCGS. Submitting requests through myCGS saves time and money.
esMD - Submit Electronically
The esMD system allows CGS to electronically receive redetermination requests, the first level of appeal. Submit and complete the Medicare HHH Jurisdiction 15 Redetermination Request Form when using esMD.
Submit on Paper
To submit a Redetermination Request on paper (through the mail), follow these steps:
How long does it take to get a decision from Medicare?
Any other information that may help your case. You’ll generally get a decision from the Medicare Administrative Contractor within 60 days after they get your request. If Medicare will cover the item (s) or service (s), it will be listed on your next MSN. Learn more about appeals in Original Medicare.
How long does it take to appeal a Medicare denial?
You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination. If you miss the deadline, you must provide ...
What is an appeal in Medicare?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: • A request for a health care service, supply, item, or drug you think Medicare should cover. • A request for payment of a health care service, supply, item, ...
What to do if you decide to appeal a health insurance plan?
If you decide to appeal, ask your doctor, health care provider, or supplier for any information that may help your case. See your plan materials, or contact your plan for details about your appeal rights.
How many levels of appeals are there?
The appeals process has 5 levels. If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you'll get instructions in the decision letter on how to move to the next level of appeal.
General Mailing Address
We encourage providers to send postal mail to the appropriate PO Box, but if you absolutely necessarily have to send Medicare documents via Priority mail or through a commercial courier (UPS, FedEx) for which a PO Box cannot be used, please use the following street address:
Qualified Independent Contractor (QIC) Reconsideration
Please use the following to submit requests for reconsiderations (second level appeals) to the QIC for Part A or Part B.