WHERE TO MAIL YOUR APPLICATION. Send this completed application with original signatures and all required documentation to your designated MAC. The MAC that services your State is responsible for processing your enrollment application. To locate the mailing address for your designated MAC, go to . www.cms.gov/MedicareProviderSupEnroll. CMS-855I (12/18) 3
Full Answer
What documents are needed for Medicare enrollment?
- Initial enrollment period. This is a 7-month window around your 65th birthday when you can sign up for Medicare. ...
- Open enrollment period (October 15–December 7). ...
- General enrollment period (January 1–March 31). ...
- Special enrollment period. ...
- Medicare Advantage open enrollment (January 1–March 31). ...
What forms do you need to apply for Medicare?
- The name and address of your employer (s) for this year and last year;
- The amount of money earned last year and this year. ...
- A copy of your Social Security Statement or a record of your earnings. ...
- The beginning and ending dates of any active U.S. ...
How do I sign up for Medicare?
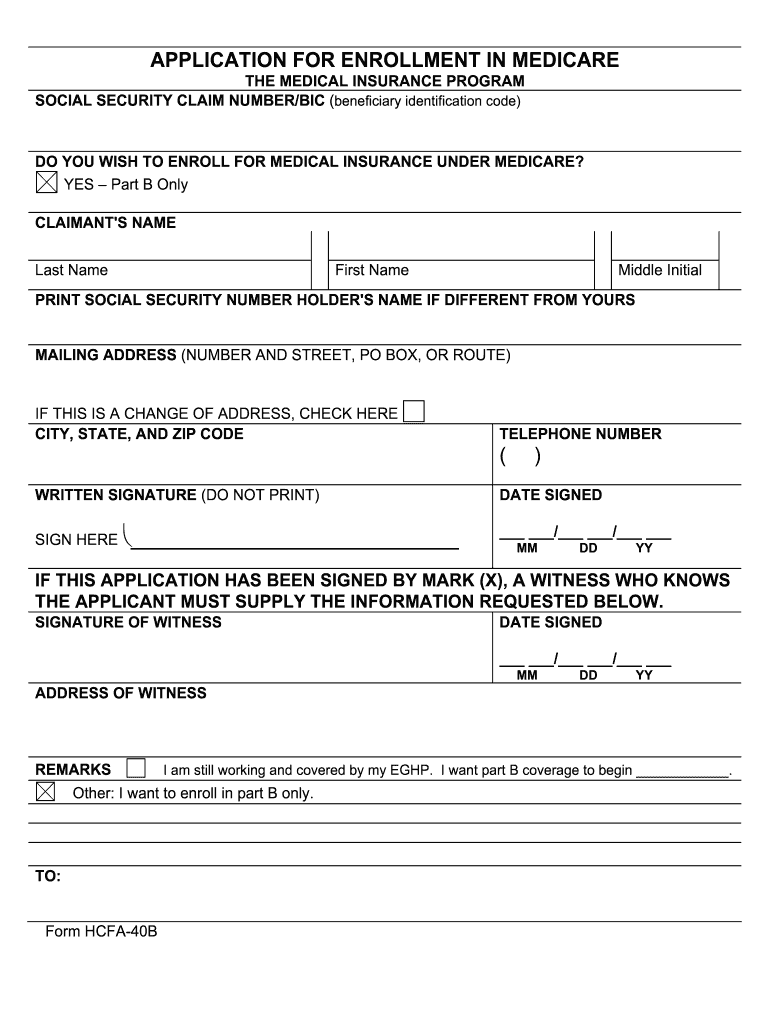
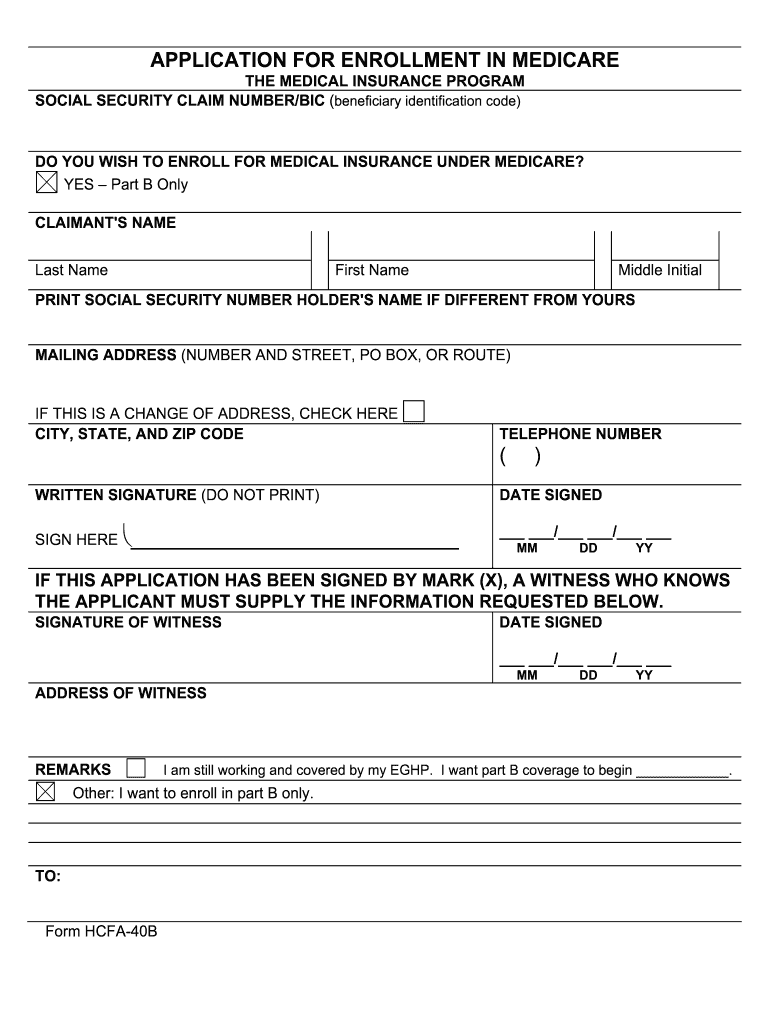
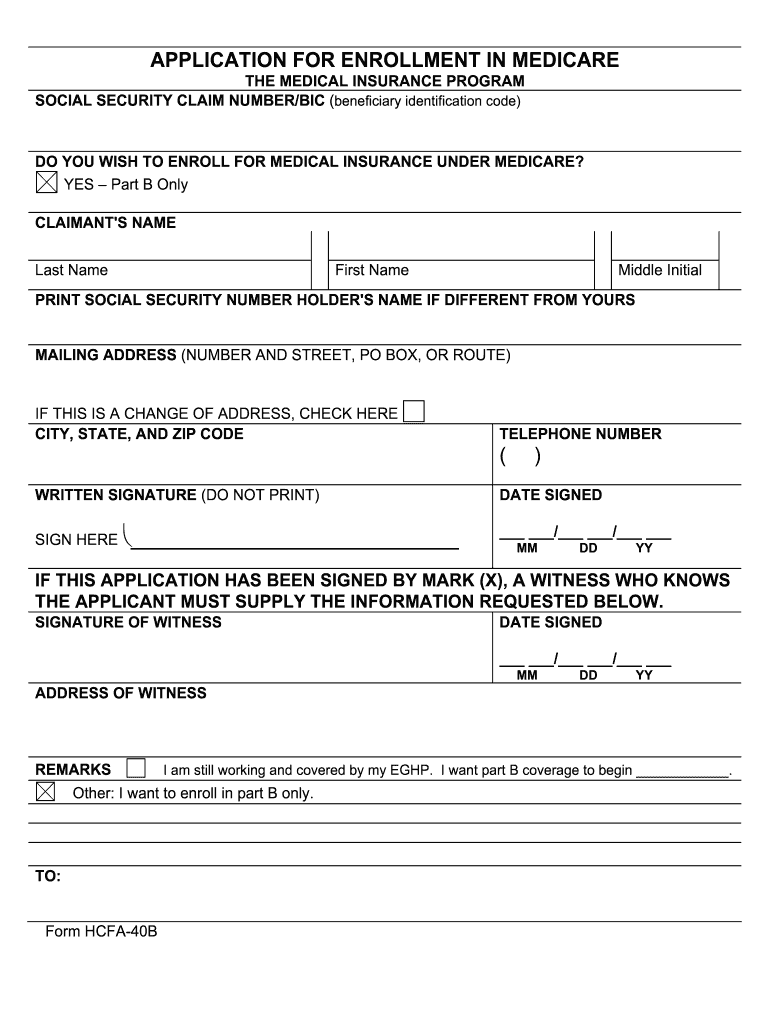
Note: When completing the forms CMS-40B and CMS-L564:
- State “I want Part B coverage to begin (MM/YY)” in the remarks section of the CMS-40B form or online application.
- If your employer is unable to complete Section B, please complete that portion as best as you can on behalf of your employer without your employer's signature.
- Also submit one of the following forms of secondary evidence:
How do you apply for Medicare?
You may qualify for prescription drug help automatically if you:
- Have full Medicaid coverage
- Get help from your state Medicaid program paying Medicare Part B premiums
- Receive Supplemental Security Income benefits
See more
How do I submit my Pecos 855R?
Providers and suppliers are able to submit their reassignment certifications either by signing section 6A and 6B of the paper CMS-855R application or, if completing the reassignment via Internet-based PECOS, by submitting signatures electronically or via downloaded paper certification statements (downloaded from www. ...
How do I add a new provider to Medicare?
Enrollment ApplicationsEnroll as a Medicare provider or supplier.Review information currently on file.Upload your supporting documents.Electronically sign and submit your information online.
What is a CMS 855?
CMS 855A. Form Title. Medicare Enrollment Application - Institutional Providers. Revision Date.
How do I add a provider to my Pecos?
0:146:13Medicare Provider Enrollment Through PECOS - YouTubeYouTubeStart of suggested clipEnd of suggested clipNumber if you do not already have an active NPI number you can register for one through the nationalMoreNumber if you do not already have an active NPI number you can register for one through the national plan and provider enumeration system or n Pez.
How do I fill out a CMS 460 form?
4:145:17Enrollment: CMS 460 Participation Agreement - YouTubeYouTubeStart of suggested clipEnd of suggested clipOrganizations at the bottom of the page have the authorized or delegated official signed date andMoreOrganizations at the bottom of the page have the authorized or delegated official signed date and list the office phone number this cannot be the contact person it must be an authorized or delegated.
What is Caqh and credentialing?
CAQH is an online data repository of credentialing data. Practitioners self report demographic, education and training, work history, malpractice history, and other relevant credentialing information for insurance companies to access.
What is 855B application?
CMS-855B (Rev. 03/2021) 1. WHO SHOULD SUBMIT THIS APPLICATION. Clinics, group practices, and other suppliers must complete this application to enroll in the Medicare program and receive a Medicare billing number.
What is a CMS 29 form?
The Form CMS-29 is utilized as an application to be completed by suppliers of RHC services requesting participation in the Medicare/Medicaid programs. This form initiates the process of obtaining a decision as to whether the conditions for certification are met as a supplier of RHC services.
What is a Pecos provider?
PECOS stands for Provider, Enrollment, Chain, and Ownership System. It is the online Medicare enrollment management system that allows individuals and entities to enroll as Medicare providers or suppliers.
Is NPI the same as Medicare provider number?
Yes, you must have an NPI to do business with any health insurance company including Medicare. But, your NPI is NOT your Medicare provider number. You may obtain an NPI through NPPES by applying online, click here to go to their website. It's a quick and simple process.
How do you navigate through Pecos for initial enrollment?
0:1012:09PECOS Enrollment Tutorial – Initial Enrollment for an Individual ProviderYouTubeStart of suggested clipEnd of suggested clipEntering user ID and password selected login button after logging in you'll need to select this myMoreEntering user ID and password selected login button after logging in you'll need to select this my enrollments button here first.
How do I update Pecos?
Once you have completed any changes in NPPES, you can update your PECOS account at https://pecos.cms.hhs.gov. TMF's short video, Updating Your Medicare Provider Enrollment, Chain, and Ownership System (PECOS) Account, provides some guidance for this process.
How to become a Medicare provider?
Become a Medicare Provider or Supplier 1 You’re a DMEPOS supplier. DMEPOS suppliers should follow the instructions on the Enroll as a DMEPOS Supplier page. 2 You’re an institutional provider. If you’re enrolling a hospital, critical care facility, skilled nursing facility, home health agency, hospice, or other similar institution, you should use the Medicare Enrollment Guide for Institutional Providers.
How to get an NPI?
If you already have an NPI, skip this step and proceed to Step 2. NPIs are issued through the National Plan & Provider Enumeration System (NPPES). You can apply for an NPI on the NPPES website.
How long does it take to change your Medicare billing?
To avoid having your Medicare billing privileges revoked, be sure to report the following changes within 30 days: a change in ownership. an adverse legal action. a change in practice location. You must report all other changes within 90 days. If you applied online, you can keep your information up to date in PECOS.
Do you need to be accredited to participate in CMS surveys?
ii If your institution has obtained accreditation from a CMS-approved accreditation organization, you will not need to participate in State Survey Agency surveys. You must inform the State Survey Agency that your institution is accredited. Accreditation is voluntary; CMS doesn’t require it for Medicare enrollment.
Can you bill Medicare for your services?
You’re a health care provider who wants to bill Medicare for your services and also have the ability to order and certify. You don’t want to bill Medicare for your services, but you do want enroll in Medicare solely to order and certify.
How to change Medicare enrollment after getting an NPI?
Before applying, be sure you have the necessary enrollment information. Complete the actions using PECOS or the paper enrollment form.
How to get an NPI for Medicare?
Step 1: Get a National Provider Identifier (NPI) You must get an NPI before enrolling in the Medicare Program. Apply for an NPI in 1 of 3 ways: Online Application: Get an I&A System user account. Then apply in the National Plan and Provider Enumeration System (NPPES) for an NPI.
How to request hardship exception for Medicare?
You may request a hardship exception when submitting your Medicare enrollment application via either PECOS or CMS paper form. You must submit a written request with supporting documentation with your enrollment that describes the hardship and justifies an exception instead of paying the application fee.
How long does it take to become a Medicare provider?
You’ve 90 days after your initial enrollment approval letter is sent to decide if you want to be a participating provider or supplier.
What is Medicare Part B?
Medicare Part B claims use the term “ordering/certifying provider” (previously “ordering/referring provider”) to identify the professional who orders or certifies an item or service reported in a claim. The following are technically correct terms:
What is Medicare revocation?
A Medicare-imposed revocation of Medicare billing privileges. A suspension, termination, or revocation of a license to provide health care by a state licensing authority or the Medicaid Program. A conviction of a federal or state felony within the 10 years preceding enrollment, revalidation, or re-enrollment.
How much is the Medicare application fee for 2021?
Application Fee Amount. The enrollment application fee sent January 1, 2021, through December 31, 2021, is $599. For more information, refer to the Medicare Application Fee webpage. How to Pay the Application Fee ⤵. Whether you apply for Medicare enrollment online or use the paper application, you must pay the application fee online: