To find a doctor that accepts Medicare payments, you may want to visit the Centers for Medicare and Medicaid Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…Medicaid
Full Answer
How do you find a Medicare provider?
- Providers can enter data via the Interactive Voice Response (IVR) telephone systems operated by the MACs.
- Providers can submit claim status inquiries via the Medicare Administrative Contractors’ provider Internet-based portals.
- Some providers can enter claim status queries via direct data entry screens.
Where can I find a doctor that accepts Medicare and Medicaid?
How to find a doctor who accepts Medicare There are a few simple ways to find a doctor who accepts your Medicare plan: Visit physician compare. The Centers for Medicare & Medicaid Services (CMS) has a tool that allows you to look up doctors near you and compare them side-by-side.
Who are the Medicare providers?
You can go to any Medicare-approved doctor, other health care provider, or hospital that accepts the plan's payment terms and agrees to treat you. Not all providers will. If you join a PFFS Plan that has a network, you can also see any of the network providers who have agreed to always treat plan members.
How to find Aetna Medicare providers?
- Your plan may pay less toward your care. ...
- The fees for health services may be higher. ...
- Any amount you pay might not contribute to your plan deductible, if you have one.
- You may need preauthorization for any services you receive in order for any coverage to apply.
How do I find Medicare doctors in my area?
Log InMedicare: To find a provider who accepts Original Medicare, call 1-800-MEDICARE (633-4227) or use Medicare's Physician Compare tool. ... American Medical Association (AMA): The AMA offers a search engine on its website where you can find doctors in your area by specialty.More items...
Which websites provide information about Medicare?
Medicare.gov is the official website for the U.S. government's Medicare program. Medicare.gov provides official benefit information regarding Medicare, including different coverage options, costs, preventative services, and tools for Medicare beneficiaries.
What is the Physician Compare website?
Physician Compare is a Centers for Medicare & Medicaid Services (CMS) website that allows the public to find and select physicians who are currently enrolled in the Medicare program as well as other information on Eligible Professionals (EPs) who participate in CMS quality programs.
What is the difference between a Medicare provider and supplier?
Supplier is defined in 42 CFR 400.202 and means a physician or other practitioner, or an entity other than a provider that furnishes health care services under Medicare.
Is MyMedicare Gov a legitimate site?
A: The Centers for Medicare & Medicaid Services is the government agency that is responsible for Medicare and Medicaid. The website MyMedicare.gov is a legitimate website where you can find information about your personal Medicare account. It is safe to go directly to that website and enter personal information.
What is the best Medicare Part D plan?
Best-rated Medicare Part D providersRankMedicare Part D providerMedicare star rating for Part D plans1Kaiser Permanente4.92UnitedHealthcare (AARP)3.93BlueCross BlueShield (Anthem)3.94Humana3.83 more rows•Mar 16, 2022
How do you check a doctors performance?
To determine a doctor's status, go to the Medical Board's website or call (800) 633-2322 and someone at the Medical Board will look up the doctor for you. To use the website, click on “License Search” on the home page.
How do you compare doctors?
These comparison tools can help you decide which doctor or facility is best for you.HealthGrades. http://www.healthgrades.com. ... Hospital Compare. https://www.medicare.gov/hospitalcompare/search.html. ... Leapfrog Group. http://www.leapfroggroup.org. ... National Committee for Quality Assurance (NCQA) ... Quality Check.
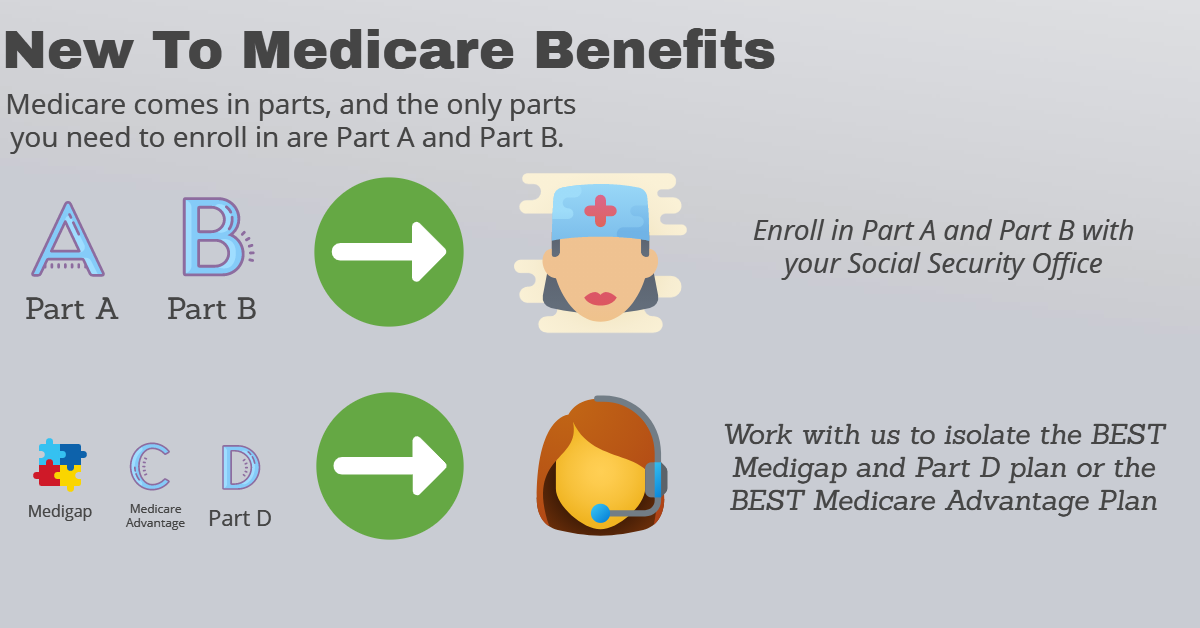
What is Part B of Medicare?
Part B helps pay for covered medical services and items when they are medically necessary. Part B also covers some preventive services like exams, lab tests, and screening shots to help prevent, find, or manage a medical problem. Cost: If you have Part B, you pay a Part B premium each month.
What is Pecos?
PECOS is the online Medicare enrollment management system which allows you to: Enroll as a Medicare provider or supplier. Revalidate (renew) your enrollment. Withdraw from the Medicare program. Review and update your information.
What does Medicare approved provider mean?
To be approved or certified by Medicare means that the provider has met the requirements to receive Medicare payments. Medicare certification is one way to protect you as the Medicare beneficiary and assure the quality of your care.
What does Medicare Provider mean?
A Medicare provider is a physician, health care facility or agency that accepts Medicare insurance. Providers earn certification after passing inspection by a state government agency. Make sure your doctor or health care provider is approved by Medicare before accepting services.
Who must tell you if you have been excluded from Medicare?
Your provider must tell you if he or she has been excluded from Medicare.
What does it mean when a provider opts out of Medicare?
What it means when a provider opts out of Medicare. Certain doctors and other health care providers who don't want to work with the Medicare program may "opt out" of Medicare. Medicare doesn't pay for any covered items or services you get from an opt out doctor or other provider, except in the case of an emergency or urgent need.
Can a provider accept Medicare?
The provider isn't required to accept only Medicare's fee-for-service charges. You can still get care from these providers, but they must enter into a private contract with you (unless you're in need of emergency or urgently needed care).
Do you have to pay for Medicare Supplement?
If you have a Medicare Supplement Insurance (Medigap) policy, it won't pay anything for the services you get.
Do you have to sign a private contract with Medicare?
Rules for private contracts. You don't have to sign a private contract. You can always go to another provider who gives services through Medicare. If you sign a private contract with your doctor or other provider, these rules apply: You'll have to pay the full amount of whatever this provider charges you for the services you get.
Can Medicare reimburse you for a bill?
Neither you or the provider will submit a bill to Medicare for the services you get from that provider and Medicare won't reimburse you or the provider. Instead, the provider bills you directly and you pay the provider out-of-pocket.
How to check agency information?
Regularly check your agency's information (name, address, phone number, ownership type) using the Provider Preview Reports in the Certification and Survey Provider Enhanced Reports (CASPER) application in the Internet Quality Improvement and Evaluation System (iQIES) system.
What to do if your provider preview report needs to be updated?
If information on your Provider Preview Reports needs to be updated, contact your Medicare Administrative Contractor for help.
How to become a Medicare provider?
Become a Medicare Provider or Supplier 1 You’re a DMEPOS supplier. DMEPOS suppliers should follow the instructions on the Enroll as a DMEPOS Supplier page. 2 You’re an institutional provider. If you’re enrolling a hospital, critical care facility, skilled nursing facility, home health agency, hospice, or other similar institution, you should use the Medicare Enrollment Guide for Institutional Providers.
How to get an NPI?
If you already have an NPI, skip this step and proceed to Step 2. NPIs are issued through the National Plan & Provider Enumeration System (NPPES). You can apply for an NPI on the NPPES website.
How long does it take to change your Medicare billing?
To avoid having your Medicare billing privileges revoked, be sure to report the following changes within 30 days: a change in ownership. an adverse legal action. a change in practice location. You must report all other changes within 90 days. If you applied online, you can keep your information up to date in PECOS.
Do you need to be accredited to participate in CMS surveys?
ii If your institution has obtained accreditation from a CMS-approved accreditation organization, you will not need to participate in State Survey Agency surveys. You must inform the State Survey Agency that your institution is accredited. Accreditation is voluntary; CMS doesn’t require it for Medicare enrollment.
Can you bill Medicare for your services?
You’re a health care provider who wants to bill Medicare for your services and also have the ability to order and certify. You don’t want to bill Medicare for your services, but you do want enroll in Medicare solely to order and certify.
What information do you need to release a private health insurance beneficiary?
Prior to releasing any Private Health Information about a beneficiary, you will need the beneficiary's last name and first initial, date of birth, Medicare Number, and gender. If you are unable to provide the correct information, the BCRC cannot release any beneficiary specific information.
When does Medicare use the term "secondary payer"?
Medicare generally uses the term Medicare Secondary Payer or "MSP" when the Medicare program is not responsible for paying a claim first. The BCRC uses a variety of methods and programs to identify situations in which Medicare beneficiaries have other health insurance that is primary to Medicare.
What is BCRC in Medicare?
The Benefits Coordination & Recovery Center (BCRC) consolidates the activities that support the collection, management, and reporting of other insurance coverage for Medicare beneficiaries. The purpose of the COB program is to identify the health benefits available to a Medicare beneficiary and to coordinate the payment process to prevent mistaken Medicare payment. The BCRC does not process claims or claim-specific inquiries. The Medicare Administrative Contractors, (MACs), intermediaries, and carriers are responsible for processing claims submitted for primary or secondary payment and resolving situations where a provider receives a mistaken payment of Medicare benefits.
Can a Medicare claim be terminated?
Medicare claims paying offices can terminate records on the CWF when the provider has received information that MSP no longer applies (e.g., cessation of employment, exhaustion of benefits). Termination requests should be directed to your Medicare claims payment office.