Fill out a " Redetermination Request Form [PDF, 100 KB] " and send it to the Medicare contractor at the address listed on the MSN. Follow the instructions for sending an appeal. You must send your request for redetermination to the company that handles claims for Medicare (their address is listed in the "Appeals Information" section of the MSN).
Full Answer
When can I file an appeal to a Medicare claim?
You must file this appeal within 180 days of getting the denial of your first appeal. Medicare Advantage. With Medicare Advantage plans, you're dealing not only with Medicare, but with the rules set by the private insurance company that runs your program.
How do I file an appeal to a Medicare claim?
To file a Medicare appeal or a “redetermination,” here's what you do:
- Look over the notice and circle the items in question and note the reason for the denia.
- Write down the specific service or benefit you are appealing and the reason you believe the benefit or service should be approved, either on the notice or on a separate ...
- Sign it and write down your telephone number and Medicare number. ...
How to file for Medicare Appeals?
You can file an appeal if you disagree with a coverage or payment decision made by one of these:
- Medicare
- Your Medicare health plan
- Your Medicare drug plan
How to properly compose Medicare appeal letter and its sample?
Sample Appeal Letter A. Please accept this letter as [patient's name] appeal to [insurance company name] decision to deny coverage for [state the name of the specific procedure denied]. It is my understanding based on your letter of denial dated [insert date] that this procedure has been denied because: [quote the specific reason for the denial ...

What address do you send Medicare claims to?
Medicare All state claim address and phone number list, if any modification please comment it....Medicare claim address, phone numbers, payor id – revised list.StateArizonaIVR #1-877-908-8431Claim mailing addressMedicare Part B P.O. Box 6704 Fargo, ND 58108-6704Appeal addressMedicare Part B PO Box 6704 Fargo, ND 58108-6704Online resourcewww.noridianmedicare.com22 more columns
What is the first level of appeal for Medicare?
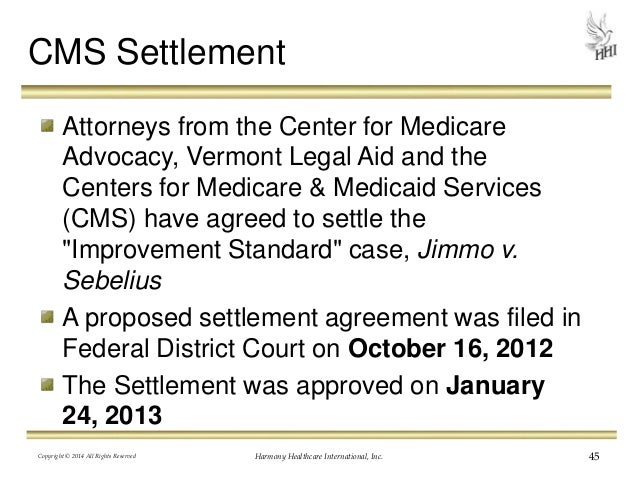
redeterminationThe first level of an appeal for Original Medicare is called a redetermination. A redetermination is performed by the same contractor that processed your Medicare claim. However, the individual that performs the appeal is not the same individual that processed your claim.
How do I file an appeal for Medicare?
Fill out a "Redetermination Request Form [PDF, 100 KB]" and send it to the company that handles claims for Medicare. Their address is listed in the "Appeals Information" section of the MSN. Or, send a written request to company that handles claims for Medicare to the address on the MSN.
What is a Level 1 appeal?
If you disagree, work with your provider to submit an appeal to your health plan – this is called a Level 1 appeal. Once an appeal is submitted, an appeals representative will review your request and any supporting documents to ensure a medical procedure meets medical necessity requirements.
What is the correct order of the levels of the Medicare appeal?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
Which of the following is the first step in the appeals process?
First, a transcript (written record) of the trial must be prepared by a court reporter.
How do I appeal a Medicare Part B premium?
First, you must request a reconsideration of the initial determination from the Social Security Administration. A request for reconsideration can be done orally by calling the SSA 1-800 number (800.772. 1213) as well as by writing to SSA.
What is the difference between reconsideration and redetermination?
Any party to the redetermination that is dissatisfied with the decision may request a reconsideration. A reconsideration is an independent review of the administrative record, including the initial determination and redetermination, by a Qualified Independent Contractor (QIC).
How long does Medicare have to respond to an appeal?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days. Payment request—60 days.
How do I appeal a CMS decision?
If you think the decision is wrong, you can ask the CMS to look at their decision again. This is called asking for a 'mandatory reconsideration'. You should say why you think the decision is wrong. You can call the CMS or write to them.
What are the four levels of appeals?
There are four stages to the appeal process — reconsideration, hearing, council, and court.
What are the five steps of the appeals process?
The 5 Steps of the Appeals ProcessStep 1: Hiring an Appellate Attorney (Before Your Appeal) ... Step 2: Filing the Notice of Appeal. ... Step 3: Preparing the Record on Appeal. ... Step 4: Researching and Writing Your Appeal. ... Step 5: Oral Argument.
What is an appeal in Medicare?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: • A request for a health care service, supply, item, or drug you think Medicare should cover. • A request for payment of a health care service, supply, item, ...
What to do if you decide to appeal a health insurance plan?
If you decide to appeal, ask your doctor, health care provider, or supplier for any information that may help your case. See your plan materials, or contact your plan for details about your appeal rights.
How long does Medicare take to respond to a request?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 calendar days. Payment request—60 calendar days. Learn more about appeals in a Medicare health plan.
How to ask for a prescription drug coverage determination?
To ask for a coverage determination or exception, you can do one of these: Send a completed "Model Coverage Determination Request" form. Write your plan a letter.
How long does it take to appeal a Medicare denial?
You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination. If you miss the deadline, you must provide ...
How long does it take for a Medicare plan to make a decision?
The plan must give you its decision within 72 hours if it determines, or your doctor tells your plan, that waiting for a standard decision may seriously jeopardize your life, health, or ability to regain maximum function. Learn more about appeals in a Medicare health plan.
How long does it take to get a decision from Medicare?
Any other information that may help your case. You’ll generally get a decision from the Medicare Administrative Contractor within 60 days after they get your request. If Medicare will cover the item (s) or service (s), it will be listed on your next MSN. Learn more about appeals in Original Medicare.
What level is an appeal sent to?
If the plan decides against you (fully or partially), your appeal is automatically sent to level 2.
How to appeal a Medicare reconsideration?
Include this information in your written reconsideration request: 1 Your name, address, and the Medicare number on your Medicare card [JPG]. 2 The items or services for which you're requesting a reconsideration, the dates of service, and the reason (s) why you're appealing. 3 If you've appointed a representative, include the name of your representative and proof of representation.
What to include in appeal for reconsideration?
If you've appointed a representative, include the name of your representative and proof of representation. Include any other information that may help your case.
How long does it take for a health insurance company to respond to a request?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days. Payment request—60 days. You'll get a fast request if your plan determines, or your doctor tells your plan, that waiting for a standard service decision may seriously jeopardize your: Life. Health.
How to contact Novitas for Medicare appeal?
If you have questions related to the first level of appeal / redetermination requests, please contact our Customer Service Center at 1-855-252-8782. Please use the following address and post office boxes to submit requests for claim redeterminations (first level appeals) to Novitas Solutions. Medicare Appeals.
What is the appeals process in Novitas?
The appeals process starts with Novitas Solutions at the first level of appeal / redetermination. If the appeals process continues to progress from one level to the next, questions regarding appeal status, other than a redetermination , should be directed to the party that is reviewing the documentation (depending on the level of appeal .)
What is the first level of Medicare appeal?
The first level of an appeal for Original Medicare is called a redetermination . A redetermination is performed by the same contractor that processed your Medicare claim. However, the individual that performs the appeal is not the same individual that processed your claim. The appeal is a new and independent review of your claim.
What is QIO in medical?
You may request an expedited determination by a Quality Improvement Organization (QIO) if you disagree with the provider's decision to discharge services or the decision to terminate services and your physician certifies that failure to continue the services places your health at significant risk.
What do you do after a claim is sent to the appropriate contractor?
After a claim is sent to the appropriate contractor, the contractor must: Determine if the items and services on the claim are covered or reimbursable by Medicare; Calculate any amount that is payable by Medicare; Make the payments to health care provider (s) who furnished the items or services; and.
How long does it take to appeal Medicare?
See the Medicare Summary Notice you received in the mail; your appeal rights are on the last page or back. You can request an appeal within 120 days from the date you received the Medicare Summary Notice.
Is OMHA responsible for levels 1 and 2?
OMHA is not responsible for levels 1, 2, 4, and 5 of the appeals process. OMHA provides additional information on other levels of appeals to help you understand the appeals process in a broad context. Content created by Office of Medicare Hearings and Appeals (OMHA) Content last reviewed on August 5, 2016.
Who does Medicare contract with?
Your doctor or hospital submits a bill to Medicare. Medicare contracts with private companies (" contractors ") to process medical claims (bills) for health care items and services provided to Medicare beneficiaries.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
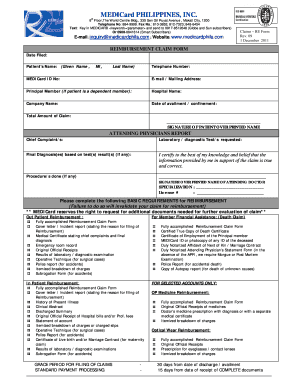
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.