What is the best Medicare plan?
They are here to talk about their 5 star medicare plans available to switch your current plan or during the election periods throughout the year. As independent agents, Deb and Jerry represent most of the supplement plan and drug -plan carriers and all Medicare advantage plan carriers.
What is Medicare 5 star rating system?
Medicare uses information from member satisfaction surveys, plans, and health care providers to give overall performance star ratings to plans. A plan can get a rating between 1 and 5 stars. A 5-star rating is considered excellent. These ratings help you compare plans based on quality and performance.
What is a five star Medicare plan?
5 ... Medicare to let them know that he wanted to keep his original Medicare. According to a Centers for Medicare & Medicaid Services spokesperson, an ACO is not "a Medicare Advantage Plan ...
Why are Medicare star ratings important?
- Staying healthy: access to preventative services to keep members healthy.
- Chronic conditions management: care coordination and frequency of treatment that members received for their long-term/chronic conditions.
- Member experience: overall satisfaction with the plan.

Who sets the standards for Medicare star ratings?
The Centers for Medicare & Medicaid Services (CMS) developed a five-star rating system for those on Medicare to compare Medicare Advantage and Medicare Part D prescription drug plan options. Medicare reviews the plans' performances each year and assigns each policy a star rating, between one and five.
How often are Medicare star ratings updated?
each fallA 5-star rating is considered excellent. These ratings help you compare plans based on quality and performance. Medicare updates these ratings each fall for the following year. These ratings can change each year.
How does CMS determine star rating?
- Ratings are calculated from a nursing home's performance on 10 Quality Measures (QMs), which are a subset of those reported on Nursing Home Compare. - The QMs include 7 long-stay (chronic care) QMs and 3 short-stay (post-acute care) QMs.
How can a Medicare beneficiary use the stars ratings?
The Centers for Medicare & Medicaid Services (CMS) created a Star Rating system to help beneficiaries and their families compare plan performance and quality for Medicare Advantage plans, Medicare Prescription Drug Plans, and Medicare Cost plans.
Do new plans have star ratings?
New contracts do not have the historical performance information necessary to determine a Star Rating, so they are temporarily assigned a 3.5% bonus payment for the first three years. After three or more years, contracts begin to receive a Star Rating based on their historical performance.
Do Part D plans have star ratings?
Medicare plans eligible for star ratings include Medicare Advantage, Medicare Cost, and Medicare Part D prescription drug plans.
What are Medicare Star measures?
Medicare uses a Star Rating System to measure how well Medicare Advantage and Part D plans perform. Medicare scores how well plans perform in several categories, including quality of care and customer service. Ratings range from one to five stars, with five being the highest and one being the lowest.
Why did CMS create star ratings?
CMS created the Five-Star Quality Rating System to help consumers, their families, and caregivers compare nursing homes more easily and to help identify areas about which you may want to ask questions.
What is the difference between hedis and stars?
For HEDIS measures, Star Ratings use a clustering algorithm that identifies “gaps” in the data and creates five categories (one for each Star Rating). Star Ratings incorporate a measure on improvement into plans' overall score, with a weight of 5. HPR does not incorporate an improvement bonus.
How can a Medicare beneficiary use the star ratings quizlet?
How can I Medicare beneficiary use the stars rating? Medicare beneficiaries enrolled in a low performing plan can switch to an available five-starplan at any time. RATIONAL: although plans not obtaining four stars or better may be penalized, plans that achieve highest quality ratings can achieve higher payments.
What states have 5 star Medicare Advantage plans?
States where 5-star Medicare Advantage plans are available:Alabama.Arizona.California.Colorado.Florida.Georgia.Hawaii.Idaho.More items...•
How to find Medicare star rating?
You can find a plan's star rating using Medicare's Plan Finder tool or by calling 1-800-MEDICARE.
What is the Medicare star rating system?
What Is the Medicare Star-Rating System? The Medicare Star-Rating System is a method for consumers to evaluate and compare Part D drug plans and Medicare Advantage Plans, which vary greatly in terms of cost and coverage. Medicare reviews the performance of plans one a year and publishes new star ratings each fall.
How many stars are there in Medicare Advantage?
The categories are ranked between one to five stars, with five being the highest and one being the lowest. According to Medicare Interactive, Medicare Advantage Plans are rated on their performance in the following five different categories: 1 .
When can Medicare change plans?
Enrollees can change plans during specific times or during Special Enrollment Periods (SEP), which are times outside normal enrollment periods that are triggered by specific circumstances.
Can you switch to a five star Medicare Advantage plan?
In general, you can change your plan or enroll in a new one only during a Special Enrollment Period. You can use an SEP to join or switch to a five-star Medicare Advantage or Part D plan. However, a SEP can only be used once a year.
Does Medicare Part D change?
Each January, Medicare Part D drug plans and Medicare Advantage Plans can change their coverage and costs for the new calendar year. Therefore, users of the plans should review their coverage and compare their plans with other available plans to ensure their coverage is optimal.
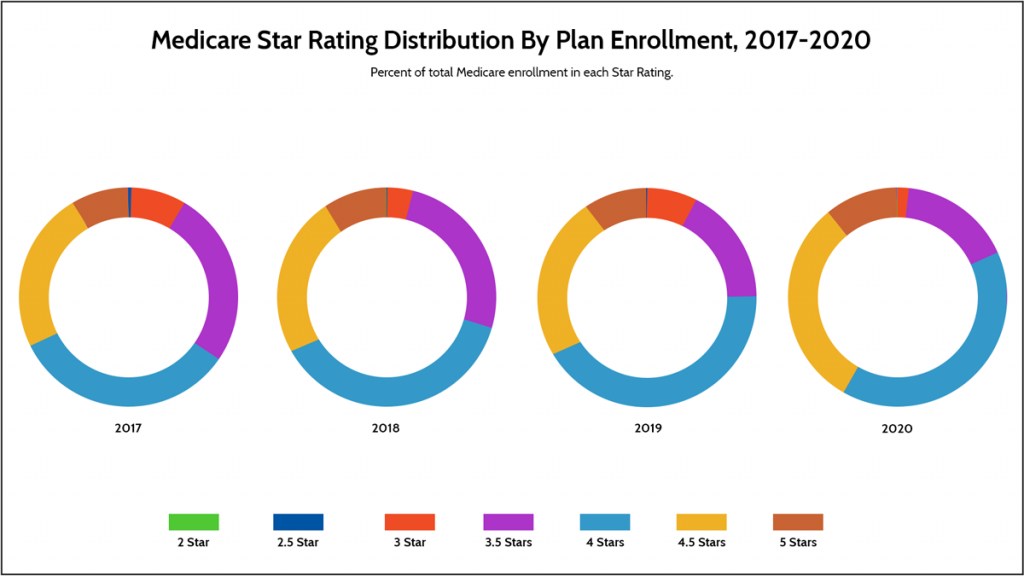
Star Ratings for Medicare Advantage Plans (MA-PD)
Good News: In October 2021, CMS issued their latest annual ratings. Just over two-thirds (68%) of Medicare Advantage plans that offer prescription drug coverage (MA-PD) have an overall rating of 4 stars or higher. This marks an increase from 49% in 2021 but still means 32% of plans received 3.5 stars or less.
Ratings for Medicare Drug Plans (Part D)
Bad News: According to the 2021 CMS report, the majority (58%) of individuals are in plans rated with between 1 and 3 stars. The balance, some 42% are in plans receiving 4 or more stars.
How does Medicare's star rating system work?
You could choose from a wide range of Medicare Part C (now known as Medicare Advantage) plans as early as 1997. But you didn't have a good way to compare them until 2008. That's when the Centers for Medicare & Medicaid Services (CMS) first rolled out the star rating system.
What parts of a health insurance plan are rated?
The way that the CMS rates healthcare plans depends on what type of plan it is.
What is the standard rating for a Medicare plan?
Most Medicare plans have a good rating these days, but not all. According to the CMS, nearly 68% of Medicare plans with prescription drug coverage (MA-PDP) in 2022 have a four-star rating or higher. That’s up from 49% in 2021.
How to use the rating system to pick the best health insurance plan
In general, it's best to choose the highest-rated plan that you can afford. You can compare plans and their ratings on the Medicare Plan Finder website. On the Plan Finder tool, each plan has an overall star rating based on all the rated categories.
The bottom line
Choosing between different Medicare plans can be tough. But the star ratings can help you identify high-performing ones and those with higher scores in categories that may matter to you. The CMS rates each plan on up to 40 different factors to create a helpful picture of how well the plan treats its members and their healthcare needs.
Top 5-star Medicare Advantage plans
Medicare Advantage plans with five stars are top-tier plans that are considered "excellent" by the Medicare's administering agency, the Centers for Medicare & Medicaid Services (CMS).
5-star special enrollment period
If a 5-star plan is available in your location, you qualify for a 5-star special enrollment period (SEP) that allows you to switch to a 5-star plan at any time during the year.
How Medicare star ratings are calculated
Each Medicare plan's overall star rating is a weighted average of several different data points. This means it's a robust measurement that can help you understand which are the best-performing Medicare plans in your area.
Frequently asked questions
Medicare star ratings are calculated using 40 criteria across Part C and Part D coverage. This includes survey data about member satisfaction, calculations about the number of complaints, outcomes such as how often those with diabetes fill their prescriptions and more.
Methodology
Data and analysis is based on Centers for Medicare & Medicaid Services (CMS) public use files, fact sheets and technical notes. Medicare Advantage analysis only includes plans that include prescription drug coverage and excludes employer-sponsored plans, special needs plans, PACE plans, sanctioned plans and health care prepayment plans (HCPPs).
How are Medicare plans rated?
The Centers for Medicare and Medicaid Services uses a star rating system to evaluate Medicare Advantage plans and Medicare Part D plans.
Which Medicare plans received 5-star ratings for 2022?
For 2022, there are a total of 87 Medicare contracts nationwide that have a 5-star rating (a significant increase from the 28 Medicare contracts that had 5-star ratings in 2021). Three are Medicare cost plans and 74 are Medicare Advantage plans with integrated Part D coverage.
How has the COVID pandemic affected Medicare star ratings?
Due to the pandemic, the federal government had to contend with the fact that a significant amount of the data used for star ratings could not be collected remotely, and that in-person data collection wasn’t feasible.