Medicare in Maryland covered the highest percentage of costs in the nation at 91.13%. At more than an entire percent lower, Alaska came in second at 89.01%. Two of the top ten states with the most retirees—Texas and Delaware—made it into the bottom ten for Medicare coverage.
Which states have the highest average Medicare Advantage premiums?
Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. Medicare Part D (prescription drug coverage)
How do Medicare ratings compare health plans?
· Medicare is the front-runner when it comes to networks. If you don’t want to stick to a limited number of doctors or hospitals, Original Medicare is likely your best option. With Original Medicare, you can go to any provider who accepts the national program.
How do MAPD plans rank with Medicare?
Your Medicare coverage choices. Learn about the 2 main ways to get your Medicare coverage — Original Medicare or a Medicare Advantage Plan (Part C). What Part A covers. Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care. What Part B covers
How do I find the best Medicare plan for me?
· Medicare Five-Star Ratings for Nursing Homes. Medicare does not pay for long-term care in a nursing home, but Part A pays for short-term stays in skilled nursing facilities and rehabilitation facilities after an inpatient hospitalization. 1 Regardless, Medicare assesses the quality of nursing homes for both short-term and long-term stays ...
What are CMS stars ratings?
Star Ratings are released annually and reflect the experiences of people enrolled in Medicare Advantage and Part D prescription drug plans. The Star Ratings system supports CMS's efforts to empower people to make health care decisions that are best for them.
Who benefits most from Medicare?
People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
What is the highest rated Medicare plan?
Blue Cross Blue Shield, Humana and United Healthcare earn the highest rankings among the national carriers in many states. Overall, Aetna Medicare ranks the best in the most (23) states. That said, there is no single “best plan.” Your needs and preferences will determine the best choice for you.
Why are Medicare star ratings important?
Medicare star ratings are important because they give you an idea about which plans in your area have the highest satisfaction ratings. Star ratings only pertain to Medicare Advantage and Part D plans. For both types of coverage, the ratings provide a way to compare your plan options beyond their cost.
What would happen if Medicare ended?
Payroll taxes would fall 10 percent, wages would go up 11 percent and output per capita would jump 14.5 percent. Capital per capita would soar nearly 38 percent as consumers accumulated more assets, an almost ninefold increase compared to eliminating Medicare alone.
What percent of seniors choose Medicare Advantage?
Recently, 42 percent of Medicare beneficiaries were enrolled in Advantage plans, up from 31 percent in 2016, according to data from the Kaiser Family Foundation.
Does Medicare cover dental?
Medicare doesn't cover most dental care (including procedures and supplies like cleanings, fillings, tooth extractions, dentures, dental plates, or other dental devices). Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
Can you switch back and forth between Medicare and Medicare Advantage?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
What are 4 types of Medicare Advantage plans?
Below are the most common types of Medicare Advantage Plans.Health Maintenance Organization (HMO) Plans.Preferred Provider Organization (PPO) Plans.Private Fee-for-Service (PFFS) Plans.Special Needs Plans (SNPs)
What states have 5-star Medicare Advantage plans?
States where 5-star Medicare Advantage plans are available:Alabama.Arizona.California.Colorado.Florida.Georgia.Hawaii.Idaho.More items...•
What Medicare has a 5-star rating?
The 21 health plans earning 5 stars include KelseyCare Advantage, Kaiser Permanente, UnitedHealthcare, CarePlus by Humana, Tufts Health Plan, Health Partners, Capital District Physicians' Health Plan, Quartz Medicare Advantage of Wisconsin, Cigna, Health Sun - Anthem, BCBS - Health Now New York and Martins Point.
What is the Medicare 5-star rating system?
Medicare uses information from member satisfaction surveys, plans, and health care providers to give overall performance star ratings to plans. A plan can get a rating between 1 and 5 stars. A 5-star rating is considered excellent. These ratings help you compare plans based on quality and performance.
Why is Washington ranked highly in Medicare?
Washington ranked fairly highly in our report, due in part to having a high number of available plans that are generally rated well for quality by Medicare.
How many people are in Medicare Advantage?
22 million Medicare beneficiaries (34% of all Medicare enrollees) are enrolled in a type of private Medicare plan called a Medicare Advantage plan. Another 20.6 million are enrolled in a stand-alone Medicare prescription drug plan (PDP).
How much does Medicare Part D cost?
Medicare Part D Prescription Drug Plan beneficiaries in the state pay an average monthly premium of $37.84 for their drug coverage. This dollar amount is right around the national average, and the average PDP deductible is roughly $44 higher than the national average at $366.80.
What is the MAPD premium for 2021?
The average MAPD premium in 2021 is $41.27 (around $8 higher than the national average), and the average MAPD drug coverage deductible is $169.15 for the year, which is very close to the national average. 69% of Vermont MAPD plans are rated 4 stars or higher by Medicare.
How many stars does Medicare have?
Quality is important to consumers, and in eight states, at least 75% of their MAPD plans score four stars or better for quality measures by the Centers for Medicare and Medicaid Services.
When does Medicare open enrollment end?
This period, also called the fall Medicare Open Enrollment period, lasts until December 7.
Does Medicare vary by state?
As noted in the maps above, the quality of Medicare’s local markets varies by state and region.
How much higher is Medicare compared to private insurance?
However, according to a 2020 KFF study, private insurance payment rates were 1.6-2.5 times higher than Medicare rates for inpatient hospital services. 5.
How much does Medicare cost?
While most people will pay $0 for Medicare Part A premiums, the standard premium for Medicare Part B is $148.50. 4 Parts A and B (Original Medicare) are the basic building blocks for coverage, and delaying your enrollment in either can lead to financial penalties.
What is the difference between Medicare and private insurance?
The difference between private health insurance and Medicare is that Medicare is mostly for individual Americans 65 and older and surpasses private health insurance in the number of coverage choices, while private health insurance allows coverage for dependents. Not only does Medicare provide many coverage combinations to choose from, ...
What is Medicare Supplement?
Medicare Supplement plans are designed to cover the out-of-pocket costs left over from Original Medicare. For example, these plans can cover coinsurance amounts, copays, or deductibles. Original Medicare + Medicare Supplement + Prescription Drug.
What happens if you delay Medicare for four years?
For example, if you delayed enrolling in Medicare for four years, you’ll have to pay a higher premium for eight years. Medicare Part B. The Part B penalty is a lifelong consequence to delaying your Medicare coverage. This late-enrollment penalty can increase your premiums by 10% for each year you delayed coverage. 10.
How much is Medicare Part A deductible?
The Medicare Part A deductible is $1,484. The Medicare Part B deductible is $203. 4. On average, an employer insurance plan will have an annual deductible of $1,400. 6. This is a national average and may not reflect what you actually pay in premiums. It is best to use your plan information to make comparisons.
Which is better: Medicare or Original?
Medicare is the front-runner when it comes to networks. If you don’t want to stick to a limited number of doctors or hospitals, Original Medicare is likely your best option. With Original Medicare , you can go to any provider who accepts the national program.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
How does Medicare measure quality of care?
Medicare also looks to see how often someone is sent back to the hospital and how many residents are vaccinated to prevent influenza and pneumonia. Another useful measure is the Medicare spending per beneficiary. This compares Medicare spending at that facility with skilled nursing facilities nationwide. Simply put, are you getting your money's worth?
How does Medicare look at nursing home staffing?
Medicare specifically looks at staffing ratios, specifically, the number of hours worked by registered nurses, licensed practical nurses, licensed vocational nurses, nurse aides, and physical therapists divided by the number of residents in the nursing home. 4 While this allows a quick glimpse at overall care ratios, it does not allow Medicare to see how many staff are working at any given time or how much care is given to each resident, i.e., some may require more care than others.
What is the Centers for Medicare and Medicaid Services?
Centers for Medicare and Medicaid Services. Ensuring safety and quality in America's nursing homes. Updated April 15, 2019.
How often does Medicare require health inspections?
Health inspections: Medicare requires health inspections to be performed at least once a year at each facility, more often if a facility is performing poorly. 3 This will include fire safety inspections and checks on emergency preparedness.
Why is more transparency needed in Medicare?
More transparency is needed so that Medicare beneficiaries can make informed decisions about where to receive care.
What is the five star rating system for hospitals?
Medicare has established a five-star rating system that lets you know which facilities are performing the best.
Does Medicare give a five star rating?
Unfortunately, you will only see an overall star rating when you search on Hospital Compare. Medicare does not make public what specific information was looked at for any given hospital. That means a hospital could have a five-star rating in three categories but perform poorly in as many as four other categories because that data was never reviewed.
How to check Medicare plan ratings?
You can compare up to three plans at a time. Or you can call 800-MEDICARE (1-800-633-4227) to get a plan’s ratings.
What does Medicare rating mean?
What the Ratings Mean. What Medicare Evaluates to Rate Quality. Medicare rates the quality of Medicare Advantage plans, which cover hospitalization, outpatient care, and often prescription-drug coverage. It also rates Part D drug plans, which help to pay for the cost of prescription medications for people not enrolled in a Medicare Advantage plan.
What does Medicare evaluate to rate quality?
What Medicare Evaluates to Rate Quality. Medicare uses information from many sources to do the ratings. This includes surveys filled out by members of a health plan as well as required data reporting from the health plan. Medicare also uses information from health care providers.
What is Medicare based on?
In general, Medicare rates plans based on member health, member complaints, receipt of recommended care, and member satisfaction. Some of the factors used to rate plans may be important to your health and satisfaction with the plan, others less so.
Is 5 stars good or bad for Medicare?
Five stars is excellent. Four stars is above average. Three stars is average. Two stars is below average. One star is poor. Continued. If a plan has no rating, it's new. Or there might not be enough information for a rating to be done. Find a Medicare Plan that Fits Your Needs Get a Free Medicare Plan Review.
How to compare Medicare plans?
People with Medicare can compare quality through the star ratings, along with other information such as cost and coverage, on the online Medicare Plan Finder tool available on Medicare.gov.
How many Medicare Advantage plans will be available in 2022?
In 2022, 295 plans (compared to 256 in 2021) will cover all Medicare services, plus Medicaid-covered behavioral health treatment or long-term services.
How much is Medicare Advantage 2022?
The agency said in late September that the average premium for Medicare Advantage plans will be lower in 2022 at $19 per month, compared to $21.22 in 2021. But Part D coverage is rising to $33 per month, compared to $31.47 in 2021.
How many health plans will have five stars in 2021?
In all, 73 health plans earned five stars, up significantly from the 21 five-star plans for 2021. Some of the major players earning five stars are UnitedHealthcare, Humana, Kaiser Permanente, BayCare Health Plans, Martin's Point Generations Advantage, Commonwealth Care Alliance and Tufts Health Plan, among others.
What does star rating mean?
Star ratings reflect a plan's performance and are related to quality bonus payments.
Can Medicare Advantage and Part D plan change in 2022?
During this time, Medicare beneficiaries can compare coverage options like Original Medicare and Medicare Advantage, and choose health and drug plans for 2022. Medicare Advantage and Part D plan costs and covered benefits can change from year to year, so Medicare beneficiaries should look at their coverage choices and decide on the options that best meet their health needs, said CMS.
What is Medicare Advantage?
Medicare Advantage is an all-in-one plan choice alternative for receiving Medicare benefits. You may also hear it referred to as Medicare Part C. This plan is bundled with Medicare Part A and Part B and usually includes Part D, which provides prescription drug coverage. Medicare pays private insurance companies to administer the benefits of Medicare Advantage plans they sell.
How many Medicare Advantage plans are there in 2021?
adults age 65 and older. But picking the right plan can be complicated—nationwide, insurance providers offered a total of 3,550 different Medicare Advantage plans in 2021 alone [1]. What’s more, finding the right insurance plan is highly personalized to the individual. Only by providing your ZIP code and demographic information can you see a list of plans for which you’re eligible, and even then, you’re likely comparing the details of approximately 30 plans.
What is the donut hole in Medicare?
Most Medicare drug plans have a coverage gap called the “donut hole,” which means there’s a temporary limit on what the drug plan will cover. “A person gets limited coverage while in the ‘donut hole.’ whether on a Medicare Advantage plan or a separate Part D plan,” says Antinea Martin-Alexander, founder of Advocate Insurance Group in South Carolina. “The individual will pay no more than 25% of the cost of the medication in the donut hole until a total out of $6,550 in out of pocket expenses is reached. There are different items that contribute to the out-of-pocket expenses while in the donut hole: any yearly drug deductible you may have, copays for any and all your medications, what the manufacturer’s discount is on that medication and what the insurance company pays for that medication,” she says.
How many doctors are in United Healthcare?
If network size is your top priority, consider any United Healthcare plans for which you may be eligible, as it has more than 1.3 million physicians and care professionals and 6,500 hospitals and care facilities in its nationwide network. Premiums, physician copays and specialist copays can also start as low as $0 depending on the plan, and additional benefits, including dental, vision, hearing, lifestyle and transportation coverage, may be available as well. United Healthcare is also one of the larger providers to offer lower insulin copays—$35 or less—which can be a significant benefit for people managing diabetes.
When does Medicare open enrollment end?
1. If you’re already enrolled in a Medicare Advantage plan, you can switch to a different Medicare Advantage plan or Original Medicare during the Medicare Advantage open enrollment period, which starts on Jan. 1 and ends on March 31 annually. You can only make one switch during that time period.
Is Humana a good health insurance?
With an A.M. Best rating of A- and a J.D. power ranking of 822 (out of 1,000), Humana is both financially stable and positively reviewed by people who have its health coverage. Humana offers health maintenance organization (HMO) plans, preferred provider organization (PPO) plans, private fee-for-service (PFFS) plans and special needs plans (SNPs) to cater to a variety of health care needs and budgets.
Does Medicare Advantage have a monthly premium?
Some Medicare Advantage plans may have lower out-of-pocket costs than Original Medicare, and some have a $0 monthly premium. Here are a few questions to consider before purchasing a plan.
How to find a health insurance navigator?
To find a health insurance navigator, go to HealthCare.gov and enter your ZIP code. These services are “free, confidential and available to the public around the country,” says Turner.
What is health insurance?
Health insurance is a contract that requires an insurer to pay some or all of a person’s medical expenses in exchange for a monthly premium. “It’s to prevent you from hitting financial ruin should you run into an emergency,” says Molly Moore, co-founder and chief health plan officer at health insurance start-up Decent. “Some people get health insurance because they know they have ongoing health care issues that need to be taken care of, and some people get health insurance because they’re scared of something that could happen that they can’t plan for,” she says.
What is the ACA?
The ACA offers financial assistance that reduces monthly premiums and out-of-pocket costs to help make health insurance more affordable. Premium tax credits, for example, are based on household income. “You probably qualify for assistance,” says Lang. With the American Rescue Plan Act of 2021, Americans who previously qualified for subsidies are eligible for more money and people who weren’t able to qualify previously now can, he adds.
Why do people with health insurance go to the doctor?
People who have health insurance are often more likely to go to the doctor when they need to because they know what it will cost , says Katie Roders Turner, executive director of the Family Healthcare Foundation in Tampa Bay, Florida. They tend to follow up on medical concerns their doctors flag, such as high blood pressure, before they turn into bigger problems, and they’re more likely to obtain necessary prescription drugs since they’re available at a more affordable rate.
Why is it important to read the fine print of a health insurance plan?
Outside these essential benefits, what a plan covers will vary, which is why it’s important to read the fine print.
When does open enrollment for health insurance start?
Open Enrollment for 2022 starts Monday, Nov. 1, 2021, and ends Saturday, Jan. 15, 2022. If you want your coverage to begin Jan. 1, 2022, you need to enroll in a plan by Dec.15, 2021.
Is health insurance expensive?
While health insurance is generally considered very expensive , there are ways to get help with paying for your coverage, says Lang. A recent Stride survey, found 80% of uninsured gig workers who didn’t think they could afford health insurance weren’t aware of tax credits that could assist with low-cost coverage. The American Rescue Plan Act of 2021 (also called the COVID-19 Stimulus Package) has made insurance much more affordable, he adds. Stride data shows nearly 40% of gig workers who enrolled in health insurance in 2021 were paying less than $1 a month.
Which states have the lowest Medicare premiums?
Florida, South Carolina, Nevada, Georgia and Arizona had the lowest weighted average monthly premiums, with all five states having weighted average plan premiums of $17 or less per month. The highest average monthly premiums were for Medicare Advantage plans in Massachusetts, North Dakota and South Dakota. *Medicare Advantage plans are not sold in ...
What is the second most popular Medicare plan?
Medigap Plan G is, in fact, the second-most popular Medigap plan. 17 percent of all Medigap beneficiaries are enrolled in Plan G. 2. The chart below shows the average monthly premium for Medicare Supplement Insurance Plan G for each state in 2018. 3.
How to contact Medicare Advantage 2021?
New to Medicare? Compare Medicare plan costs in your area. Compare Plans. Or call. 1-800-557-6059. 1-800-557-6059 TTY Users: 711 to speak with a licensed insurance agent.

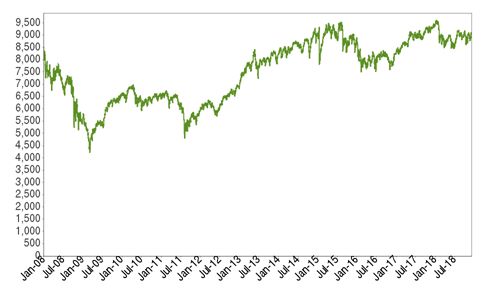
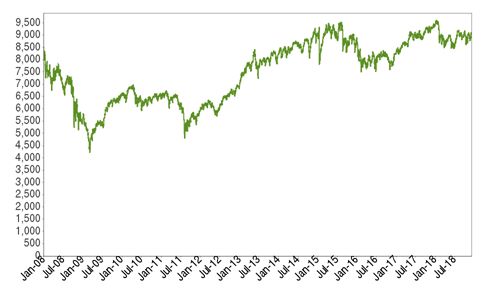
Best States For Medicare: Overview
2022 National Average Medicare Premiums, Deductibles and Quality
- MAPD plans and Prescription Drug Plans are both reasonably affordable in 2022. 1. The average 2022 MAPD premium is $62.66 per month, though many areas may offer plans that feature $0 monthly premiums. The average deductible for the drug coverage offered by MAPD plans is $292.98 for the year. 2. The average PDP premium is $47.59 per month in 2022, with an averag…
Best States For Medicare: 2022 Average Medicare Costs by State
- Factors in Medicare Advantage Premiums
The national average cost of a Medicare Advantage Prescription Drug plan in 2022 is $62.66 per month. But as you can see from the table above, the cost of an MA-PD plan can vary quite dramatically by location. 1. In Massachusetts, Michigan, Rhode Island and the Dakotas, average … - Medicare Advantage Plan Quality by State
Every year, the Centers for Medicare & Medicaid Services rates all Medicare Advantage plans according to a five-star scale based on various quality metrics. Three stars represents a plan of average quality, while four stars is considered above average and five stars is excellent. The met…
Expert Analysis
- As of October 15, millions of American seniors have the opportunity to purchase a private Medicare insurance plan for the first time or switch to a new coverage option during the Medicare Annual Enrollment Period (AEP). This period, also called the fall Medicare Open Enrollment period, lasts until December 7. We asked a panel of experts for their insight on what Medicare beneficia…
Methodology
- This project used data provided by the Centers for Medicare & Medicaid Services (CMS). The 2022 MA Landscape Source Files and 2022 PDP Landscape Source Fileswere used for analysis.
Fair Use Statement
- Of course we would love for you to share our work with others. We just ask that if you do, please grant us the proper citation with a link to this study so that we may be given credit for our efforts.
Research and Reports
- Our research reports analyze a number of issues important to seniors, from health perceptions, medical communication, health habits, and more. 1Every year, Medicare evaluates plans based on a 5-star rating system.