First, you must request a reconsideration of the initial determination from the Social Security Administration. A request for reconsideration can be done orally by calling the SSA 1-800 number (800.772.1213) as well as by writing to SSA . Below are the situations which may qualify a beneficiary for a new Part B determination:
What is a Medicare Part B premium appeal?
Medicare Part B Premium Appeals. The Social Security Administration (SSA) notifies a beneficiary of his or her Part B insurance premium and any IRMAA with the beneficiary’s annual notice of Social Security benefits (referred to as an initial determination). SSA is responsible for issuing all initial and reconsideration determinations.
How do I appeal a Medicare claim?
• Your representative’s signature and the date they signed the request. If you’re appointing someone to help with your appeal, send the representative a form or written request with your appeal request to the Medicare Administrative Contractor (MAC) (the company that handles claims for Medicare), or your Medicare health plan.
Can I appeal if my provider does not submit a claim?
You may be asked to pay for the items or services now, but because you request your provider or supplier to not submit a claim to Medicare, you can’t file an appeal. ■ Option 3—You don’t want the items or services that may not be paid for by Medicare, and you aren’t responsible for any payments.
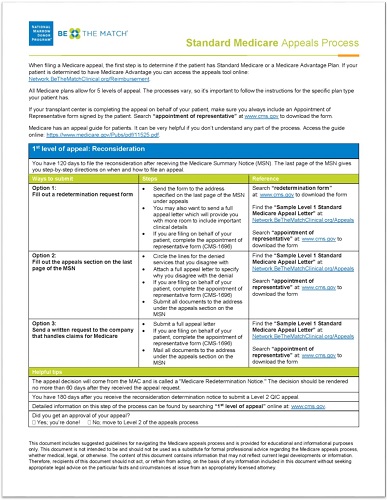
How many appeal levels are there for Medicare?
This booklet tells health care providers about Medicare’s 5 appeal levels in Fee-for-Service (FFS) (original Medicare) Parts A & B and includes resources on related topics. This booklet doesn’t cover Medicare Parts C or D appeals.

How do I appeal a Medicare Part B premium?
First, you must request a reconsideration of the initial determination from the Social Security Administration. A request for reconsideration can be done orally by calling the SSA 1-800 number (800.772. 1213) as well as by writing to SSA.
Does Medicare accept appeals?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: A request for a health care service, supply, item, or drug you think Medicare should cover.
What is the first step in the appeals process for Medicare Part B claim denials?
The first level of a standard claim appeal is called a Request for Redetermination and is a "paper review" of your claim. That means that you will not need to appear in person; the redetermination will be made on the basis of your medical records.
What are the five steps in the Medicare appeals process?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
How successful are Medicare appeals?
For the contracts we reviewed for 2014-16, beneficiaries and providers filed about 607,000 appeals for which denials were fully overturned and 42,000 appeals for which denials were partially overturned at the first level of appeal. This represents a 75 percent success rate (see exhibit 2).
How do you appeal?
What to Include in an Appeal Letter: Step-by-StepStep 1: Use a Professional Tone. ... Step 2: Explain the Situation or Event. ... Step 3: Demonstrate Why It's Wrong or Unjust. ... Step 4: Request a Specific Action. ... Step 5: Proofread the Letter Carefully. ... Step 6: Get a Second Opinion. ... Professional Appeal Letter.More items...
Can you get denied for Medicare Part B?
If a Part A or Part B claim is denied or not handled the way you think it should be, you can appeal the decision. You may request a formal Redetermination of the initial decision.
Can Medicare Part B be denied?
If you don't qualify to delay Part B, you'll need to enroll during your Initial Enrollment Period to avoid paying the penalty. You may refuse Part B without penalty if you have creditable coverage, but you have to do it before your coverage start date.
How long does Medicare have to respond to an appeal?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days. Payment request—60 days.
Which of the following are reasons a claim may be denied?
Here are the top 5 reasons why claims are denied, and how you can avoid these situations.Pre-certification or Authorization Was Required, but Not Obtained. ... Claim Form Errors: Patient Data or Diagnosis / Procedure Codes. ... Claim Was Filed After Insurer's Deadline. ... Insufficient Medical Necessity. ... Use of Out-of-Network Provider.
What is the difference between reconsideration and redetermination?
Any party to the redetermination that is dissatisfied with the decision may request a reconsideration. A reconsideration is an independent review of the administrative record, including the initial determination and redetermination, by a Qualified Independent Contractor (QIC).
What are the four levels of appeals?
There are four stages to the appeal process — reconsideration, hearing, council, and court.
Who has the right to appeal denied Medicare claims?
You have the right to appeal any decision regarding your Medicare services. If Medicare does not pay for an item or service, or you do not receive an item or service you think you should, you can appeal. Ask your doctor or provider for a letter of support or related medical records that might help strengthen your case.
How do you handle a denied Medicare claim?
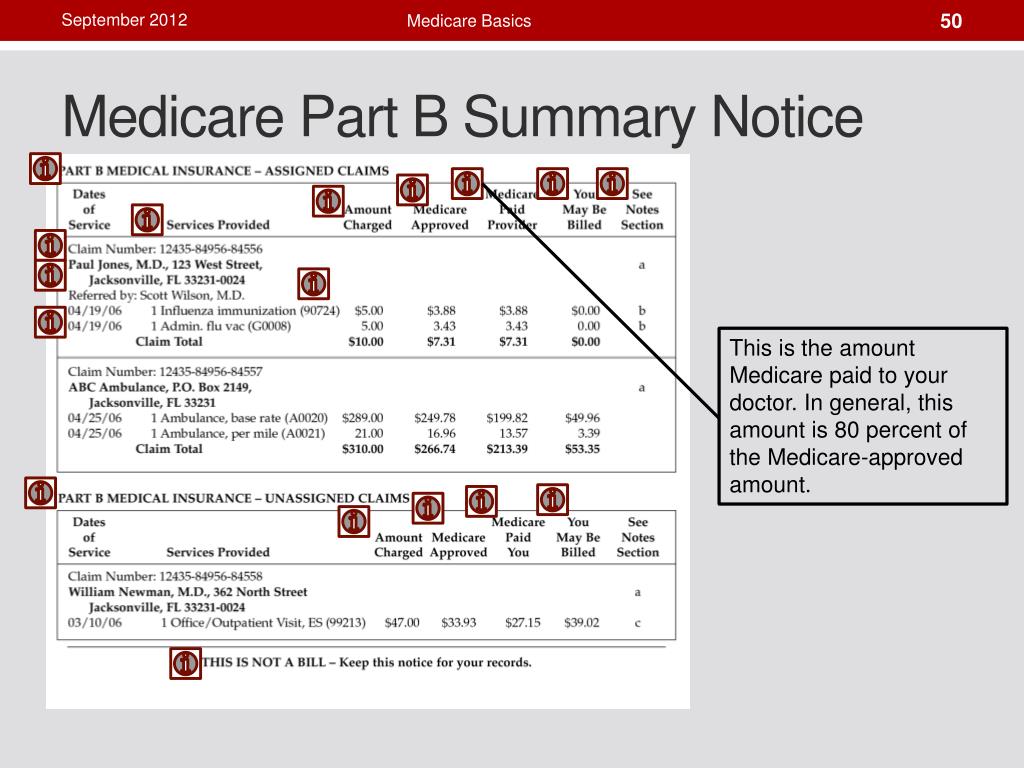
File your appeal within 120 days of receiving the Medicare Summary Notice (MSN) that lists the denied claim. Circle the item on your MSN that you are appealing and clearly explain why you think Medicare's decision is wrong. You can write on the MSN or attach a separate page.
Can you be denied Medicare coverage?
Generally, if you're eligible for Original Medicare (Part A and Part B), you can't be denied enrollment into a Medicare Advantage plan. If a Medicare Advantage plan gave you prior approval for a medical service, it can't deny you coverage later due to lack of medical necessity.
How do I write a Medicare appeal letter?
The Medicare appeal letter format should include the beneficiary's name, their Medicare health insurance number, the claim number and specific item or service that is associated with the appeal, dates of service, name and location of the facility where the service was performed and the patient's signature.
How to request reconsideration of Social Security?
A request for reconsideration can be done orally by calling the SSA 1-800 number (800.772.1213) as well as by writing to SSA .
What are the circumstances that qualify a beneficiary for a new Part B determination?
Below are the situations which may qualify a beneficiary for a new Part B determination: Events that result in the loss of dividend income or affect a beneficiary's expenses, but do not affect the beneficiary's modified adjusted gross income are not considered qualifying life-changing events.
Who is responsible for determining a beneficiary's Social Security benefits?
The Social Security Administration (SSA) notifies a beneficiary of his or her Part B insurance premium and any IRMAA with the beneficiary’s annual notice of Social Security benefits (referred to as an initial determination). SSA is responsible for issuing all initial and reconsideration determinations.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
How long does it take to appeal a level 2 redetermination?
You may file for a Level 2 appeal within 180 days of receiving the written notice of redetermination, which affirms the initial determination in whole or in part.
What is Medicare number?
The Medicare Number (Health Insurance Claim Number or Medicare Beneficiary Identifier); The specific service (s) and/or item (s) for which the reconsideration is requested; The specific date (s) of service; Your name; The name and signature of your representative, or your own name and signature if you have not authorized or appointed ...
What to do if you are not satisfied with the IRE decision?
If you’re not satisfied with the IRE’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or, in certain circumstances, a review of the appeal record by an ALJ or an attorney adjudicator.
What is the ABN for Medicare?
If you have Original Medicare and your doctor, other health care provider, or supplier thinks that Medicare probably (or certainly) won’t pay for items or services, he or she may give you a written notice called an ABN (Form CMS-R-131).
How long does it take for an IRE to review a case?
They must get this information within 10 days after the date you get the notice telling you your case file has been sent to the IRE. The IRE’s address is on the notice.
Does CMS exclude or deny benefits?
The Centers for Medicare & Medicaid Services (CMS) doesn’t exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, disability, sex, or age in admission to, participation in, or receipt of the services and benefits under any of its programs and activities, whether carried out by CMS directly or through a contractor or any other entity with which CMS arranges to carry out its programs and activities.
Do doctors have to give advance notice of non-coverage?
Doctors, other health care providers, and suppliers don’t have to (but still may) give you an “Advance Beneficiary Notice of Noncoverage” for services that Medicare generally doesn’t cover, like:
What happens if Medicare denies your appeal?
If they deny your appeal, they will provide instructions on how to appeal the denial to an Administrative Law Judge. Be aware that you will continue to pay the higher Medicare Part B premium while your appeal is in process. However, if your appeal is approved, it could be retroactive for any months you have already paid.
How much is Part B deductible in 2021?
In return for covering a small, once annual Part B deductible ($203 in 2021) you can sometimes find premiums as much as $250 lower than a Plan F. That keeps money in your pocket. Medigap plans L, M, N and High Deductible F are also great solutions for high income individuals.
What is MAGI on SSA-44?
Your MAGI amount is made up of your total adjusted gross income plus any tax-exempt interest income. (The Form SSA-44 has instructions which explain which line numbers from your IRS Tax return that you will use to calculate this number).
What is the difference between a complaint and an appeal?
What's the difference between a complaint and an appeal? A complaint is about the quality of care you got or are getting. For example, you can file a complaint if you have a problem calling the plan, or you're unhappy with how a staff person at the plan treated you. You file an appeal if you have an issue with a plan's refusal to cover a service, ...
Can you file a complaint with Medicare?
You can file a complaint if you have concerns about the quality of care or other services you get from a Medicare provider. How you file a complaint depends on what your complaint is about.