
If a beneficiary needs to submit a claim form, the beneficiary should complete and mail the Patient Request for Medical Payment form (CMS-1490S) to: First Coast Service Options Medicare Part B Claims P.O. Box 2009
Full Answer
What forms do you need to apply for Medicare?
- The name and address of your employer (s) for this year and last year;
- The amount of money earned last year and this year. ...
- A copy of your Social Security Statement or a record of your earnings. ...
- The beginning and ending dates of any active U.S. ...
What documents are needed for Medicare application?
What do you need to bring when applying for Medicare?
- Birth certificate. ...
- Proof of U.S. ...
- Your Social Security card (if already receiving SSA benefits) If you are already receiving benefits from Social Security or the Railroad Retirement Board, you may be required to supply your ...
- Health insurance information. ...
- Tax information. ...
- Military documents. ...
- Part B enrollment application. ...
Where to submit Medicare claims?
What is the first step in submitting Medicare claims?
- Complete a Patient’s Request For Medical Payment form. …
- Obtain an itemized bill for your medical treatment. …
- Add supporting documents to your claim. …
- 4. Mail completed form and supporting documents to Medicare.
How to file a Medicare claim?
How to file a Medicare claim. 1. Fill out a Patient’s Request for Medical Payment form. . You can also pick up a form at your local Social Security office. Instructions are included with the form. 2. Get an itemized bill for your medical treatment. Your itemized bill is the evidence for the Medicare claim.
How do I submit a DME claim to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
What form is used to send claims to Medicare?
CMS-1500 claim formThe CMS-1500 claim form is used to submit non-institutional claims for health care services provided by physicians, other providers and suppliers to Medicare.
Does Medicare accept paper claims?
The Administrative Simplification Compliance Act (ASCA) requires that as of October 16, 2003, all initial Medicare claims be submitted electronically, except in limited situations. Medicare is prohibited from payment of claims submitted on a paper claim form that do not meet the limited exception criteria. web page.
How do I get Medicare reimbursement?
How to Get Reimbursed From Medicare. To get reimbursement, you must send in a completed claim form and an itemized bill that supports your claim. It includes detailed instructions for submitting your request. You can fill it out on your computer and print it out.
Where do I mail Medicare claim forms?
Mail to Medicare, GPO Box 9822, in your capital city, or place in the 'drop box' at your local Medicare office. Do you want this recorded as your permanent postal address? medical expenses. Benefits will be paid to this person.
What is the mailing address for Medicare claims?
Medicare All state claim address and phone number list, if any modification please comment it....Medicare claim address, phone numbers, payor id – revised list.StateArizonaIVR #1-877-908-8431Claim mailing addressMedicare Part B P.O. Box 6704 Fargo, ND 58108-6704Appeal addressMedicare Part B PO Box 6704 Fargo, ND 58108-6704Online resourcewww.noridianmedicare.com22 more columns
Can you mail Medicare claims?
4. Mail completed form and supporting documents to Medicare All claims must be submitted by mail; you can't file a Medicare claim online. You can find the mailing address for your state's contractor in a number of ways: View the second page of the Medicare instructions for your Medicare claim type.
How do I submit a claim to CMS 1500?
CMS does not supply the form to providers for claim submission. In order to purchase claim forms, you should contact the U.S. Government Printing Office at 1-866-512-1800, local printing companies in your area, and/or office supply stores.
How are CMS 1500 forms submitted?
How to Submit Claims: Claims may be electronically submitted to a Medicare carrier, Durable Medical Equipment Medicare Administrative Contractor (DMEMAC), or A/B MAC from a provider's office using a computer with software that meets electronic filing requirements as established by the HIPAA claim standard and by ...
How do I get my $800 back from Medicare?
All you have to do is provide proof that you pay Medicare Part B premiums. Each eligible active or retired member on a contract with Medicare Part A and Part B, including covered spouses, can get their own $800 reimbursement.
How do I get my Medicare Part B refund?
Call 1-800-MEDICARE (1-800-633-4227) if you think you may be owed a refund on a Medicare premium. Some Medicare Advantage (Medicare Part C) plans reimburse members for the Medicare Part B premium as one of the benefits of the plan. These plans are sometimes called Medicare buy back plans.
What is a CMS demand letter?
The demand letter explains how to resolve the debt, either by repayment or presentation, and documentation of a valid defense. The insurer/TPA is to repay Medicare the lesser of its total primary payment obligation or the amount that Medicare paid.
What is the number to call for Medicare?
If a physician or supplier furnishes Medicare covered services to you and refuses to submit a claim on your behalf for those services, please call 1-800-MEDICARE (1-800-633-4227) in order to file a complaint with the Medicare contractor. TTY users should call 1-877-486-2048.
How to contact Medicare contractor?
If you still do not know the address of your Medicare contractor, call 1-800-MEDICARE (1-800-633-4227) . TTY users should call 1-877-486-2048.
How do I contact Medicare for diabetic test strips?
IF YOU NEED HELP, CALL 1-800 -MEDICARE (1-800-633-4227) . TTY USERS SHOULD CALL 1-877-486-2048.
What is the authority to collect Medicare information?
COLLECTION AND USE OF MEDICARE INFORMATION. We are authorized by the Centers for Medicare & Medicaid Services to ask you for information needed in the administration of the Medicare program. Authority to collect information is in section 205 (a), 1872 and 1875 of the Social Security Act, as amended.
How long does it take for Medicare to process a claim?
Make a copy of your claim submission for your records and allow at least 60 days for Medicare to receive and process your request.
How long does Medicare pay for a ship?
Medicare may pay for medically necessary services furnished on a ship in a U.S. port or within 6 hours of when the ship arrived at or departed from a U.S. port only if all of the following requirements are met:
What to call if you are not enrolled in Medicare?
The provider or supplier is not enrolled with Medicare. IF YOU NEED HELP, CALL 1-800-MEDICARE (1-800-633-4227). TTY USERS SHOULD CALL 1-877-486-2048. Type of Patient’s Request (see instructions for additional information, check one box only):
What does it mean when a provider refuses to file a claim for Medicare covered services?
The provider or supplier refused to file a claim for Medicare Covered Services The provider or supplier is unable to file a claim for the Medicare Covered Services The provider or supplier is not enrolled with Medicare
How long does Medicare pay for a ship?
Medicare may pay for medically necessary services furnished on a ship in a U.S. port or within 6 hours of when the ship arrived at or departed from a U.S. port only if all of the following requirements are met:
How long does it take for Medicare to process an itemized bill?
itemized bill and any supporting documents. Make a copy of your claim submission for your records and allow at least 60 days for Medicare to receive and process your request.
What is the authority to collect Medicare information?
We are authorized by the Centers for Medicare & Medicaid Services to ask you for information needed in the administration of the Medicare program. Authority to collect information is in section 205(a), 1872 and 1875 of the Social Security Act, as amended.
Does Medicare cover health care outside the US?
Medicare law prohibits payment for health care services furnished outside the United States (U.S.) except in certain limited circumstances. The term “outside the U.S.” means anywhere other than the 50 states of the U.S., the District of Columbia, Puerto Rico, the U.S. Virgin Islands, Guam, American Samoa, and the Northern Mariana Islands. Services furnished on a ship in a U.S. port or within 6 hours of when the ship arrived at or departed from a U.S. port are furnished inside the U.S.
Can DMEPOS be submitted to Medicare?
In most situations, your supplier of DMEPOS will submit your claim to Medicare , if they do not, you can submit a claim for an item or services furnished by this supplier.
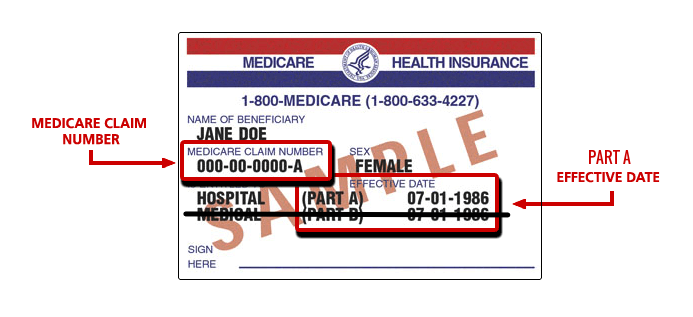
What do I need to file a 1490s?
You’ll need the 1490S form if your doctor does not file a claim for you and you need to file it yourself. What you’ll need: • Name, Medicare number, and address. • Description of the service or medical item. • Itemized bill containing the following information: ◦ Date of service. ◦ Place of service.
How long do you have to file a claim with Medicare?
Other important information: • You must file a claim within one calendar year from the date of service. Mail completed form and itemized bill to your state’s Medicare Administrative Contractor (MAC). You can find the address for your MAC by calling Medicare at 1-800-MEDICARE (1-800-633-4277). Download 1490S Form.
How to file a claim for Medicare?
How to File a Medicare Claim Yourself. If you need to file your own Medicare claim, you’ll need to fill out a Patient Request for Medical Payment Form, the 1490S. Make sure it’s filed no later than 1 full calendar year after the date of service. Medicare can’t pay its share if the submission doesn’t happen within 12 months.
How long does it take to get a Medicare summary notice?
Most claims are sent in within 24 hours of processing. You can even get your Medicare Summary Notice online; sign up to receive an e-Medicare Summary Notice and get monthly emails that link you to your details. With this, you get the most up to date information and no waiting 3 months for a letter.
How long does it take for Medicare to process a claim?
How Are Medicare Claims Processed? Your doctor will submit the claims. Then, Medicare will take about 30 days to process the claim. When it comes to Part A services, Medicare will pay the hospital directly. But, with Part B claims payment depends on whether or not the doctor accepts Medicare assignment.
Can a doctor submit a claim to Medicare?
But, in some instances, like foreign travel or doctors that don’t accept assignment, you’ll file the claim. If you receive an Advance Beneficiary Notice of Noncoverage and decide to proceed, it’s best to request your doctor submit the claim to Medicare before billing you.
Is Medicare always primary?
Medicare isn’t always primary. In this instance where Medicare is secondary, you’ll bill the primary insurance company before Medicare. Then, you can submit an Explanation of Benefits from the primary payor with the claim. The primary payer must process the claim first, and if they don’t, your doctor may bill Medicare.
Can Medicare help you complete a claim?
Medicare is trying to make it simple for beneficiaries; there are many tools that can help you complete any Medicare form or document on your own. Although, if you find that you need help with your claim, don’t hesitate to contact someone.
Can Medicare pay your share?
Medicare can’t pay its share if the submission doesn’t happen within 12 months. You can log in to MyMedicare.gov and view your claims to ensure they are being filed in a timely fashion. If your claims aren’t being taken care of, contact the doctor and ask them to file the claim.
What does it mean when a provider refuses to file a claim for Medicare covered services?
The provider or supplier refused to file a claim for Medicare Covered Services The provider or supplier is unable to file a claim for the Medicare Covered Services The provider or supplier is not enrolled with Medicare
How long does Medicare pay for a ship?
Medicare may pay for medically necessary services furnished on a ship in a U.S. port or within 6 hours of when the ship arrived at or departed from a U.S. port only if all of the following requirements are met:
What is the authority to collect Medicare information?
We are authorized by the Centers for Medicare & Medicaid Services to ask you for information needed in the administration of the Medicare program. Authority to collect information is in section 205(a), 1872 and 1875 of the Social Security Act, as amended.
How long does it take for Medicare to process an itemized bill?
itemized bill and any supporting documents. Make a copy of your claim submission for your records and allow at least 60 days for Medicare to receive and process your request.
Can DMEPOS be submitted to Medicare?
In most situations, your supplier of DMEPOS will submit your claim to Medicare , if they do not, you can submit a claim for an item or services furnished by this supplier.
Does Medicare cover health care outside the US?
Medicare law prohibits payment for health care services furnished outside the United States (U.S.) except in certain limited circumstances. The term “outside the U.S.” means anywhere other than the 50 states of the U.S., the District of Columbia, Puerto Rico, the U.S. Virgin Islands, Guam, American Samoa, and the Northern Mariana Islands. Services furnished on a ship in a U.S. port or within 6 hours of when the ship arrived at or departed from a U.S. port are furnished inside the U.S.
