You can file an Original Medicare claim by sending a Beneficiary Request for Medical Payment form and the provider’s bill or invoice to your regional Medicare Administrative Contractor (Here is a list of these broken down by state). Keep copies of everything you submit.
Full Answer
How do I file a Medicare claim?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
Can I submit my own Medicare claims?
Beneficiaries can submit their own claims for certain services when a provider won’t file a claim. However, you cannot file a claim with Original Medicare for diabetic test strips, Part B drugs, or equipment paid for under the DMEPOS Competitive Bidding Program. Your pharmacy or medical supplier must bill Medicare directly for these items.
What is a Medicare a claim?
A claim asks Medicare or your insurer to pay for your medical care. Claims are submitted to Medicare after you see a doctor or are treated in a hospital. If you have a Medicare Advantage or Part D plan, your insurer will process claims on Medicare’s behalf. Who files Medicare claims? Your healthcare provider will usually file claims for you.
How do I file a complaint against a Medicare provider?
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
What address do you send Medicare claims to?
Medicare All state claim address and phone number list, if any modification please comment it....Medicare claim address, phone numbers, payor id – revised list.StateArizonaIVR #1-877-908-8431Claim mailing addressMedicare Part B P.O. Box 6704 Fargo, ND 58108-6704Appeal addressMedicare Part B PO Box 6704 Fargo, ND 58108-6704Online resourcewww.noridianmedicare.com22 more columns
How do I submit a claim to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
Where do I send my Medicare form CMS 1490s?
MEDICARE ADMINISTRATIVE CONTRACTOR ADDRESS TABLEIf you received a service in:Mail your claim form, itemized bill, and supporting documents to::California Southern (For Part B)Noridian Healthcare Solutions, LLC P.O. Box 6775 Fargo, ND 58108-677554 more rows
What is the first step in submitting Medicare claims?
The first thing you'll need to do when filing your claim is to fill out the Patient's Request for Medical Payment form. ... The next step in filing your own claim is to get an itemized bill for your medical treatment.More items...•
How do I submit a claim to CMS 1500?
CMS does not supply the form to providers for claim submission. In order to purchase claim forms, you should contact the U.S. Government Printing Office at 1-866-512-1800, local printing companies in your area, and/or office supply stores.
What is the difference between UB 04 and CMS 1500?
The UB-04 (CMS-1450) form is the claim form for institutional facilities such as hospitals or outpatient facilities. This would include things like surgery, radiology, laboratory, or other facility services. The HCFA-1500 form (CMS-1500) is used to submit charges covered under Medicare Part B.
Does Medicare accept paper claims?
The Administrative Simplification Compliance Act (ASCA) requires that Medicare claims be sent electronically unless certain exceptions are met. Providers meeting an ASCA exception may send their claims to Medicare on a paper claim form. (For more information regarding ASCA exceptions, refer to Chapter 24.)
What is a CMS 1450 form?
The CMS-1450 form (aka UB-04 at present) can be used by an institutional provider to bill a Medicare fiscal intermediary (FI) when a provider qualifies for a waiver from the Administrative Simplification Compliance Act (ASCA) requirement for electronic submission of claims.
Can you submit Medicare forms online?
You can submit your claim online through your Medicare online account, Express Plus Medicare mobile app, at a service centre or by post. To submit your claim online, follow these steps: Complete a Medicare Two-way claim form. Log into your Medicare online account through myGov or Express Plus Medicare mobile app.
How are Medicare claims processed?
Your provider sends your claim to Medicare and your insurer. Medicare is primary payer and sends payment directly to the provider. The insurer is secondary payer and pays what they owe directly to the provider. Then the insurer sends you an Explanation of Benefits (EOB) saying what you owe, if anything.
Which of the following do providers use to electronically submit claims?
NHA practice test 1QuestionAnswerWhich of the following blocks should the billing and coding specialist complete on the CMS 1500 claim form for procedures, services, or supplies?Block 24DWhich of the following do physicians use to electronically submit claims?Clearinghouse96 more rows
How do I make a Medicare claim on myGov?
Sign in to myGov and select Medicare. If you're using the app, open it and enter your myGov pin. On your homepage, select Make a claim. Make sure you have details of the service, cost and amount paid to continue your claim.
What is the Claims Mailing Address for Medicare?
There is no central address that all Medicare claims are sent to. Each state works with a company called a Medicare Administrative Contractor (MAC)...
How Do I File a Claim?
If you’re submitting a claim for reimbursement, you’ll need to print off a Patient Request for Medical Payment form (CMS-1490S). You can fill it ou...
Why would I need to file a claim?
As we mentioned, you may not need to file a claim if you’re on Medicare. Most of your claims will be filed for you if you’re on Original Medicare,...
What do I need to include when mailing a reimbursement claim?
Along with the completed Patient Request for Medical Payment form, you’ll also need to include:
Can I Submit a Claim Directly to Medicare If I Have Medicare Advantage?
No — if you have Medicare Advantage, all coverage decisions are made by the private insurer you purchased your policy from. So, if you have a Medic...
What is the Railroad Medicare claims address?
If you receive retirement benefits and Medicare through the Railroad Retirement Board, your claims are handled by a separate Medicare Administrativ...
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
What is CMS claim?
CMS’s claim is the amount that is determined to be owed to the Medicare program. This is the amount that was paid out by Medicare, less any prorated procurement costs (see 42 CFR 411.37) if the claim is in dispute.
When did Medicare start paying for inpatient hospital?
The Social Security Amendments of 1983 (P.L. 98-21) provided that, effective with cost reporting periods beginning on or after October 1, 1983, most Medicare payments for Part A hospital inpatient operating costs are to be made prospectively on a per discharge basis. Part A Inpatient Hospital operating costs include costs (including malpractice insurance cost) for general routine services, ancillary services, and intensive care type unit services. However, they exclude capital-related costs incurred prior to October1, 1991, when capital-related costs began to be paid based on a separate prospective payment rate and direct medical education costs (which are paid using a different method). Part B inpatient ancillary and outpatient service will continue to be paid retrospectively on a reasonable cost basis.
What is Medicare secondary payer?
These sections include, among other things, information regarding the implementation of this provision retroactively, the processing of current claims, the determination of the 18-month period in which Medicare may be secondary, and the method of calculating the Medicare secondary payment.
What is the HMO/CMP liability?
If a noncontracted physician provides a service to one of the cost-based HMO/CMP’s enrollees, and the physician is not a Medicare participating physician, the limit of the HMO/CMP’s liability is the lower of the actual charge or the limiting charge permitted under the statute for FFS Medicare. The HMO/CMP is responsible for beneficiary coinsurance and deductible payments.
What is CMS 2552?
Providers using cost reports other than Form CMS-2552 will utilize the principles outlined for Form CMS-2552. That is, separate apportionment and settlement schedules will be prepared by the provider for each Medicare HMO/CMP processing the provider’s bills and for non-HMO/CMP beneficiaries. Each set of schedules will apportion the appropriate cost centers between the applicable groups of Medicare patients and all other provider patients.
Does Medicare pay for WC?
Medicare may not pay for services that are payable under Workers’ Compensation (WC) laws. Where the Medicare cost-based HMO/CMP coordinates its own health organization with WC coverage, it will use the procedures developed by its own organization to identify and recover costs for services furnished to Medicare members. When the Medicare cost-based HMO/CMP does not coordinate benefits for its own organization, it must establish reasonable screening procedures to identify potential WC liability situations. If it is determined that Medicare has paid for items or services which can be or could have been paid for under WC, the Medicare payment constitutes an overpayment. All WC acts require that the employer furnish the employee with necessary medical and hospital services, medicines, transportation, apparatus, nursing care, and other necessary restorative items and services. For specific information regarding the WC plan of a particular governmental entity, contact the appropriate agency of the governmental entity. If payment for services cannot be made by WC because they were furnished by a source not authorized by WC, the services can be paid for by Medicare.
Does Medicare have recovery rights?
Also, Medicare has the right to recover its benefits from any entity, including a State Medicaid Agency that has been paid by the responsible third party. In other words, Medicare’s recovery rights when another third party is primary payer take precedence over the rights of any other entity. The superiority of Medicare’s recovery right over those of other entities, including Medicaid, derives from the preceding cited statute.
When does MA default enrollment start?
As outlined in the 2019 guidance, only MA organizations who meet the criteria outlined and are approved by CMS to conduct default enrollment for coverage effective dates of January 1, 2019 , or later.
When is the MA model enrollment period?
All enrollments with an effective date on or after January 1, 2021, must be processed in accordance with the revised guidance requirements, including the new model MA enrollment form. MA plans are expected to use the new model form for the 2021 plan year Annual Enrollment Period (AEP) which begins on October 15, 2020.
Medicare Advantage Inpatient Claim "Shadow Billing"
CMS requires hospitals and skilled nursing facilities (SNFs) to submit claims to the A/B MACs or Fiscal Intermediaries (FI) and to the Medicare Advantage (MA) plans for inpatient services provided to Medicare beneficiaries who are enrolled in an MA plan.
Hospitals
Inpatient Prospective Payment System (PPS) hospitals, Inpatient Rehabilitation Facilities (IRFs), and Long-Term Care Hospitals (LTCHs) must submit two claims for inpatient stays by Medicare Advantage beneficiaries.
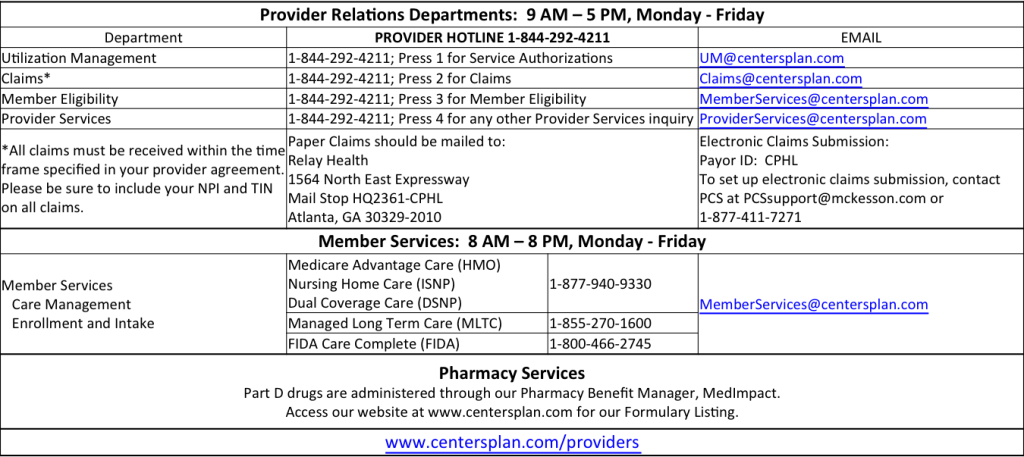
How to contact Change Healthcare?
If you have any further questions or experience any issues, you may reach out to Change Healthcare Support at 800-527-8133 (option 1) or send us an email. L.A. Care requires that an initial claim be submitted to the appropriate Claims Department under a specific timeline.
How does change healthcare work?
Making Change Healthcare our exclusive clearinghouse for the submission of electronic claims will provide you with the following benefits: 1 Allows our providers access to direct electronic claim submissions to Change Healthcare. In addition, providers will have the improved ability to verify electronic eligibility for our members via the 270/271 EDI Transaction and perform claim status lookup via the 276/277 Transaction. 2 Reduce administrative fees related to the submission of claims, eligibility, and claims status transactions. 3 Allows L.A. Care the functionality of creating and customizing edits in the frontend to help you improve the submission of your data and ensure your claims are processed accurately and in a timely manner. 4 Access to bill electronic claims at no cost to the provider. Please note that using the free billing option will only be available to those providers that do not currently have a business relationship with Change Healthcare and will allow only the direct submission of electronic claims to L.A. Care. 5 Access our step by step instruction video#N#(link is external)#N#of how to use ConnectCenter 6 Access to submit electronic attachments through Change Healthcare’s attachment portal. This functionality is currently being developed and will be available in the near future.
When Do I Need to File A Claim?
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining in detail your reason for subm…
Where Do I Send The Claim?
- The address for where to send your claim can be found in 2 places: 1. On the second page of the instructions for the type of claim you’re filing (listed above under "How do I file a claim?"). 2. On your "Medicare Summary Notice" (MSN). You can also log into your Medicare accountto sign up to get your MSNs electronically and view or download them an...