According to Medicare.gov, Medicare does pay for “part-time or intermittent home health aide services.” This is understandably confusing. It means that a home health worker may provide personal care services that a home health aide provides.
Full Answer
What services are covered by Medicare?
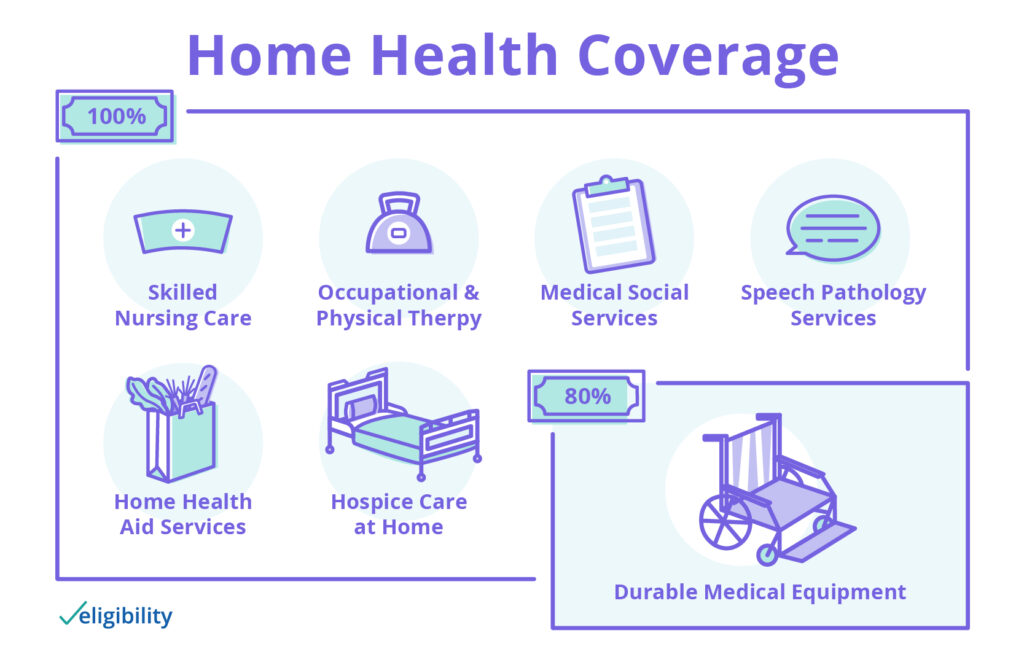
Home health services. Medicare Part A (Hospital Insurance) and/or Medicare Part B (Medical Insurance) cover eligible home health services like these: Part-time or "intermittent" skilled nursing care. Physical therapy. Occupational therapy. Speech-language pathology services. Medical social services.
How does Medicare pay for home health aides?
The home health aides must work for a Medicare-approved home health agency and your doctor must certify that you are homebound. These agencies agree to be paid the Medicare-approved amount and to be paid directly by Medicare.
How does Medicaid work with Medicare?
Medicaid, via Medicare Savings Programs, also helps to cover the costs of Medicare premiums, deductibles, and co-payments. Medicaid provides a wide variety of long-term care benefits and supports to allow persons to age at home or in their community.
What is the Centers for Medicare and Medicaid Services?
The Centers for Medicare and Medicaid Services, abbreviated as CMS, oversees both the Medicare and Medicaid programs. For the Medicaid program, CMS works with state agencies to administer the program in each state, and for the Medicare program, the Social Security Administration (SSA) is the agency through which persons apply.
What type of aid is offered for Medicare?
State Medicare Savings Programs (MSP) programs help pay premiums, deductibles, coinsurance, copayments, prescription drug coverage costs.
Does Medicare pay for home assistant?
Medicare may also pay for some in-home assistance with your daily needs for a short period following an illness or injury. But if you need long-term help with daily activities in your home, it's important to know that Medicare typically doesn't cover those caregiving services.
How Much Does Medicare pay for home health care per hour?
Medicare will cover 100% of the costs for medically necessary home health care provided for less than eight hours a day and a total of 28 hours per week. The average cost of home health care as of 2019 was $21 per hour.
How Long Will Medicare pay for home health care?
Medicare pays your Medicare-certified home health agency one payment for the covered services you get during a 30-day period of care. You can have more than one 30-day period of care. Payment for each 30-day period is based on your condition and care needs.
What can a registered nurse do for home care?
A registered nurse or licensed practical nurse may administer your home care which may include giving IV drugs, changing wound dressings, tube feedings, teaching about diabetes care, or certain injections. The home health aides must work for a Medicare-approved home health agency and your doctor must certify that you are homebound.
What is home health agency?
The home health agency will be responsible for all of your medical, nursing, and rehabilitative care and will communicate your needs to the managing physician. Your condition will be monitored and assessed regularly and will create discharge plans when appropriate.
Does Medicare cover home health care?
Home health care can be less costly than a long hospital stay and Medicare can help cover the costs. If your physician orders reasonable and medically necessary treatment of an illness or injury, Medicare will help pay for home health services as long as you meet certain criteria.
Do home health aides have to be Medicare approved?
The home health aides must work for a Medicare-approved home health agency and your doctor must certify that you are homebound. These agencies agree to be paid the Medicare-approved amount and to be paid directly by Medicare. The home health agency will be responsible for all of your medical, nursing, and rehabilitative care ...
Does Medicare Part B cover out of pocket costs?
The Medicare Part B deductible will apply. Many Medicare recipients choose to purchase supplemental insurance to help cover the out-of-pocket costs from Part A and Part B. If you have enrolled in a Medigap plan, it may help pay for deductibles and coinsurance associated with home health care.
Who is covered by Part A and Part B?
All people with Part A and/or Part B who meet all of these conditions are covered: You must be under the care of a doctor , and you must be getting services under a plan of care created and reviewed regularly by a doctor.
What is a medical social service?
Medical social services. Part-time or intermittent home health aide services (personal hands-on care) Injectible osteoporosis drugs for women. Usually, a home health care agency coordinates the services your doctor orders for you. Medicare doesn't pay for: 24-hour-a-day care at home. Meals delivered to your home.
What is an ABN for home health?
The home health agency should give you a notice called the Advance Beneficiary Notice" (ABN) before giving you services and supplies that Medicare doesn't cover. Note. If you get services from a home health agency in Florida, Illinois, Massachusetts, Michigan, or Texas, you may be affected by a Medicare demonstration program. ...
Does Medicare cover home health services?
Your Medicare home health services benefits aren't changing and your access to home health services shouldn’t be delayed by the pre-claim review process.
Can you get home health care if you attend daycare?
You can still get home health care if you attend adult day care. Home health services may also include medical supplies for use at home, durable medical equipment, or injectable osteoporosis drugs.
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
How to apply for medicaid?
How to Apply. To apply for Medicare, contact your local Social Security Administration (SSA) office. To apply for Medicaid, contact your state’s Medicaid agency. Learn about the long-term care Medicaid application process. Prior to applying, one may wish to take a non-binding Medicaid eligibility test.
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
What is dual eligible?
Definition: Dual Eligible. To be considered dually eligible, persons must be enrolled in Medicare Part A, which is hospital insurance, and / or Medicare Part B, which is medical insurance. As an alternative to Original Medicare (Part A and Part B), persons may opt for Medicare Part C, which is also known as Medicare Advantage.
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
How old do you have to be to qualify for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old. For persons who are disabled or have been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis), there is no age requirement. Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
Does Medicare cover out-of-pocket expenses?
Persons who are enrolled in both Medicaid and Medicare may receive greater healthcare coverage and have lower out-of-pocket costs. For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses. Medicaid does cover some expenses that Medicare does not, such as personal care assistance in the home and community and long-term skilled nursing home care (Medicare limits nursing home care to 100 days). The one exception, as mentioned above, is that some Medicare Advantage plans cover the cost of some long term care services and supports. Medicaid, via Medicare Savings Programs, also helps to cover the costs of Medicare premiums, deductibles, and co-payments.
What is a Medicare supplement?
If you think you or someone in your family might need custodial care, you may want to consider a long-term care insurance policy to help you cover the cost. A Medicare supplement (Medigap) plan may also help you pay some of the costs that Medicare won’t cover.
What is Medicare Part B?
Medicare Part B is medical coverage. If you need home health services but weren’t admitted to the hospital first, Part B covers your home healthcare. You do have to meet the other eligibility requirements, though.
How long does Medicare Part A cover?
If you were admitted to the hospital for 3 consecutive days or Medicare covered your stay in a skilled nursing facility, Part A will cover home healthcare for 100 days, as long as you receive home health services within 14 days of leaving the hospital or nursing facility .
How much does a home health aide cost?
Cost of hiring a caregiver. A 2019 industry survey on home health costs found that a home health aide is likely to cost an average of $4,385 per month. The same survey listed the average monthly cost of a caregiver to provide custodial care services as $4,290.
What do you need to be a home health aide?
You need a home health aide to help care for you while you recover. The home health agency providing your care is Medicare-approved or certified.
Does Medicare pay for physical therapy?
Physical therapy. If a physical therapist treats you in your home, Medicare is likely to pay for these kinds of services: assessment of your condition. gait training and exercises to help you recover from surgery, injuries, illnesses, or neurological conditions like stroke. postoperative wound care.
Does Medicare cover home care?
From time to time, original Medicare ( Part A and Part B) may cover medical care given to you in your home if you’re homebound. Medicare may also pay for some in-home assistance with your daily needs for a short period following an illness or injury. But if you need long-term help with daily activities in your home, ...
What services does Medicare cover for long term care?
Long-term care policies may also cover homemaker support services, such as meal preparation, laundry, light housekeeping and supervised intake of medications . Family Caregiver Support. Family caregivers are vital to the health and well-being of many Medicare recipients.
Do you have to be Medicare certified to be a home health agency?
The home health agency servicing you must be Medicare-certified, meaning they are approved by Medicare and accept assignment . If Medicare approves the claim for home health services, the authorized fees may be covered. Custodial Care for Day-to-Day Living.
Does Medicare cover hospital stays?
Some Medicare recipients are fortunate enough to have family members care for them and want to know if Medicare can help. Original Medicare is structured to cover costs incurred during hospital stays (Part A) and medical office visits (Part B).
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. for inpatient respite care.
What is hospice care?
hospice. A special way of caring for people who are terminally ill. Hospice care involves a team-oriented approach that addresses the medical, physical, social, emotional, and spiritual needs of the patient. Hospice also provides support to the patient's family or caregiver. care.
What happens when you choose hospice care?
When you choose hospice care, you decide you no longer want care to cure your terminal illness and/ or your doctor determines that efforts to cure your illness aren't working . Once you choose hospice care, your hospice benefit will usually cover everything you need.
How long can you be in hospice care?
After 6 months , you can continue to get hospice care as long as the hospice medical director or hospice doctor recertifies (at a face-to-face meeting) that you’re still terminally ill. Hospice care is usually given in your home but may also be covered in a hospice inpatient facility. Original Medicare will still pay for covered benefits for any health problems that aren’t part of your terminal illness and related conditions, but this is unusual. When you choose hospice care, you decide you no longer want care to cure your terminal illness and/or your doctor determines that efforts to cure your illness aren't working. Once you choose hospice care, your hospice benefit will usually cover everything you need.
Do you have to pay for respite care?
You may have to pay a small copayment for the respite stay . Care you get as a hospital outpatient (like in an emergency room), care you get as a hospital inpatient, or ambulance transportation, unless it's either arranged by your hospice team or is unrelated to your terminal illness and related conditions.
Does hospice pay for copay?
Hospice also provides support to the patient's family or caregiver. care. You pay a. copayment. An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug.
Does Medicare cover hospice care?
Any other services Medicare covers to manage your pain and other symptoms related to your terminal illness and related conditions, as your hospice team recommends. Medicare doesn’t cover room and board when you get hospice care in your home or another facility where you live (like a nursing home).