Medicare pays first, and Medicaid pays second. Medicaid never pays first for services covered by Medicare. It only pays after Medicare, employer group health plans, and/or Medicare Supplement
Medigap
Medigap refers to various private health insurance plans sold to supplement Medicare in the United States. Medigap insurance provides coverage for many of the co-pays and some of the co-insurance related to Medicare-covered hospital, skilled nursing facility, home health care, ambulance, durable medical equipment, and doctor charges. Medigap's name is derived from the notion that it exists to …
Who pays first – Medicare or Medicaid?
In some situations, Medicare will serve as your primary payer, which means Medicare pays first. Your other insurance coverage will then serve as your secondary payer. You are “dual-eligible” (entitled to both Medicare and Medicaid ).
Does Medicare pay first or Tricare pay first?
In most circumstances, Medicare pays first for any covered services. TRICARE will pay second and can pick up some of the expenses like your Medicare deductibles and coinsurance. TRICARE may also pay for some services that Medicare does not cover. You will be responsible though for any services that neither program covers.
What is the difference between Original Medicare and Medicare Advantage?
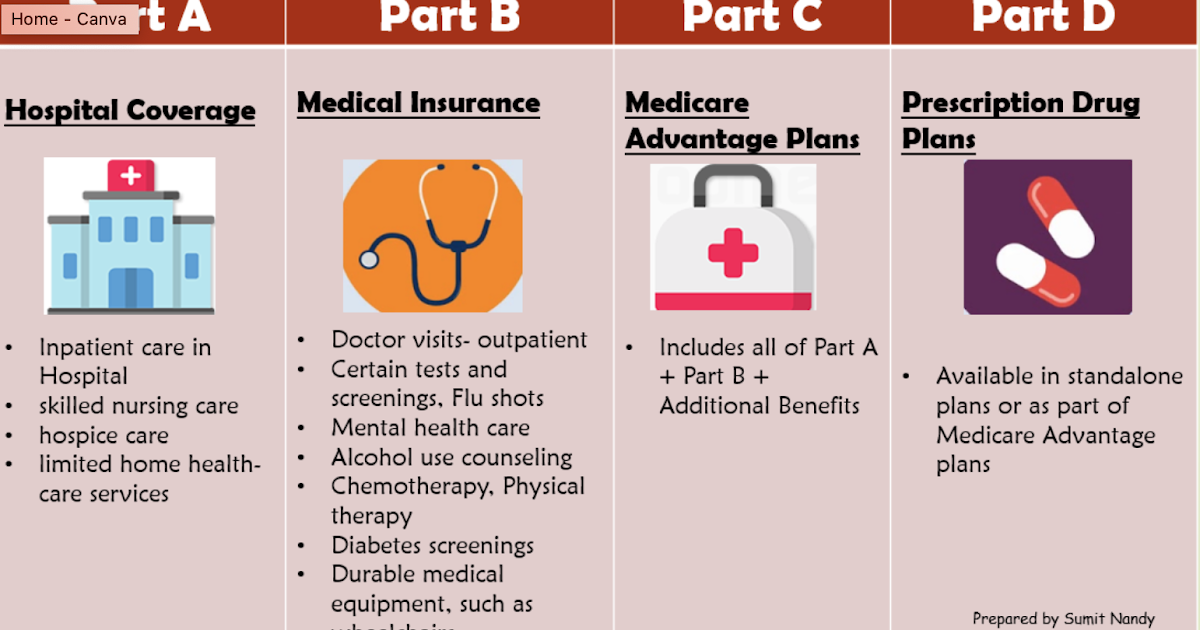
Original Medicare refers to Part A and Part B, but there are others as well: Part A covers hospital inpatient care. Part B covers outpatient care. This includes: Part C is Medicare Advantage (MA), an optional managed-care alternative to original Medicare.
Who pays first cobra or Medicare?
For most people on COBRA, Medicare pays first, except in situations where your Medicare is awarded due to End Stage Renal Disease. There are certain enrollment periods surrounding Medicare and COBRA, so you should always consult your employer’s plan benefits administrator for guidance.

What came first Medicare or Medicaid?
On July 30, 1965, President Lyndon B. Johnson signed into law the Social Security Act Amendments, popularly known as the Medicare bill. It established Medicare, a health insurance program for the elderly, and Medicaid, a health insurance program for the poor.
Is Medicare first or secondary?
Medicare pays first and your group health plan (retiree) coverage pays second . If the employer has 100 or more employees, then the large group health plan pays first, and Medicare pays second .
Is Medicare billed first?
Medicare pays first for your health care bills, before the IHS. However, if you have a group health plan through an employer, and the employer has 20 or more employees, then generally the plan pays first and Medicare pays second. If your employer has fewer than 20 employees, Medicare generally pays first.
Which insurance is primary when you have two?
If you have two plans, your primary insurance is your main insurance. Except for company retirees on Medicare, the health insurance you receive through your employer is typically considered your primary health insurance plan.
Is Medicare always the primary?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
Does Medicare coverage start the month you turn 65?
The date your coverage starts depends on which month you sign up during your Initial Enrollment Period. Coverage always starts on the first of the month. If you qualify for Premium-free Part A: Your Part A coverage starts the month you turn 65.
How do you determine which health insurance is primary?
Primary insurance is a health insurance plan that covers a person as an employee, subscriber, or member. Primary insurance is billed first when you receive health care. For example, health insurance you receive through your employer is typically your primary insurance.
Does Medicare send claims to secondary insurance?
Medicare will send the secondary claims automatically if the secondary insurance information is on the claim. As of now, we have to submit to primary and once the payments are received than we submit the secondary.
What is the difference between Medicare and Medicaid?
The difference between Medicaid and Medicare is that Medicaid is managed by states and is based on income. Medicare is managed by the federal government and is mainly based on age. But there are special circumstances, like certain disabilities, that may allow younger people to get Medicare.
What is the birthday rule?
Birthday Rule: This is a method used to determine when a plan is primary or secondary for a dependent child when covered by both parents' benefit plan. The parent whose birthday (month and day only) falls first in a calendar year is the parent with the primary coverage for the dependent.
What happens when you have 2 health insurance plans?
If you have multiple health insurance policies, you'll have to pay any applicable premiums and deductibles for both plans. Your secondary insurance won't pay toward your primary's deductible. You may also owe other cost sharing or out-of-pocket costs, such as copayments or coinsurance.
Is it smart to have two health insurance plans?
Having two health plans can help cover normally out-of-pocket medical expenses, but also means you'll likely have to pay two premiums and face two deductibles. Your primary plan initially picks up coverage costs, followed by the secondary plan. You might still owe out-of-pocket costs at the end.
What is Medicare and Medicaid?
Medicare and Medicaid are government-run health care programs meant to serve different populations: Medicare is an insurance program that primarily serves people 65 and older, regardless of income. Medicaid is an assistance program that provides health insurance to low-income people of all ages.
Is Medicare a federal or state program?
Medicare: Medicare is a federal program. What’s covered and what people pay is generally the same in every state. Medicaid: Medicaid is a state and federal program. The federal government makes the guidelines, but the program is administered by states so eligibility requirements vary.
Does Medicaid cover nursing home costs?
Medicaid can help pay Medicare premiums, deductibles and copays for impoverished people. Medicaid also can pay for nursing home and personal care services, expenses that aren’t typically covered by Medicare.
Does Medicare cover ALS?
Medicare also covers younger people with disabilities and certain diseases, including end stage renal disease (kidney failure) and Lou Gehrig’s disease or amyotrophic lateral sclerosis (ALS). People with higher incomes pay larger premiums for certain parts of Medicare, but eligibility isn’t limited by income.
Is Medicaid based on income?
Medicaid: Medicaid coverage is based on income. Medicaid is available in every state to those with incomes below the poverty line. Under the Affordable Care Act, most states have expanded Medicare eligibility to people with incomes up to 133% of the federal poverty line.
Does Medicaid cover Lou Gehrig's disease?
There are exceptions: People, including children, with end-stage renal disease or Lou Gehrig’s disease may qualify through the work history of a spouse or parent. Medicaid: Medicaid covers dependents. Medicaid and the related Children’s Health Insurance Program provide health insurance to more than 35 million children.
Does Medicare cover doctor visits?
Medicare Part B, which covers doctor’s visits, and Part D, which covers prescriptions, also require paying premiums. Medicaid: Medicaid is typically free. Some people may have to pay small copays. Medicaid can also make a claim against people’s assets after they die, but most people receiving Medicaid have few or no assets.
What is Medicare insurance?
Medicare. Medicare is an insurance program. Medical bills are paid from trust funds which those covered have paid into. It serves people over 65 primarily, whatever their income; and serves younger disabled people and dialysis patients. Patients pay part of costs through deductibles for hospital and other costs.
Do you pay for medical expenses on medicaid?
Patients usually pay no part of costs for covered medical expenses. A small co-payment is sometimes required. Medicaid is a federal-state program. It varies from state to state. It is run by state and local governments within federal guidelines.
Is Medicare a federal program?
Small monthly premiums are required for non-hospital coverage. Medicare is a federal program. It is basically the same everywhere in the United States and is run by the Centers for Medicare & Medicaid Services, an agency of the federal government.
Medicare Fast Facts
Here’s a quick breakdown of some quick facts to give you an overview of Medicare.
Medicaid Fast Facts
You might qualify for medicaid, and it could offer you substantial coverage depending on which state you live in.
A Closer Look at Medicare
This federal program helps pay for a number of different expenses related to health care through the US Department of Health and Human Services. The most common group that takes advantage of Medicare are senior citizens, after turning 65 years old.
A Closer Look at Medicaid
This program assists people who meet a certain criteria for limited income. People with less resources should still be able to access necessary health care, and Medicare can help fill that void. Could it be better? Most certainly.
When did Medicare expand to cover disabled people?
When Congress expanded Medicare to cover seriously disabled Americans in 1972, the law also mandated that SSDI two-year waiting period. For this reason, the Social Security Administration (SSA) isn’t likely to change that requirement anytime soon.
What is Medicaid insurance?
Medicaid is a need-based joint federal and state insurance program that covers low-income individuals and families. That said, Medicaid coverage can vary significantly from state to state. That’s because the federal government covers up to 50% of each state’s Medicaid program costs.
How does Medicare work?
Medicare provides coverage for Americans who: Here’s how Medicare payments work: Essentially, your Social Security taxes go into a trust fund that grows throughout your working years. Money from that trust fund then pays all eligible bills incurred by people covered under the Medicare program.
How long do you have to wait to apply for SSDI?
(Those five months cover the waiting period before you became eligible to apply for SSDI benefits.) But if your disability started long before you applied for SSDI, that time counts toward your mandatory two-year waiting period.
What is Medicare Part B?
Medical: Medicare Part B works like most private insurance policies and covers doctor’s visits, lab work, and visits to the emergency room. Prescription Drugs: Medicare Part D helps cover prescribed medication costs. Medicare Part A and B participants are eligible for Part D (or you can purchase it as a standalone plan).
Is there a waiting period for Medicare vs Medicaid?
If you’re getting SSI benefits, you’re also automatically enrolled in the Medicaid program unless you live in: If you reside in an automatic-enrollment state, there’s no waiting period for Medicaid coverage.
Does Medicaid cover everyone?
This means all remaining Medicaid program costs must be paid for at the state level. Unlike Medicare, Medicaid isn’t available to everyone and it has very strict eligibility requirements. To qualify for Medicaid coverage, you must either already be receiving SSI benefits or fit within a mandatory eligibility group.
Which pays first, Medicare or ESRD?
The group health plan pays first for qualified services, and Medicare is the secondary payer. You have ESRD and COBRA insurance and have been eligible for Medicare for 30 months or fewer. COBRA pays first in this situation.
How long do you have to be on Cobra to get Medicare?
You have ESRD and COBRA insurance and have been eligible for Medicare for at least 30 months. COBRA is the secondary payer in this situation, and Medicare pays first for qualified services. You are 65 or over – or you are under 65 and have a disability other than ESRD – and are covered by either COBRA insurance or a retiree group health plan.
What is Medicare Advantage?
A Medicare Advantage plan replaces your Original Medicare coverage. In addition to those basic benefits, Medicare Advantage plans can also offer some additional coverage for things like prescription drugs, dental, vision, hearing aids, SilverSneakers programs and more.
Is Medicare a secondary payer?
Medicare serves as the secondary payer in the following situations: You are 65 or older and are covered by a group health plan because you or your spouse is still working and the employer has 20 or more employees. The group health plan is the primary payer, and Medicare pays second.
Does tricare work with Medicare?
You may use both types of insurance for your health care , but they will operate separately from each other. TRICARE does work with Medicare. Active-duty military personnel who are enrolled in Medicare may use TRICARE as a primary payer, and then Medicare pays second as a secondary payer. For inactive members of the military who are enrolled in ...
Is Medicare Part A or Part B?
While you must remain enrolled in Medicare Part A and Part B (and pay the associated premiums), your Medicare Advantage plan serves as your Medicare coverage. Medicare Part D, which provides coverage for prescription drugs, is another type of private Medicare insurance.
Is Medicaid a dual payer?
You are “dual-eligible” ( entitled to both Medicare and Medicaid ). Medicaid becomes the secondary payer after Medicare pays first. You are age 65 or older and are covered by a group health plan because you or your spouse is still working and the employer has fewer than 20 employees.
Who pays first for Medicare?
When it comes to Medicare, ‘Who Pays First’ is a very common dilemma these days. That’s because people are working longer than ever and often have other insurance coverage in place alongside Medicare. In most cases of other coverage, one insurance becomes the primary payer, and the other insurance becomes the secondary payer.
Is Medicare the same as Medicaid?
Original Medicare is a federal health insurance program for people age 65 or older, and for people with certain disabilities. Medicaid is a joint federal and state program for people with limited incomes and assets. If you have qualified for both, Medicare will always pay first, and Medicaid will pay second.
Is Medicare primary or secondary?
Employer health plans with 20 or more employees will be primary and Medicare will be secondary. If there are less than 20 employees, then Medicare is primary and your group health plan is secondary. Again, in both of these situations, you would not need a Medigap plan because you already have a primary and secondary payer.
Does Medicare pay for retirees?
Medicare and Retiree Coverage. If you have group health benefits through a former employer or a spouse’s former employer, Medicare pays first. This means you must be enrolled in both Medicare Parts A and B. After Medicare pays out its benefits, it will send the remainder of those bills on to your retiree health plan.
Is Cobra more expensive than Medicare?
However, COBRA benefits for people over 65 can often be enormously expensive. Be sure to compare costs/benefits against the cost of Medicare with a Medigap plan. Often we find the Medigap option to be significantly less expensive.
Can you get Medicare early if you are 65?
Medicare and Group Health Coverage for Beneficiaries Under 65. Some people qualify for Medicare early due to a disability. If that employee works for a company with less than 100 employees, Medicare will be primary. If the employer has more than 100 employees, the larger group health plan will pay first, and Medicare will pay secondary.
Do you have to use Medicare or VA?
If you wish to use your VA benefits, you must seek care from a VA facility. Many Veterans choose to have Medicare as well as VA benefits so that they have the freedom to treat with a civilian doctor if they wish to do so.
How to learn more about Medicare?
How to Learn More About Your Medicare Options. Primary insurance isn't too hard to understand; it's just knowing which insurance pays the claim first. Medical billing personnel can always help you figure it out if you're having trouble. While it's not hard to understand primary insurance, Medicare is its own beast.
Is Medicare primary insurance in 2021?
Updated on July 13, 2021. Many beneficiaries wonder if Medicare is primary insurance. But, the answer depends on several factors. While there are times when Medicare becomes secondary insurance, for the most part, it’s primary. Let’s go into further detail about what “primary” means, and when it applies.
Is Medicare a primary or secondary insurance?
Mostly, Medicare is primary. The primary insurer is the one that pays the claim first, whereas the secondary insurer pays second. With a Medigap policy, the supplement is secondary. Medicare pays claims first, and then Medigap pays. But, depending on the other policy, you have Medicare could be a secondary payer.
Does Medicare pay your claims?
Since the Advantage company pays the claims, that plan is primary. Please note that Medicare WON’T pay your claims when you have an Advantage plan. Medicare doesn’t become secondary to an Advantage plan. So, you’ll rely on the Advantage plan for claim approvals.
Can you use Medicare at a VA hospital?
Medicare and Veterans benefits don’t work together; both are primary. When you go to a VA hospital, Veteran benefits are primary. Then, if you go to a civilian doctor or hospital, Medicare is primary. But, you CAN’T use Veterans benefits at a civilian doctor. Also, you can’t use Medicare benefits at the VA.
Is Medicare a part of tricare?
Medicare is primary to TRICARE. If you have Part A, you need Part B to remain eligible for TRICARE. But, Part D isn’t a requirement. Also, TRICARE covers your prescriptions. Your TRICARE will be similar to a Medigap plan; it covers deductibles and coinsurances.
