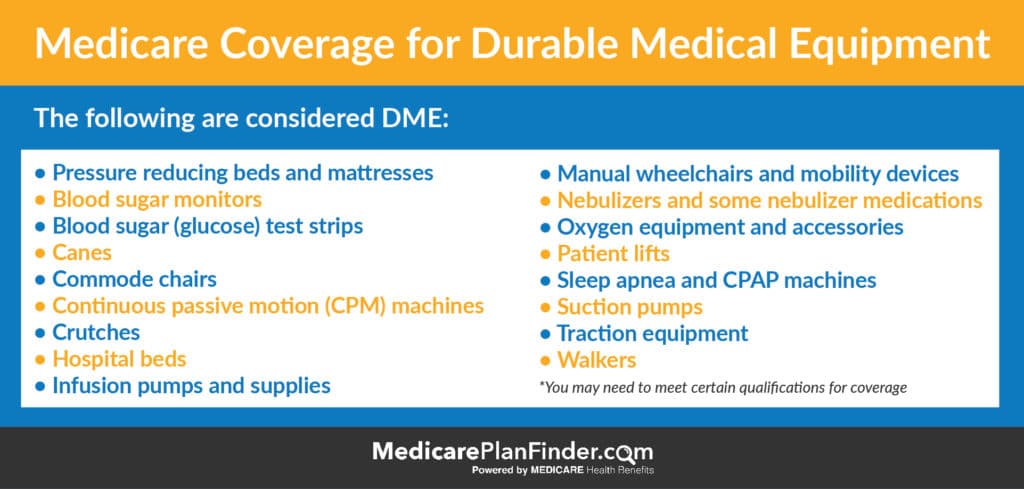
The list of DME that is covered by Medicare includes (but is not limited to):
- Air-fluidized beds and various other support surfaces
- Blood pressure monitors
- Blood sugar monitors
- Blood sugar test strips
- Canes
- Catheters
- Cochlear implants
- Commode chairs
- Continuous passive motion machines
- Continuous Positive Airway Pressure (CPAP) devices and accessories
- Crutches
- Diabetic supplies
- Hospital beds
- Knee braces
- Ostomy supplies
- Pacemakers
- Patient lifts
- Prosthetic devices
- Suction pumps
- Traction equipment
- Wheelchairs
- Walkers
- Blood sugar meters.
- Blood sugar test strips.
- Canes.
- Commode chairs.
- Continuous passive motion devices.
- Continuous Positive Airway Pressure (CPAP) devices.
- Crutches.
- Hospital beds.
What DME does Medicare pay for?
What durable medical equipment does Medicare cover? Medicare covers a range of items, supplies and equipment such as durable medical equipment. The list of DME that is covered by Medicare includes (but is not limited to): Air-fluidized beds and various other support surfaces Blood pressure monitors Blood sugar monitors Blood sugar test strips Canes
What medical supplies are covered by Medicare?
The term DME is defined as equipment which:
- Can withstand repeated use; i.e., could normally be rented and used by successive patients;
- Is primarily and customarily used to serve a medical purpose;
- Generally is not useful to a person in the absence of illness or injury; and,
- Is appropriate for use in a patient’s home.
What is considered DME?
What Is Durable Medical Equipment?
- Safety Devices. Safety devices many seniors have in their homes include shower chairs and guard rails, lift bars and bumpers for sharp edges.
- Mobility Aids. Many seniors experience increasingly limited mobility as they age. ...
- Therapy Equipment. Some DME is intended to help seniors recover from injury or to improve a medical condition. ...
Does Medicare cover DME?
Typical DME that Medicare will cover includes hospital beds, wheelchairs, walkers and home oxygen equipment. Medicare will not cover any disposable supplies — unless the supplies are used in conjunction with recognized durable medical equipment that is used inside the home.

What are Dmepos items?
Master List of Durable Medical Equipment, Prosthetics, Orthotics and Supplies (DMEPOS) Items Potentially Subject to Conditions of Payment. CMS has streamlined regulatory requirements to help simplify DMEPOS payment requirements and reduce provider and supplier burden.
What is an example of durable medical equipment?
Oxygen concentrators, monitors, ventilators, and related supplies. Personal care aids like bath chairs, dressing aids, and commodes. Mobility aids such as walkers, canes, crutches, wheelchairs, and scooters. Bed equipment like hospital beds, pressure mattresses, bili lights and blankets, and lift beds.
What is Medicare DME?
DME is reusable medical equipment, like walkers, wheelchairs, or hospital beds. If I have Medicare, can I get DME? Anyone who has Medicare Part B (Medical Insurance) can get DME as long as the equipment is medically necessary.
Are shower chairs considered DME?
Shower chairs are classified as Durable Medical Equipment (DME), and depending on the specific mobility or balance issues you have been diagnosed with, these chairs may or may not be covered by your Medicare insurance. What are shower chairs? Shower chairs may also be called shower or bath seats, stools, or benches.
Are disposable needles considered DME?
Durable medical supplies can also include disposable gloves that a patient or caregiver may wear during a daily treatment. Supplies can also include bandages, catheter equipment, needles for injection kits and diapers. If it is used once and then thrown away, it is considered a durable medical supply.
Are bandages durable medical equipment?
What Is Not Durable Medical Equipment? Not every item an older adult needs for safety, mobility or therapy counts as durable medical equipment. Gauze bandages, for example, are disposable supplies.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
Is a knee brace durable medical equipment?
Orthotic devices like braces are otherwise known as Durable Medical Equipment. Braces may be used to support the knee, neck, arm, or back. Combining the use of orthotic devices with other treatments may delay the need for a surgical procedure.
Which of the following is excluded from Medicare coverage?
Non-medical services, including a private hospital room, hospital television and telephone, canceled or missed appointments, and copies of x-rays. Most non-emergency transportation, including ambulette services. Certain preventive services, including routine foot care.
Is a raised toilet seat covered by Medicare?
Medicare generally considers toilet safety equipment such as risers, elevated toilet seats and safety frames to be personal convenience items and does not cover them. Medicare Advantage may offer some coverage if your plan includes supplemental OTC benefits.
Does Medicare cover bed pans?
Medicare covers a commode chair with detachable arms (E0165) if the detachable arms feature is necessary to transfer the patient, or if the patient's body requires extra width. Bed Pans (autoclavable hospital type): Covered - Medicare covers bed pans if the patient is bed-confined.
Are grab bars covered by Medicare?
Grab bars are considered durable medical equipment (DME) by Medicare, falling into the same category as walkers, canes, and stair lifts. To qualify for this classification, the product must be something used in your home for a medical reason.
What is DME in Medicare?
In addition to covering a wide range of services, Medicare also covers certain medical devices, items and supplies often referred to as durable medical equipment (DME). The Centers for Medicare & Medicaid Services (CMS) defines durable medical equipment as special medical equipment, such as wheelchairs or hospital beds, ...
What is a DME?
The classification of DME extends to DMEPOS, or durable medical equipment, prosthetics, orthotics and supplies. Items in this classification include prosthetics such as artificial limbs or other body parts, along with things like braces and wound dressings.
What is DME insurance?
DME and Medicare Supplement Insurance. Medicare Supplement Insurance plans, or Medigap, provide coverage for many of the out-of-pocket costs that Medicare Part A and Part B don't cover.
How many different types of providers can you get Durable Medical Equipment?
Durable medical equipment can typically be obtained from three different types of providers, and each may carry a different cost for the same item. Be sure to check with your doctor and your DME supplier to find out how much your equipment may cost. Participating providers.
What is a participating provider?
Participating providers. A participating provider accepts the Medicare-approved amount as full payment for their equipment. The Medicare-approved amount is the amount of money that Medicare has determined it will pay for particular services and items. Non-participating providers.
Is Medicare Advantage covered by Original Medicare?
Many Medicare Advantage plans also offer a number of benefits not covered by Original Medica re. This includes providing coverage for certain items that can help make it easier for people to age in place at home, some of which are not currently classified as DME and therefore not covered by Original Medicare.
Is Medicare Advantage the same as DME?
DME and Medicare Advantage plans. By law, Medicare Advantage plans are required to provide at least the same benefits as Medicare Part A and Part B (known together as Original Medicare). This means that Medicare Advantage plans provide the same coverage for qualified DME as Original Medicare.
Description Information
Please Note: This may not be an exhaustive list of all applicable Medicare benefit categories for this item or service.
National Coverage Analyses (NCAs)
This NCD has been or is currently being reviewed under the National Coverage Determination process. The following are existing associations with NCAs, from the National Coverage Analyses database.
What are some examples of DME?
Some examples of DME are walkers, hospital beds, home oxygen equipment, diabetes self-testing equipment (and supplies), and certain nebulizers and their medications (non-disposable). Wheelchairs and power scooters are also included in the list of DME, but additional rules apply. (See below.)
What is DME in medical terms?
Medicare defines durable medical equipment, or DME, as reusable medical equipment that has been deemed medically necessary. Your doctor or another health care provider determines what equipment you need per Medicare guidelines. He or she assesses your health condition, what equipment can be used in your home and what equipment you are able to use.
What is the difference between Medicare Advantage and Original?
The main difference between Original Medicare and Medicare Advantage lies in how you get a durable medical equipment item covered. For example, a Medicare Advantage plan may require prior authorization in order for items to be covered.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
How long does a durable medical equipment item last?
Used because of an illness or injury. Able and necessary to be used at home (though you may also use it outside your home)*. Likely to last for three or more years.
What is Part B for Medicare?
Original Medicare’s Part B covers durable medical equipment items when your Medicare-enrolled doctor or health care provider prescribes it for you to use at home. Once you have the doctor’s prescription, you can take it to any Medicare-enrolled supplier.
What is considered durable medical equipment?
Durable medical equipment that is not suitable for at-home use such as paraffin bath units used in hospitals or skilled nursing facilities. Most items that are considered as providing convenience or comfort (ex. air conditioners) Items that are thrown away after use or that aren’t used with equipment (ex. catheters)
What is assignment in Medicare?
Assignment —An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
Does Medicare pay for DME repairs?
Medicare will pay 80% of the Medicare-approved amount (up to the cost of replacing the item) for repairs. You pay the other 20%. Your costs may be higher if the supplier doesn’t accept assignment.
What is Medicare Coverage for Durable Medical Equipment (DME)?
What is Medicare Coverage for Durable Medical Equipment (DME)? Whether you use a walker, a blood pressure monitor, crutches or other items that are used to improve your health, there’s no doubt that having access to medical equipment can improve your quality of life and maybe even save it.
How does Medicare cover durable medical equipment (DME)?
Original Medicare uses the term “durable medical equipment” or “DME” to refer to medical equipment items it covers. Durable medical equipment as it pertains to Medicare includes items that are intended for repeated use. Per this definition, single-use items are usually disqualified from DME coverage.
What Part of Medicare Covers Durable Medical Equipment?
Medicare benefits are supplied via different parts of the program. Medicare Part B is the outpatient benefit and covers not only things like doctor visits and surgery, but it also covers DME. For most Medicare recipients, DME is covered at the standard Part B rate of 80%.
Rentals vs. Purchases
In some cases, a piece of DME will need to be rented prior to a full purchase being covered. Medicare Part B usually covers rentals of DME that are eligible for purchase, but timeframe requirements for rentals before purchase may vary.
Non-Prescription Durable Medical Equipment
It’s important to note that Medicare’s coverage of DME only extends to items which have been ordered by a Medicare-participating physician. This means that you will not be able to receive coverage for items that you purchase on your own, including equipment for sale at retail health stores and pharmacies.
Medicare Advantage Coverage for DME
Medicare Advantage plans must include the same Part A and Part B benefits as Original Medicare, but many plans offer additional coverage. Check with your plan directly for questions regarding your DME. You may need to get your equipment from a supplier within your plan’s network.
How to get DME approved by Medicare?
You can get Medicare-approved DME in several ways: from your doctor, in-person at a supplier, or online. First, your doctor may supply it, such as a k nee or ankle brace they keep on-site. Second, your doctor may give you a list of Medicare suppliers in your area. Third, you can obtain a list of Medicare-approved suppliers from Medicare’s website . ...
What is DME in Medicare?
What is DME Medicare? Durable medical equipment or DME is the equipment you need to use in your home to support your health and keep you safe. Examples of DME include walkers, oxygen, blood sugar monitors, patient lifts, sleep apnea devices, and more. Medicare has a long list of DME it will cover, but you have to go through a Medicare-approved ...
What is Medicare Advantage?
Medicare Advantage plans are when you choose a private insurance company to fulfill your Medicare benefits. Medicare requires all Medicare Advantage plans to cover DME at the same level as Original Medicare plans. However, the specific costs and suppliers may depend on your plan.
What is covered by Medicare Part B?
If you have Medicare Part B, your plan covers certain medically necessary durable medical equipment 1 Medicare will pay for a portion of durable medical equipment (DME), including wheelchairs, canes and hospital beds. 2 Medicare defines what qualifies as DME, including items used repeatedly, needed for a medical reason, and will usually last at least three years. 3 You’ll usually need a doctor’s “prescription” and must purchase the items from a Medicare-approved supplier to get reimbursement. 4 Medicare will typically pay 80 percent for renting or purchasing DME, and you’ll pay the remaining 20 percent.
How long does a DME last?
Medicare defines what qualifies as DME, including items used repeatedly, needed for a medical reason, and will usually last at least three years. You’ll usually need a doctor’s “prescription” and must purchase the items from a Medicare-approved supplier to get reimbursement.
What does it mean when a company sells medical equipment?
When a company that sells medical equipment is a Medicare supplier, they’ve agreed to charge Medicare-approved prices for an item. This means if you are purchasing a cane from a certain medical supplier, the price should be similar to that of other suppliers. Some suppliers will bill Medicare directly for you.
What is the process of certifying medical equipment?
While these can vary somewhat based on the medical equipment, the general process is: Doctor’s prescription: A doctor or other healthcare provider must certify you need the equipment. Your doctor must participate in Medicare and provide written confirmation the item is medically necessary for you.
What are the items that are not covered by Medicare?
Surgical dressings. Immunosuppressive drugs. Erythropoietin (EPO) for home dialysis patients. Therapeutic shoes for diabetics. Oral anticancer drugs. Oral antiemetic drugs (replacement for intravenous antiemetics) Some items may not meet the definition of a Medicare benefit or may be statutorily excluded.
What are the benefits of DME?
In order for an item to be covered by the Durable Medical Equipment Medicare Administrative Contractor (DME MAC), it must fall within one of ten benefit categories. Medicare Part B covered services processed by the DME MAC fall into the following benefit categories specified in Section 1861 (s) of the Social Security Act: 1 Durable medical equipment (DME) 2 Prosthetic devices 3 Leg, arm, back and neck braces (orthoses) and artificial leg, arm and eyes, including replacement (prostheses) 4 Home dialysis supplies and equipment 5 Surgical dressings 6 Immunosuppressive drugs 7 Erythropoietin (EPO) for home dialysis patients 8 Therapeutic shoes for diabetics 9 Oral anticancer drugs 10 Oral antiemetic drugs (replacement for intravenous antiemetics)
What is Medicare Part B?
Medicare Part B covered services processed by the DME MAC fall into the following benefit categories specified in Section 1861 (s) of the Social Security Act: Durable medical equipment (DME) Prosthetic devices. Leg, arm, back and neck braces (orthoses) and artificial leg, arm and eyes, including replacement (prostheses)