What does Medicare Part a cover?
For Medicare beneficiaries, when ZEMAIRA is given at home, the drug may be covered under either Part B or Part D, depending on circumstances. For reimbursement support, please call ZEMAIRA Connect at 1-866-ZEMAIRA or 1-866-936-2472.
What's a Medicare health plan?
Prescription Hope is not a Zemaira coupon card or insurance policy. Our program is also not a Zemaira Generic. Prescription Hope is a national advocacy program that works with any coverage you may already have. Although Prescription Hope is not a Zemaira coupon, individuals looking for a Zemaira coupon can find more savings through Prescription ...
Who pays first-Medicare or group health insurance?
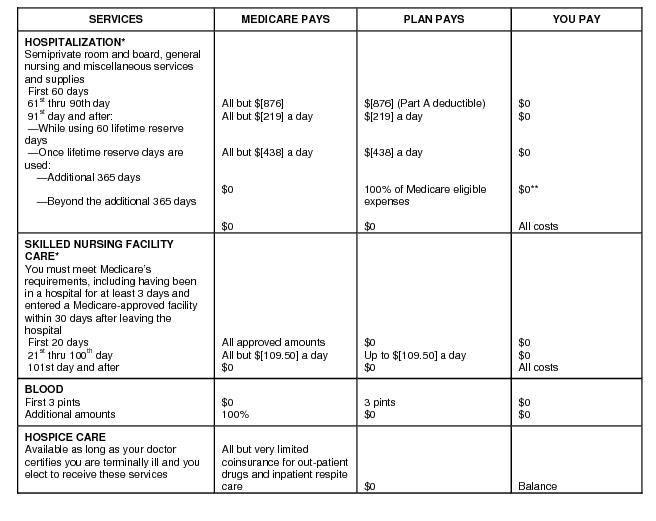
Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. and. Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. benefits to people who enroll in the plan.
Is there a third payer for health insurance?
Your Medicare coverage choices. Learn about the 2 main ways to get your Medicare coverage — Original Medicare or a Medicare Advantage Plan (Part C). What Part A covers. Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care. What Part B covers
Does Medicare pay for Temodar?
The oral form of temozolomide is covered under Medicare part B for Medicare recipients. Make sure your pharmacist knows to process this prescription through your Medicare part B and NOT part D.
Does Medicare Part B pay for capecitabine?
Do Medicare prescription drug plans cover capecitabine? No. In general, Medicare prescription drug plans (Part D) do not cover this drug.
Does Medicare pay for brovana?
BROVANA is covered under Medicare Part B Then bring your BROVANA prescription, along with any primary and supplemental insurance information, to your pharmacy.
Does Medicare Part B cover Lenvima?
Do Medicare prescription drug plans cover Lenvima? Yes. 100% of Medicare prescription drug plans cover this drug.
Is Xeloda covered by Medicare?
No. In general, Medicare prescription drug plans (Part D) do not cover this drug. Be sure to contact your specific plan to verify coverage information. A limited set of drugs administered in a doctor's office or hospital outpatient setting may be covered under Medical Insurance (Part B).
Is capecitabine a chemotherapy?
Capecitabine is a type of chemotherapy. It is used as a treatment for different types of cancer, including bowel cancer. You might have capecitabine on its own or with other chemotherapy drugs. You might also have it with radiotherapy.Nov 16, 2021
Is budesonide covered by Medicare Part B?
Do Medicare prescription drug plans cover budesonide? Yes. 100% of Medicare prescription drug plans cover this drug.
What is comparable to Brovana?
Brovana is used to treat your COPD long term. For sudden breathing problems, your doctor will likely recommend a rescue inhaler such as albuterol (ProAir) or levalbuterol (Xopenex). These medications work much faster than Brovana to treat COPD flare-ups.Oct 4, 2019
What does Brovana cost?
About Brovana It is always used with another medicine for COPD. Do not use this medicine to treat an acute COPD attack or bronchospasm. The lowest GoodRx price for the most common version of generic Brovana is around $243.90, 80% off the average retail price of $1,249.16.
Is immunotherapy covered by Medicare?
Immunotherapy is covered under Medicare as a cancer treatment. Immunotherapy drugs such as Keytruda and Opdivo are typically covered under Medicare if the medications are deemed medically necessary. Expect to pay certain out-of-pocket costs for immunotherapy cancer treatment even if you are covered by Medicare.
Is Cabometyx covered by Medicare Part B?
Do Medicare prescription drug plans cover Cabometyx? Yes.
Is Ibrance covered by Medicare Part B?
Do Medicare prescription drug plans cover Ibrance? Yes.
Who is Prescription Hope?
Prescription Hope is a nationally recognized prescription medication access program, headquartered in Columbus, Ohio. Prescription Hope offers access to over 1,500 brand-name medications through patient assistance programs. All you pay is a set service fee of $50 for each medication per month.
Do I Qualify For Zemaira Patient Assistance With Prescription Hope?
Prescription Hope works with thousands of Americans every month, obtaining prescription medications on their behalf for the set price of $50.00 per month per medication.
Is Prescription Hope A Zemaira Coupon Card, Generic, Or Insurance Product?
Prescription Hope is not a Zemaira coupon card or insurance policy. Our program is also not a Zemaira Generic. Prescription Hope is a national advocacy program that works with any coverage you may already have.
Can Prescription Hope Get My Zemaira If I Have Health Insurance Coverage?
Because Prescription Hope is not a health insurance plan, our program works alongside any coverage you may currently have to obtain your Zemaira medication at an affordable price. Our national advocacy program does not have medication tiers, copays, or deductibles.
Zemaira: Prescribed As Part Of A Treatment For Lung Problems
Zemaira is a medication that is used to replace an enzyme in patients with lung problems caused by low levels of alpha-1 antitrypsin (ATA). It is not a cure.
Can Prescription Hope Help Me Obtain My Other Medications?
According to the Centers for Disease Control, nearly one in five Americans regularly takes three prescription medications. Our advocates work on your behalf to obtain all your medications for the set price of $50.00 per month for each medication. Prescription Hope works directly with over 180 U.S.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
What is the original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). (Part A and Part B) or a.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
How much does Medicare pay for Part B?
For Part B-covered services, you usually pay 20% of the Medicare-approved amount after you meet your deductible. This is called your coinsurance. You pay a premium (monthly payment) for Part B. If you choose to join a Medicare drug plan (Part D), you’ll pay that premium separately.
Does Medicare Advantage cover prescriptions?
Most Medicare Advantage Plans offer prescription drug coverage. . Some people need to get additional coverage , like Medicare drug coverage or Medicare Supplement Insurance (Medigap). Use this information to help you compare your coverage options and decide what coverage is right for you.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
When will Medicare start paying for insulin?
Insulin savings through the Part D Senior Savings Model. Starting January 1, 2021, you may be able to get Medicare drug coverage that offers broad access to many types of insulin for no more than $35 for a month's supply.
How much does Medicare pay for insulin?
Your costs in Original Medicare. You pay 100% for insulin (unless used with an insulin pump, then you pay 20% of the. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
What is a deductible for Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. applies). You pay 100% for syringes and needles, unless you have Part D.
How long does Medicare coverage last?
This special period lasts for eight months after the first month you go without your employer’s health insurance. Many people avoid having a coverage gap by signing up for Medicare the month before your employer’s health insurance coverage ends.
What is a small group health plan?
Since your employer has less than 20 employees, Medicare calls this employer health insurance coverage a small group health plan. If your employer’s insurance covers more than 20 employees, Medicare will pay secondary and call your work-related coverage a Group Health Plan (GHP).
Does Medicare cover health insurance?
Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance coverage in different ways. If your company has 20 employees or less and you’re over 65, Medicare will pay primary. Since your employer has less than 20 employees, Medicare calls this employer health insurance coverage ...
Does Cobra pay for primary?
The only exception to this rule is if you have End-Stage Renal Disease and COBRA will pay primary. Your COBRA coverage typically ends once you enroll in Medicare. However, you could potentially get an extension of the COBRA if Medicare doesn’t cover everything the COBRA plan does like dental or vision insurance.
Does Medicare pay second to employer?
Your health insurance through your employer will pay second and cover either some or all of the costs left over. If Medicare pays secondary to your insurance through your employer, your employer’s insurance pays first. Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance ...