a characteristic of Medicare enrollment Eligible individuals are automatically enrolled, or they apply for coverage A Medicare benefit period is defined as beginning the first day of hospitalization and ending when the patient has been out of the hospital for 60 consecutive days
Who is automatically enrolled in Medicare?
Those who have worked in the Social Security system at least 10 years, are a US citizen or legal resident and have lived in the US at least 5 years are automatically enrolled in Medicare Part A and Part B at age 65
Which providers cannot enroll in Medicare?
Version 1.0 – July 30, 2015 MEDICARE PROVIDER ENROLLMENT ELIGIBILITY REFERENCE TABLE. 1. Physicians and Non Physicians Permitted to Enroll in Medicare Non Physicians NOT Permitted to Enroll in Medicare
Will I be automatically enrolled in Medicare?
Enrollment will happen automatically. For example, if you took retirement benefits at 62 instead of full retirement age, you’ll be enrolled in Medicare three months before your 65th birthday. You could also be automatically enrolled if you’ve been receiving Social Security Disability Insurance (SSDI) for 24 months.
What to do during Medicare open enrollment?
• Screening for income guidelines, being mindful of programs that might help you pay for your Medicare, and helping with fraud and general complaints. • Talking to Medicare on your behalf. • Providing enrollment help when you first come onto Medicare and annually during open enrollment. • Making referrals to other agencies and programs.

What are the characteristics of Medicare?
Medicare provides coverage of a comprehensive set of vital medical services, including care in hospitals and other settings, physician services, diagnostic tests, preventive services, and an outpatient prescription drug benefit.
What are the eligibility requirements for Medicare quizlet?
Terms in this set (59) anyone reaching age 65 and qualifying for social security benefits is automatically enrolled into the Medicare part A system and offered Medicare Part B regardless of financial need.
What is the Medicare program quizlet?
Medicare is a social insurance program administered by the United States government, providing health insurance coverage to people who are aged 65 and over, or who meet other special criteria.
What is Medicare and why is it important?
Medicare provides health insurance coverage to individuals who are age 65 and over, under age 65 with certain disabilities, and individuals of all ages with ESRD. Medicaid provides medical benefits to groups of low-income people, some who may have no medical insurance or inadequate medical insurance.
Which of the following is not true about Medicare quizlet?
Which of the following is not true about Medicare? Medicare is not the program that provides benefits for low income people _ that is Medicaid. The correct answer is: It provides coverage for people with limited incomes.
Which statement is true about a member of a Medicare Advantage plan who wants to enroll in a Medicare supplement insurance plan?
Which statement is true about members of a Medicare Advantage (MA) Plan who want to enroll in a Medicare Supplement Insurance Plan? The consumer must be in a valid MA election or disenrollment period.
What is Medicare program?
Medicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
What is Medicare quizlet Everfi?
Medicare is federal health insurance for people older than 65. What is a want. Something you don't need but you would like it.
What is the primary purpose of Medicare quizlet?
The primary purpose of Medicare as enacted in 1965 was to: Provide health insurance for older Americans.
What are examples of Medicare?
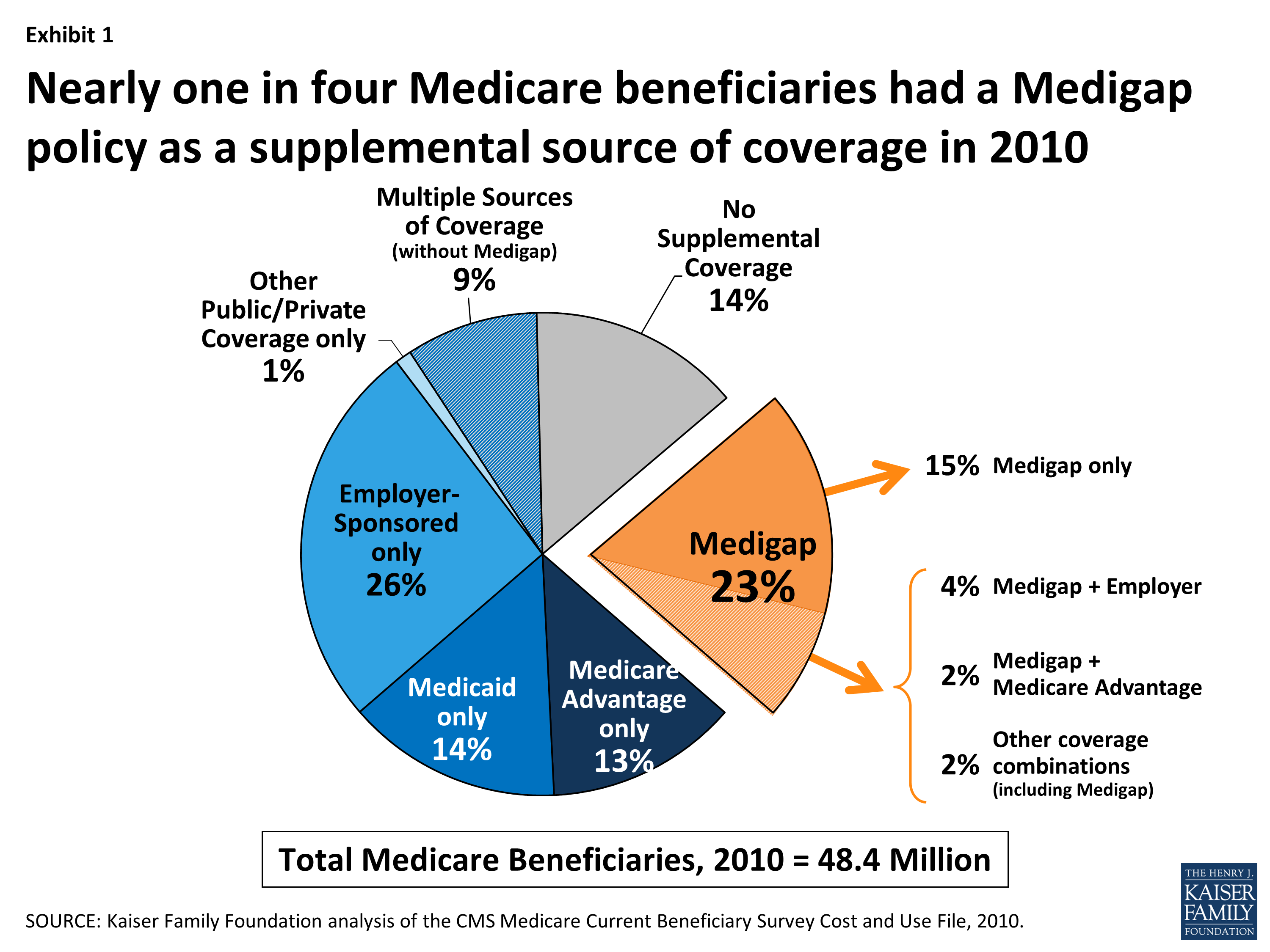
Below are some examples of the different kinds of Medicare and Medigap coverage a person may get and what costs could be when used....Original Medicare (Parts A & B)Stand-alone Medicare Part D prescription drug plan.Medicare supplement insurance plan (Plan G)
What are the four parts of Medicare?
Thanks, your Guide will be delivered to the email provided shortly.Medicare Part A: Hospital Insurance.Medicare Part B: Medical Insurance.Medicare Part C: Medicare Advantage Plans.Medicare Part D: prescription drug coverage.
What is Medicare for people 65 and older?
Medicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. at the start of each year, and you usually pay 20% of the cost of the Medicare-approved service, called coinsurance.
Do you pay Medicare premiums if you are working?
You usually don't pay a monthly premium for Part A if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A."
Does Medicare Advantage cover vision?
Most plans offer extra benefits that Original Medicare doesn’t cover — like vision, hearing, dental, and more. Medicare Advantage Plans have yearly contracts with Medicare and must follow Medicare’s coverage rules. The plan must notify you about any changes before the start of the next enrollment year.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like copayments, coinsurance, and deductibles.
Does Medicare cover prescription drugs?
Medicare drug coverage helps pay for prescription drugs you need. To get Medicare drug coverage, you must join a Medicare-approved plan that offers drug coverage (this includes Medicare drug plans and Medicare Advantage Plans with drug coverage).
What is Medicare and Medicaid?
Medicare is administered by the Centers for Medicare & Medicaid Services and is an entitlement program similar to Social Security. This means that most U.S. citizens earn Medicare health insurance eligibility by paying taxes for a set period of time.
When will seniors be automatically enrolled in Medicare?
Fact 4: Some seniors are enrolled in Part A automatically. Some seniors will be enrolled in Medicare Part A automatically around their 65th birthday. If you are not automatically enrolled, you can enroll in Medicare Parts A and B during certain enrollment periods.
What is Medicare Part D?
Medicare Part D is optional prescription drug coverage that is also provided by private insurance companies. Both Part C and Part D are regulated by the federal government. You can compare Part D plans available where you live and enroll in a Medicare prescription drug plan online when you visit MyRxPlans.com.
How many people are covered by Medicare?
Fact 2: Medicare covers more than 61 million people. Medicare had over 61 million enrollees in the United States in November 2019, according to statistics from the Centers for Medicare & Medicaid Services (CMS). 1.
When is Medicare open enrollment?
The Medicare Open Enrollment Period for Medicare Advantage plans and Medicare Part D prescription drug plans runs from October 15 to December 7. During this time, you can make several changes such as joining a Medicare Advantage plan or a Medicare prescription drug plan.
Is Medicare for seniors?
Fact 1: Medicare is for seniors and the disabled. Medicare is a federally-funded health insurance program for people age 65 or older and some younger people who have qualifying disabilities or who have end-stage renal disease (ESRD).
Do you have to pay Medicare premiums?
If you or your spouse paid Medicare taxes for 10 or more years while working, you are eligible for premium-free Medicare Part A coverage. If you are under 65, you may also qualify for premium-free Part A coverage. All Medicare beneficiaries may still be responsible ...
Background
Medicare Part C (Medicare Advantage) enrollment has grown more rapidly than fee-for-service Medicare Enrollment in the last decade, raising questions about changes in the characteristics of different enrollee populations for Medicare Part A only, Medicare Part A & B and Medicare Part C.
Method
We used 2011-2019 Medicare Eligibility Enrollment files to identify Medicare beneficiaries and classify them into three enrollment types: Medicare Part A only, Medicare Part A and B, and Medicare Part C. We analyzed two age groups: those younger than 65 and those age 65 and older.
Findings
Figure 1. For older and younger Medicare beneficiaries, enrollment in Medicare Parts A & B (lower gold band), Part A only (middle gold band) and Part C (upper blue band), 2011-2019.
Next Step
Over the last decade, Medicare Part C enrollment far outpaced that in Part A and Part B Medicare. This is partially because more Americans aged 65 and older are remaining employed and elimination of late Part B Enrollment Penalties may have encouraged such enrollment.
Explore with CareJourney
If you are interested in understanding how CareJourney analytics can help with your organization’s assessment of geographic variation, we want to hear from you. Current members can reach out to their CareJourney representative for more information.
When is the enrollment period for Medicare Part A?
Eligible individuals are automatically enrolled, or they apply for coverage. b. The general enrollment period is between January 1 and December 31. c. Those who enroll in Medicare Part A must also enroll in Medicare Part B. d. Individuals who qualify for SSA benefits must "buy in" to Medicare Part A.
What is Medicare benefit period?
A Medicare benefit period is defined as beginning the first day of hospitalization and ending when. a. the patient has been admitted to a skilled nursing facility.
How long is the Medicare enrollment period?
Medicare. The initial enrollment period (IEP) for Medicare Part A and Part B is: seven months. A federally mandated program that requires states to cover just the Medicare Part B premium for a person whose income is slightly over the poverty level is the: specified low-income Medicare beneficiary.
What is Medicare benefit period?
A Medicare benefit period is defined as beginning the first day of hospitalization and ending when: Click card to see definition 👆. Tap card to see definition 👆. the patient has been out of the hospital for 60 consecutive days. Click again to see term 👆.
When should a provider generate an ABN?
The supplier or provider should generate an ABN if he or she believes that a claim for the services is likely to receive a. medical necessity denial. A physician or practitioner with a Medicare private contract agrees not to bill for any service or supplies provided to any Medicare beneficiary for at least: two years.
