Which service is not covered by Part B Medicare?
But there are still some services that Part B does not pay for. If you're enrolled in the original Medicare program, these gaps in coverage include: Routine services for vision, hearing and dental care — for example, checkups, eyeglasses, hearing aids, dental extractions and dentures.
What is Medicare Part B all about?
Medicare Part B helps cover medically-necessary services like doctors' services and tests, outpatient care, home health services, durable medical equipment, and other medical services. Part B also covers some preventive services. Look at your Medicare card to find out if you have Part B.
Which of the following is not true about Medicare?
Which of the following is not true about Medicare? Medicare is not the program that provides benefits for low income people _ that is Medicaid. The correct answer is: It provides coverage for people with limited incomes.
What main things are covered under Medicare Part B?
Part B covers things like:Clinical research.Ambulance services.Durable medical equipment (DME)Mental health. Inpatient. Outpatient. Partial hospitalization.Limited outpatient prescription drugs.
What is Medicare Part B also known as quizlet?
Medicare Part B is also called. Supplemental Medical Insurance. Durable Medical Equipment is covered by. Medicare Part B.
Which of the following is covered by Medicare Part B quizlet?
Part B helps cover medically-necessary services like doctors' services, outpatient care, durable medical equipment, home health services, and other medical services.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
What is Medicare Part A and Part B?
Part A (Hospital Insurance): Helps cover inpatient care in hospitals, skilled nursing facility care, hospice care, and home health care. Part B (Medical Insurance): Helps cover: Services from doctors and other health care providers. Outpatient care.
Which of the following statements about Original Medicare is false?
Answer: False. Original Medicare is different from Medicare Advantage plans. Under Original Medicare, the government pays directly for the health care services you receive. On the other hand, Medicare Advantage plans are offered by private insurance companies approved by Medicare to provide Medicare coverage.
Does Medicare Part B have a deductible?
Medicare Part B Premium and Deductible The standard monthly premium for Medicare Part B enrollees will be $170.10 for 2022, an increase of $21.60 from $148.50 in 2021. The annual deductible for all Medicare Part B beneficiaries is $233 in 2022, an increase of $30 from the annual deductible of $203 in 2021.
Does Medicare Part B pay for prescriptions?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers a limited number of outpatient prescription drugs under certain conditions. A part of a hospital where you get outpatient services, like an emergency department, observation unit, surgery center, or pain clinic.
Does Medicare Part B cover 100 percent?
Generally speaking, Medicare reimbursement under Part B is 80% of allowable charges for a covered service after you meet your Part B deductible. Unlike Part A, you pay your Part B deductible just once each calendar year. After that, you generally pay 20% of the Medicare-approved amount for your care.
Understanding What Medicare Part B Offers
First, let’s take a look at what Medicare Part B actually covers. Medicare Part B covers medical treatments and services under two classifications:...
Medicare Part B Enrollment Options and Penalties
Medicare Part B is optional, but in some ways, it can feel mandatory, because there are penalties associated with delayed enrollment. As discussed...
The Cost of Medicare Part B
Unlike Medicare Part A, Medicare Part B requires a premium. For the most part, the premium for Medicare Part B is $134 per month. You also pay $204...
Medicare Part B Financial Assistance
Because Medicare Part B requires a monthly payment (known as a premium) for its services, some people may find it difficult to pay for the monthly...
Medicare Part B Special Circumstances and Updates
Some people don’t need Medicare Part B coverage right away, because they have medical insurance through their employers or meet other special condi...
Benefits of Medicare Part B
Medicare Part B covers a variety of routine healthcare visits and treatments. If you can afford the premiums, then you may want to take advantage o...
What services does Medicare cover?
Dentures. Cosmetic surgery. Acupuncture. Hearing aids and exams for fitting them. Routine foot care. Find out if Medicare covers a test, item, or service you need. If you need services Medicare doesn't cover, you'll have to pay for them yourself unless you have other insurance or a Medicare health plan that covers them.
Does Medicare cover everything?
Medicare doesn't cover everything. Some of the items and services Medicare doesn't cover include: Long-Term Care. Services that include medical and non-medical care provided to people who are unable to perform basic activities of daily living, like dressing or bathing.
Does Medicare pay for long term care?
Medicare and most health insurance plans don’t pay for long-term care. (also called. custodial care. Non-skilled personal care, like help with activities of daily living like bathing, dressing, eating, getting in or out of a bed or chair, moving around, and using the bathroom.
What is Part B?
Part B covers 2 types of services. Medically necessary services: Services or supplies that are needed to diagnose or treat your medical condition and that meet accepted standards of medical practice. Preventive services : Health care to prevent illness (like the flu) or detect it at an early stage, when treatment is most likely to work best.
What are the factors that determine Medicare coverage?
Medicare coverage is based on 3 main factors 1 Federal and state laws. 2 National coverage decisions made by Medicare about whether something is covered. 3 Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
When do you have to be on Medicare before you can get Medicare?
Individuals already receiving Social Security or RRB benefits at least 4 months before being eligible for Medicare and residing in the United States (except residents of Puerto Rico) are automatically enrolled in both premium-free Part A and Part B.
How long does it take to get Medicare if you are 65?
For someone under age 65 who becomes entitled to Medicare based on disability, entitlement begins with the 25 th month of disability benefit entitlement.
How long do you have to be on Medicare if you are disabled?
Disabled individuals are automatically enrolled in Medicare Part A and Part B after they have received disability benefits from Social Security for 24 months. NOTE: In most cases, if someone does not enroll in Part B or premium Part A when first eligible, they will have to pay a late enrollment penalty.
What is the income related monthly adjustment amount for Medicare?
Individuals with income greater than $85,000 and married couples with income greater than $170,000 must pay a higher premium for Part B and an extra amount for Part D coverage in addition to their Part D plan premium. This additional amount is called income-related monthly adjustment amount. Less than 5 percent of people with Medicare are affected, so most people will not pay a higher premium.
What happens if you don't enroll in Part A?
If an individual did not enroll in premium Part A when first eligible, they may have to pay a higher monthly premium if they decide to enroll later. The monthly premium for Part A may increase up to 10%. The individual will have to pay the higher premium for twice the number of years the individual could have had Part A, but did not sign up.
How long does Medicare take to pay for disability?
A person who is entitled to monthly Social Security or Railroad Retirement Board (RRB) benefits on the basis of disability is automatically entitled to Part A after receiving disability benefits for 24 months.
Why does Part A end?
There are special rules for when premium-free Part A ends for people with ESRD. Premium Part A and Part B coverage can be voluntarily terminated because premium payments are required. Premium Part A and Part B coverage ends due to: Voluntary disenrollment request (coverage ends prospectively); Failure to pay premiums;
What is Medicare Part A?
Tap card to see definition 👆. Coverage of Medicare Part A-eligible hospital expenses to the extent not covered by Medicare from the 61st through the 90th day in any Medicare benefit period. Explanation. The benefits in Plan A, which is known as the core plan, must be contained in all other plans sold.
Which Medicare supplement plan has the least coverage?
Explanation. In the 12 standardized Medicare supplement plans, Plan A provides the least coverage and is referred to as the core plan. Plan J has the most comprehensive coverage. Plans K and L provide basic benefits similar to plans A through J, but cost sharing is at different levels.
What happens after Tom pays the deductible?
After Tom pays the deductible, Medicare Part A will pay 100% of all covered charges. Explanation. Medicare Part A pays 100% of covered services for the first 60 days of hospitalization after the deductible is paid.
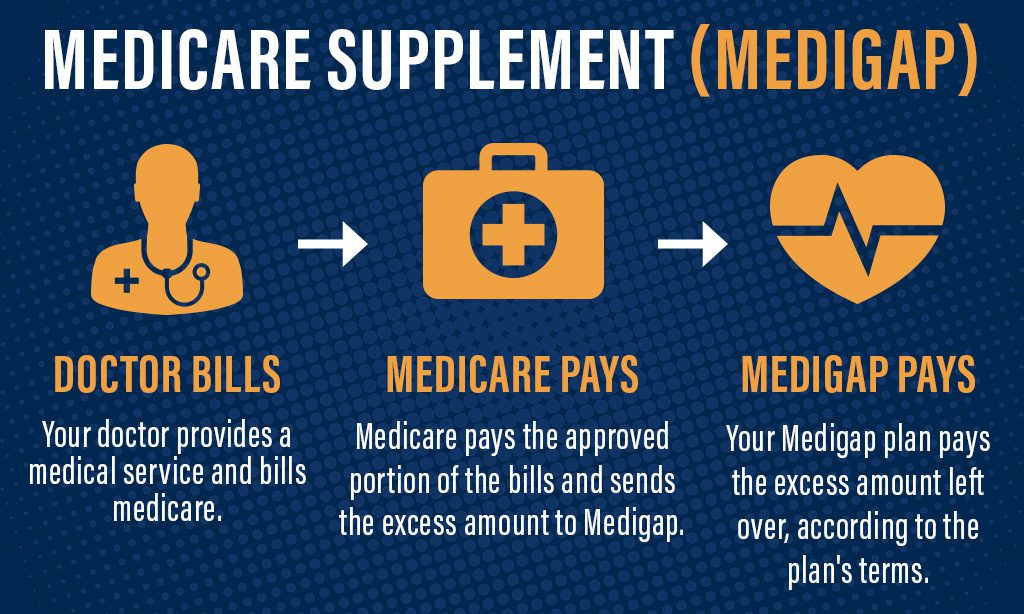
What is Medicare Supplement Insurance?
Medicare supplement insurance fills the gaps in coverage left by Medicare, which provides hospital and medical expense benefits for persons aged 65 and older. All Medicare supplement policies must cover 100% of the Part A hospital coinsurance amount for each day used from.
How long does Medicare cover skilled nursing?
Medicare will cover treatment in a skilled nursing facility in full for the first 20 days. From the 21st to the 100th day, the patient must pay a daily co-payment. There are no Medicare benefits provided for treatment in a skilled nursing facility beyond 100 days. Medicare Part A covers.
What is Medicaid in the US?
Medicaid is a federal and state program designed to help provide needy persons, regardless of age, with medical coverage. A contract designed primarily to supplement reimbursement under Medicare for hospital, medical or surgical expenses is known as. A) an alternative benefits plan. B) a home health care plan.
What is the core plan of Medicare?
Among the core benefits is coverage of Medicare Part A-eligible expenses for hospitalization, to the extent not covered by Medicare, from the 61st day through the 90th day in any Medicare benefit period.
How much does Medicare pay after deductible?
Medicare pays the remaining 80% of covered Medicare Part B charges after: The annual deductible is met. Medicare pays the remaining 80% of covered charges after the deductible is met.
What is Medicare approved charge?
The Medicare approved charge/amount is the dollar amount that Medicare considers to be the reasonable charge for a particular medical service. Payment of each medical service covered by Medicare is based on its Medicare approved charge. Click again to see term 👆. Tap again to see term 👆.
Is Medicare Part A voluntary?
Medicare Part A is automatically available to persons who have turned 65 and have applied for Social Security benefits. Medicare Part B is voluntary and may be elected or rejected as the recipient wishes.