Mostly, Medicare is primary. The primary insurer is the one that pays the claim first, whereas the secondary insurer pays second. With a Medigap policy, the supplement is secondary. Medicare pays claims first, and then Medigap pays. But, depending on the other policy, you have Medicare could be a secondary payer.
Full Answer
Is Medicare primary or secondary?
Is Medicare Primary or Secondary? - Who Pays First - MedicareFAQ Medicare is always primary if it’s your only form of coverage. When you introduce another form of coverage into the picture, there’s predetermined coordination of benefits.
What is a Medicare replacement plan?
Updated on March 19, 2021 If you’ve heard of a Medicare replacement plan, it’s the same as an Advantage plan. Advantage plans are also known as replacement plans because, in a way, they replace Original Medicare. If you’re thinking about signing up for an Advantage plan, we’re here to tell you everything you need to know.
What is the difference between Original Medicare and replacement Medicare?
Replacement plans are not identical to original Medicare, and someone with a replacement plan might have less flexibility in choosing healthcare providers than they do with original Medicare. However, replacement plans often include benefits that original Medicare does not offer, such as coverage of dental and vision care.
What are Medicare Part C and other Medicare replacements?
Replacement plans, Advantage, or Part C, plans stand-in for your Medicare for each year you’ve enrolled. They don’t act as a permanent replacement, and you can always return to Medicare during the Medicare Advantage Open Enrollment Period or Annual Enrollment Period.

Is Medicare replacement always primary?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
How do you determine which insurance is primary and which is secondary?
The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" to pay. The insurance that pays first is called the primary payer. The primary payer pays up to the limits of its coverage. The insurance that pays second is called the secondary payer.
Is Medicare replacement the same as Medicare?
A Medicare Advantage plan serves as a replacement for original Medicare. The costs, benefits, and coverage rules for Medicare Advantage may be different than those of original Medicare. They may also vary among plans.
Is Medicare primary or secondary payer?
The secondary payer (which may be Medicare) may not pay all the remaining costs. If your group health plan or retiree coverage is the secondary payer, you may need to enroll in Medicare Part B before they'll pay.
When two insurance which one is primary?
If you have two plans, your primary insurance is your main insurance. Except for company retirees on Medicare, the health insurance you receive through your employer is typically considered your primary health insurance plan.
How do I determine which insurance is primary?
Primary insurance is a health insurance plan that covers a person as an employee, subscriber, or member. Primary insurance is billed first when you receive health care. For example, health insurance you receive through your employer is typically your primary insurance.
Do Medicare replacement plans follow Medicare guidelines?
Medicare Advantage Plans Must Follow CMS Guidelines In the United States, according to federal law, Part C providers must provide their beneficiaries with all services and supplies that Original Medicare Parts A and B cover. They must also provide any additional benefits proclaimed in their Part C policy.
Can you switch back and forth between Medicare and Medicare Advantage?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
Does Medicare Advantage replace Medicare Part B?
Medicare Advantage doesn't replace Original Medicare Part A and Part B coverage; it simply delivers these benefits through an alternative channel: private insurance companies. Medicare Advantage plans are offered by private insurance companies that contract with Medicare.
Does Medicare automatically forward claims to secondary insurance?
If a Medicare member has secondary insurance coverage through one of our plans (such as the Federal Employee Program, Medex, a group policy, or coverage through a vendor), Medicare generally forwards claims to us for processing.
What does Medicare pay as secondary payer?
As secondary payer, Medicare pays the lowest of the following amounts: (1) Excess of actual charge minus the primary payment: $175−120 = $55. (2) Amount Medicare would pay if the services were not covered by a primary payer: . 80 × $125 = $100.
How do you make Medicare primary?
Making Medicare Primary. If you're in a situation where you have Medicare and some other health coverage, you can make Medicare primary by dropping the other coverage. Short of this, though, there's no action you can take to change Medicare from secondary to primary payer.
What is the difference between Medicare and Medicaid?
Eligible for Medicare. Medicare. Medicaid ( payer of last resort) 1 Liability insurance only pays on liability-related medical claims. 2 VA benefits and Medicare do not work together. Medicare does not pay for any care provided at a VA facility, and VA benefits typically do not work outside VA facilities.
Is Medicare a secondary insurance?
When you have Medicare and another type of insurance, Medicare is either your primary or secondary insurer. Use the table below to learn how Medicare coordinates with other insurances. Go Back. Type of Insurance. Conditions.
What is Medicare replacement plan?
What is a Medicare Replacement Plan. If you’ve heard of a Medicare replacement plan, it’s the same as an Advantage plan. Advantage plans are also known as replacement plans because, in a way, they replace Original Medicare. If you’re thinking about signing up for an Advantage plan, we’re here to tell you everything you need to know.
Why are Advantage Plans also known as Replacement Plans?
Advantage plans are also known as replacement plans because, in a way, they replace Original Medicare. If you’re thinking about signing up for an Advantage plan, we’re here to tell you everything you need to know.
Can you return to Medicare Advantage during Open Enrollment Period?
Replacement plans, Advantage, or Part C, plans stand-in for your Medicare for each year you’ve enrolled. They don’t act as a permanent replacement, and you can always return to Medicare during the Medicare Advantage Open Enrollment Period or Annual Enrollment Period. The way these plans work is by providing benefits through a private insurance ...
Can an Advantage Plan replace Medicare?
Again, an Advantage plan doesn’t permanently replace Medicare. However, it acts as your primary coverage. Medicare pays private insurance companies offering Advantage plans to handle beneficiary claims and benefits. The Advantage plan must offer the same benefits as Parts A and B.
Can you drop a Medicare Advantage plan?
Can a Medicare Advantage plan drop you? If you don’t pay your premium for your plan or Part B, your Advantage plan can drop you. Likewise, if you move outside the service area, they can drop you.
What is Medicare replacement plan?
Medicare Replacement plans combine the core parts of Medicare and create a private healthcare plan. These plans often have other benefits such as dental, vision, and hearing. When you enroll in a Medicare Advantage plan, you are formally telling Medicare that until December 31 st, you are choosing to get your Part A and Part B benefits through ...
When was Medicare Advantage created?
The Medicare Advantage program was created in the late 1990s to give beneficiaries another option besides Original Medicare and a Medigap plan. Some people cannot afford Medigap plan premiums so these Medicare Advantage “replacement plans” give them an alternative – a way to get their benefits from a private plan instead of Medicare.
What are the extras of Medicare Advantage?
These plans can offer extra benefits for something that Medicare doesn’t cover, like routine dental, vision, and hearing services. Some plans may even offer free fitness memberships.
Can you change your Medicare Advantage plan from year to year?
The list of covered medications, called a drug formulary, can be changed from year to year as well. If you are unhappy with any of the plan’s changes for the upcoming year, you can make a change to a different Medicare Advantage plan offered in your county during the fall Annual Election Period.
Can you use Medicare Advantage instead of Medicare Replacement?
However, Medicare prefers that you use the term Medicare Advantage or Part C plan (instead of Medicare replacement plan) because you are never permanently replacing your Original Medicare benefits. You can always return to them during the next election period.
Does Medicare replace Medicare?
Does Medicare Advantage replace Medicare? The answer is yes and no. “Medicare replacement plans” is a phrase commonly used by Medicare beneficiaries and medical providers when referring to Medicare Advantage plans. Advantage plans are private insurance policies that pay instead of Medicare for the calendar year that you enroll in them. ...
Does Medicare change benefits?
Benefits Change Annually. Something else to be aware of about Medicare Replacement plans is that the benefits change from year to year. When you enroll in a plan, the premiums and cost-sharing that you pay are for that one year only. In September, the plan will mail you an annual notice of change letter. This will go over all the things that are ...
What is Medicare replacement plan?
A Medicare replacement plan provides a way for people to get their original Medicare benefits and, usually, prescription drug coverage in one place. Some people refer to these replacement plans as Medicare Advantage plans or Medicare Part C. Replacement plans are not identical to original Medicare, and someone with a replacement plan might have ...
What is Medicare Part A and Part B?
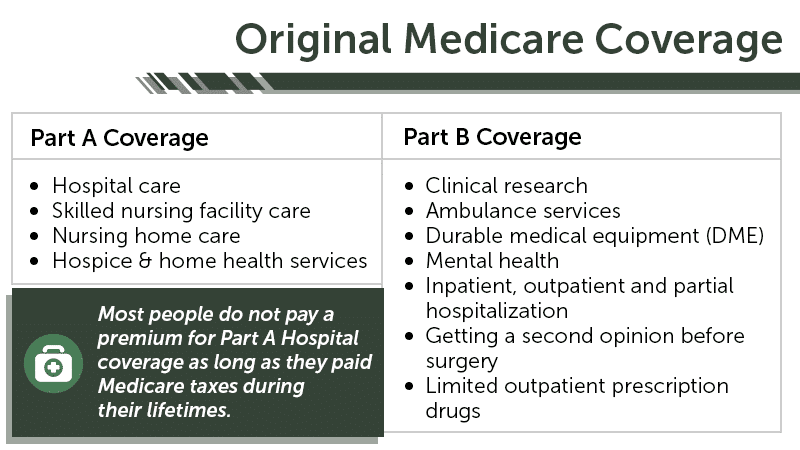
Medicare replacement plans bundle together Medicare Part A, which is inpatient hospital insurance, and Medicare Part B, which is outpatient medical insurance. The plans usually also provide the prescription drug benefits of Medicare Part D. Medicare Advantage plans are available to those who are eligible for Medicare and live in the region ...
How long does it take to sign up for Medicare Advantage?
It is a 7-month period that begins 3 months before a person reaches the age of 65 years.
How much is Medicare Part B 2021?
Some Medicare Advantage plans have a monthly premium, which a person pays along with their Medicare Part B premium. The standard Part B premium is $148.50 per month in 2021.
How many Medicare Advantage plans will be available in 2021?
In 2021, private insurance companies will offer more than 4,800 Medicare Advantage plans, up from about 2,700 plans in 2017, according to the Centers for Medicare & Medicaid Services (CMS). A person can use Medicare’s plan comparison tool to look for plans in their area.
How many people have Medicare Advantage 2020?
The policies cover all part A and B services, according to Medicare.gov. In 2020, the Kaiser Family Foundation (KFF) reported that approximately 36% of people with Medicare had a Medicare Advantage plan. They also noted that this percentage has been growing over the last 15 years.
What is an HMO plan?
HMO plans. When a person has an HMO plan, they must usually visit healthcare providers within the plan’s network. This requirement is not in place in original Medicare, which allows an individual to see any provider in the United States that accepts Medicare. Someone with an HMO plan must typically choose a primary care provider ...
What does primary and secondary payer mean?
Each type of coverage you have is called a “payer.” When you have more than one payer, there are rules to decide who pays first, called the coordination of benefits. The “primary payer” pays what it owes on your bills first and sends the remaining amount to the second or “secondary payer.” There may also be a third payer in some cases. 1
When is Medicare primary or secondary?
A number of things can affect when Medicare pays first. The following chart explains some common scenarios. 3 For information on several other scenarios, check out how Medicare works with other insurance , opens new window .
How does Medicare know if I have other coverage?
Medicare doesn’t automatically know if you have other coverage. But your insurers must report to Medicare when they’re the primary payer on your medical claims.
Where to get more details
If you have additional questions about who pays your Medicare bills first, contact your insurance provider or call Medicare’s Benefits Coordination & Recovery Center (BCRC) at 855-798-2627 (TTY: 855-797-2627).
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What is Medicare Part A and Part B?
Medicare Part A covers hospital insurance, and Part B covers medical insurance. By law, Medicare Advantage plans (which are sold by private insurance companies) are required to provide the same benefits as Original Medicare. When enrolled in Medicare Advantage, you will receive your Part A and Part B benefits through your Medicare Advantage plan ...
What benefits do you get with Medicare Advantage?
When enrolled in Medicare Advantage, you will receive your Part A and Part B benefits through your Medicare Advantage plan except for hospice care, which you will continue to receive through Part A.
Does Medicare replace Original Medicare?
The answer is that in a sense, yes , Medicare Advantage does replace Original Medicare. But there’s much more to understanding the relationship between Medicare and Medicare Advantage. This guide will help you learn more about Medicare Advantage plans so that you can better decide which type of Medicare coverage is right for your needs.
Does Medicare Advantage cover prescriptions?
Many Medicare Advantage plans include prescription drug coverage, though benefits and plan availability vary based on your location. Some plans may also offer benefits not found in Original Medicare, such as coverage for dental, hearing, vision, and other benefits.