
Coverage can be denied under a Medicare Advantage plan when:
- Plan rules are not followed, like failing to seek prior approval for a particular treatment if required
- Treatments provided were not deemed to be medically necessary
- An out-of-network provider was used when an in-network alternative was available
Full Answer
Can My Medicare Advantage plan be denied?
The services included in Medicare Advantage plans are usually covered without the risk of denial. There are also specific circumstances in which denial is explicitly prohibited. Treatment under these Medicare plans can’t be denied if: Necessary care must be performed by an out-of-network provider when no in-network provider is available
What's the latest on Medicare Advantage denials?
The report from the inspector general's office of the Department of Health and Human Services is the latest red flag related to inappropriate denials by Medicare Advantage plans, which are run by private health care insurers.
Are Medicare Advantage plans delaying or preventing care?
The industry’s main trade group claims people choose Medicare Advantage because “it delivers better services, better access to care and better value.” But federal investigators say there is troubling evidence that plans are delaying or even preventing Medicare beneficiaries from getting medically necessary care.
How many Medicare claims are denied due to prior authorization?
Based on its finding that about 13 percent of the requests denied should have been covered under Medicare, the investigators estimated as many as 85,000 beneficiary requests for prior authorization of medical care were potentially improperly denied in 2019. Advantage plans also refused to pay legitimate claims, according to the report.
Do Medicare Advantage plans deny claims?
Advantage plans also refused to pay legitimate claims, according to the report. About 18 percent of payments were denied despite meeting Medicare coverage rules, an estimated 1.5 million payments for all of 2019. In some cases, plans ignored prior authorizations or other documentation necessary to support the payment.
Can Medicare Advantage plans deny coverage for pre existing conditions?
As with Original Medicare, Medicare Advantage plans can't charge you more for preexisting conditions. Because they are offered by private insurance companies, basic costs for Medicare Advantage plans will vary by plan. In addition, you can't be denied coverage based on preexisting conditions.
What is the most widely accepted Medicare Advantage plan?
AARP/UnitedHealthcare is the most popular Medicare Advantage provider with many enrollees valuing its combination of good ratings, affordable premiums and add-on benefits. For many people, AARP/UnitedHealthcare Medicare Advantage plans fall into the sweet spot for having good benefits at an affordable price.
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
What pre-existing conditions are not covered?
Health insurers can no longer charge more or deny coverage to you or your child because of a pre-existing health condition like asthma, diabetes, or cancer, as well as pregnancy. They cannot limit benefits for that condition either.
What are the top 3 Medicare Advantage plans?
The Best Medicare Advantage Provider by State Local plans can be high-quality and reasonably priced. Blue Cross Blue Shield, Humana and United Healthcare earn the highest rankings among the national carriers in many states.
Which is better PPO or HMO?
HMO plans typically have lower monthly premiums. You can also expect to pay less out of pocket. PPOs tend to have higher monthly premiums in exchange for the flexibility to use providers both in and out of network without a referral. Out-of-pocket medical costs can also run higher with a PPO plan.
What is the difference between AARP Medicare Complete and AARP Medicare Advantage?
Original Medicare covers inpatient hospital and skilled nursing services – Part A - and doctor visits, outpatient services and some preventative care – Part B. Medicare Advantage plans cover all the above (Part A and Part B), and most plans also cover prescription drugs (Part D).
What states have 5 star Medicare Advantage plans?
States where 5-star Medicare Advantage plans are available:Alabama.Arizona.California.Colorado.Florida.Georgia.Hawaii.Idaho.More items...•
Can you switch back to Medicare from Medicare Advantage?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
What's the big deal about Medicare Advantage plans?
Medicare Advantage Plans must offer emergency coverage outside of the plan's service area (but not outside the U.S.). Many Medicare Advantage Plans also offer extra benefits such as dental care, eyeglasses, or wellness programs. Most Medicare Advantage Plans include Medicare prescription drug coverage (Part D).
Can I switch from Medicare Advantage to Medigap?
Most Medicare Advantage Plans offer prescription drug coverage. , you may want to drop your Medigap policy. Your Medigap policy can't be used to pay your Medicare Advantage Plan copayments, deductibles, and premiums.
What is Medicare Advantage Plan?
Following the rules of a Medicare Advantage plan can help avert denials for coverage, including seeking preapproval for procedures, exhausting in-network options before seeking alternatives and reviewing medical necessity with a provider before moving forward.
Does Medicare Advantage cover travel?
Medicare Advantage plans are required to offer the same coverage as Medicare Parts A and B, and often provide expanded coverage options.
Does Medicare Advantage cover end stage renal disease?
However, Medicare Advantage plans don’t offer guaranteed coverage under all circumstances.
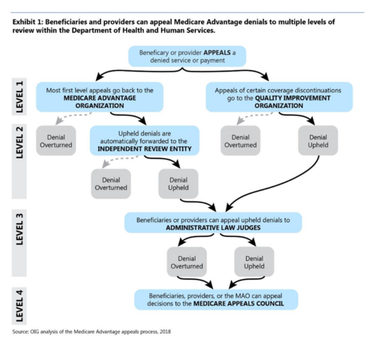
Can I appeal a Medicare Advantage claim?
Appealing a Denial of Coverage. If a Medicare Advantage insurance claim has been denied, it’s possible to file an appeal. The procedures for appeal can differ from one provider to another, so it’s vital to fully review the plan documentation before starting this process.
