EVIDENCE SURFACED RECENTLY THAT—when it comes to submitting genetic test claims to the Medicare program—the bonanza CPT code is 81408. The number of claims that Medicare paid for this code increased more than 25-fold in 24 months from 2017 and 2019, totaling $413 million, according to an analysis by Bruce Quinn, MD, PhD, a lab strategy and ...
Full Answer
Does Medicare cover genetic testing?
The health care professional performing the genetic test can explain any limitations known for a specific test and its common uses. In order for Medicare to cover genetic testing, certain requirements must be met.
What is the ICD 10 code for genetic testing?
Report code 81479 and gene test Nonspecific (NAT) in the claim narrative/remarks. It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted.
What is the First Coast billing and coding for genetic testing?
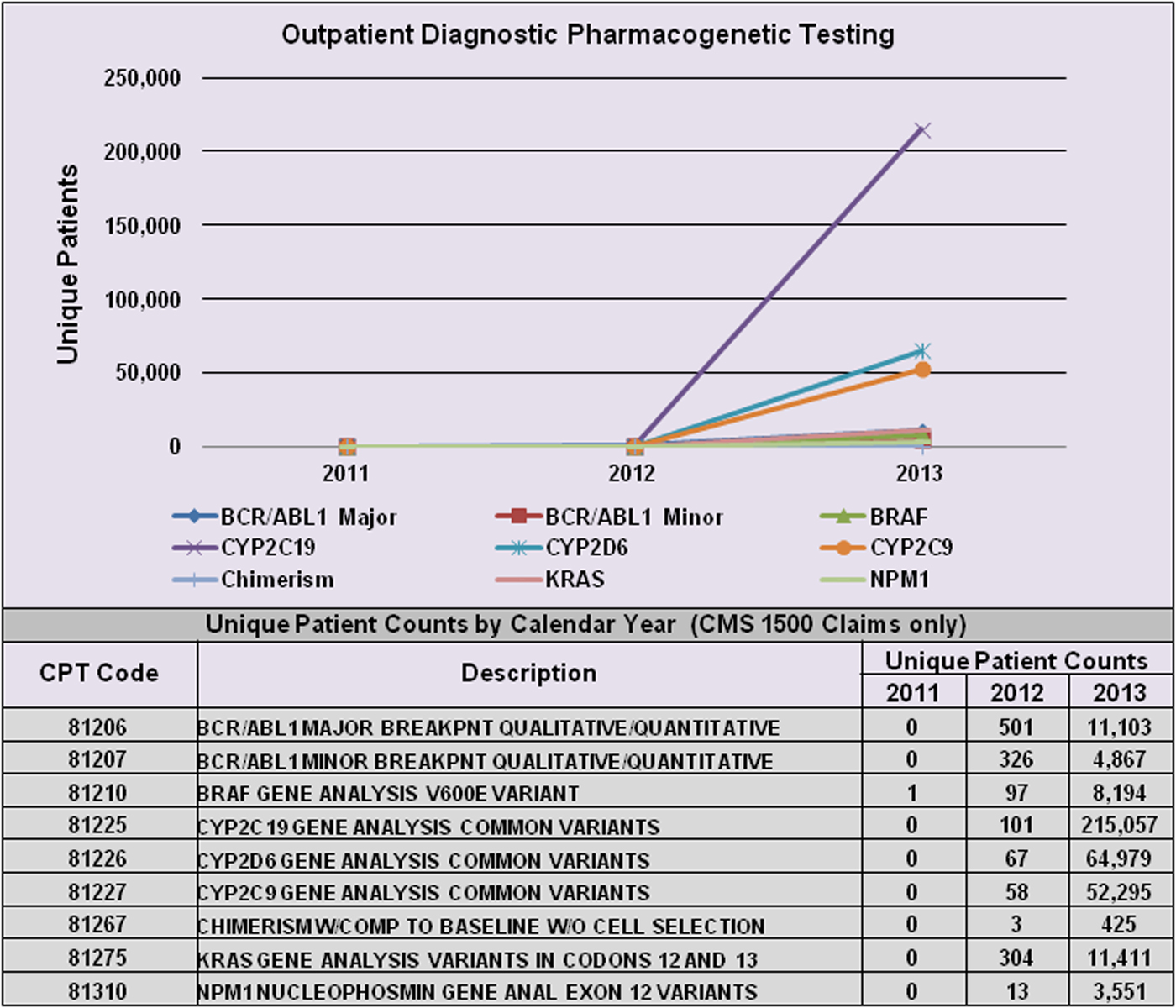
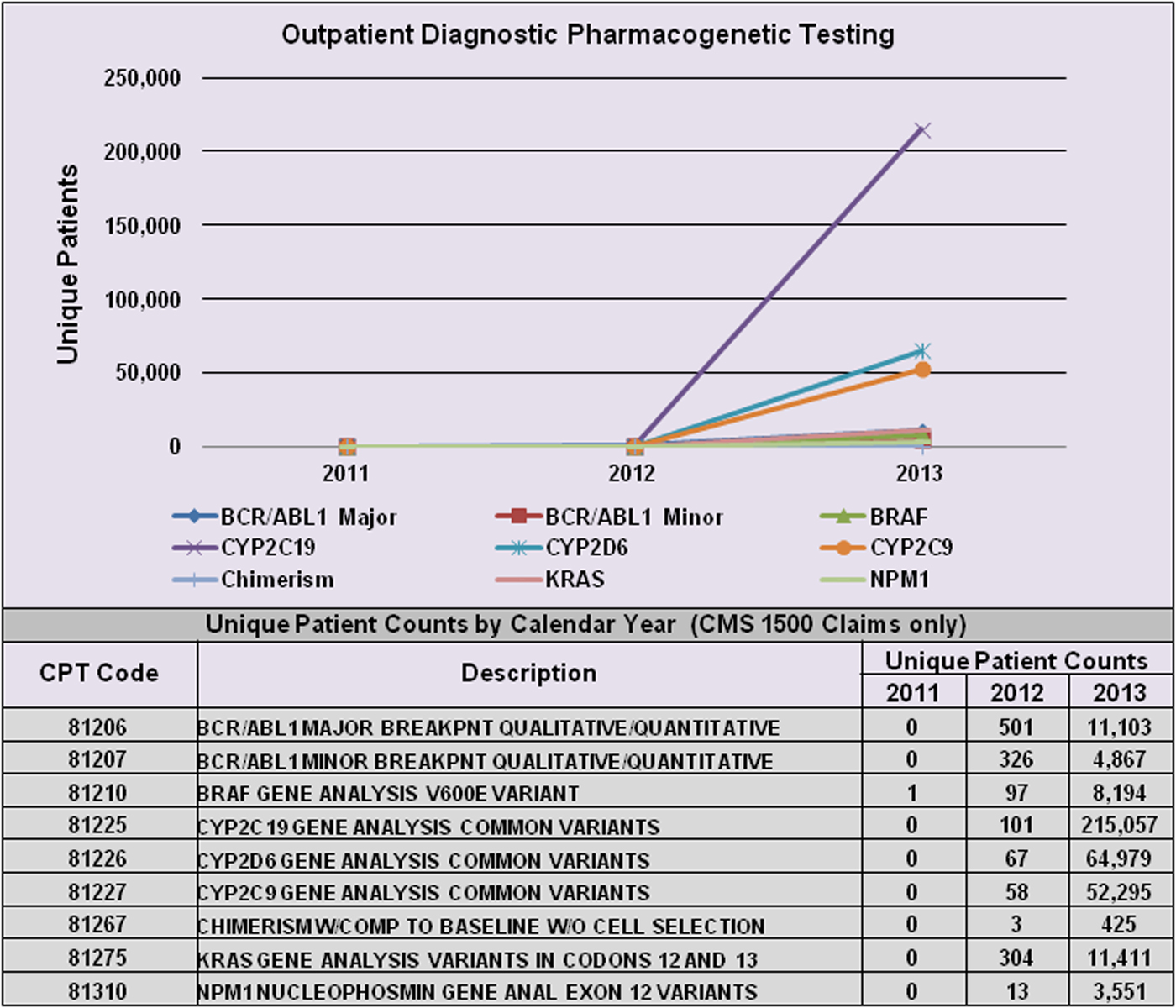
This First Coast Billing and Coding Article for Local Coverage Determination (LCD) L35698 CYP2C19, CYP2D6, CYP2C9, and VKORC1 Genetic Testing provides billing and coding guidance for frequency limitations as well as diagnosis limitations that support diagnosis to procedure code automated denials.
Are there any non-medical genetic tests?
Many non-medical genetic tests exist that are used to help determine identity or genealogy. These may be available as an over-the-counter product but are not used to serve as any diagnostic resource to determine medical conditions or treatment options.
What are the codes for genetic testing?
CPT Codes for Molecular Tests1Test NameCPT codes2ATP7B, Gene Sequencing814063Autism/Intellectual Disability (ID) Panel testing81229, 81244, 81331, 81302, 81321, 81304, 81323, 81406 X 7, 81405 X 24Beckwith-Wiedemann Syndrome Analysis814015BRCA1 and BRCA2 Sequencing (NGS)8116377 more rows
Does Medicare do genetic testing?
Medicare has limited coverage of genetic testing for an inherited genetic mutation. Medicare covers genetic testing for people with a cancer diagnosis who meet certain criteria; you must have a cancer diagnosis to qualify for coverage of genetic testing for an inherited mutation under Medicare.
How do you bill for genetic testing?
Common CPT Billing Codes for Genetic Risk Assessment99401 Preventive medicine counseling/risk factor reduction, 15 minutes.99402 Preventive medicine counseling/risk factor reduction, 30 minutes.99403 Preventive medicine counseling/risk factor reduction, 45 minutes.More items...
Is CPT 81420 genetic testing?
Sequencing-based non-invasive prenatal testing (NIPT) (CPT® codes 81420, 81507) to screen for fetal trisomy 13, 18 and 21 is considered medically necessary in a viable single or twin gestation pregnancy ≥ 10 weeks gestation.
Is CPT code 81479 genetic testing?
Unlisted Molecular Pathology - CPT Code 81479 However, when reporting CPT code 81479, the specific gene being tested must be entered in block 80 (Part A for the UBO4 claim), box 19 (Part B for a paper claim) or electronic equivalent of the claim.
Is CPT code 81206 genetic testing?
CPT® 81206, Under Genetic Analysis Procedures The Current Procedural Terminology (CPT®) code 81206 as maintained by American Medical Association, is a medical procedural code under the range - Genetic Analysis Procedures.
Is CPT 96040 covered by Medicare?
Genetic counseling billed under CPT 96040 is non-covered by Medicare and most other insurances, yet we continue to charge and bill. Please validate genetic counseling is non-covered by our managed care payers.
Does Medicare reimburse for 96040?
Reimbursement Medicare does not provide separate payment for genetic counseling; pro- cedure code 96040 is listed as status “B” (not separately paid) for both hospitals and freestanding centers. However, other insurers may allow separate reimbursement when genetic counseling meets their specific pay- ment requirements.
What is CPT code S0265?
S0265 is a valid 2022 HCPCS code for Genetic counseling, under physician supervision, each 15 minutes or just “Genetic counsel 15 mins” for short, used in Other medical items or services.
Is CPT 81220 genetic testing?
CPT® 81220, Under Genetic Analysis Procedures The Current Procedural Terminology (CPT®) code 81220 as maintained by American Medical Association, is a medical procedural code under the range - Genetic Analysis Procedures.
How much does CPT code 81420 Cost?
Noninvasive prenatal testing (CPT code 81420) is currently paid at $802 and its proposed reimbursement was reduced to $759, which market analysts, nonetheless, saw as a positive for NIPT providers such as Illumina and Natera.
What is the CPT code 81420?
81420: Fetal chromosomal aneuploidy (e.g., trisomy 21, monosomy X) genomic sequence analysis panel, circulating cell-free fetal DNA in maternal blood, must include analysis of chromosomes 13, 18, and 21.
What is a non-medical genetic test?
Many non-medical genetic tests exist that are used to help determine identity or genealogy. These may be available as an over-the-counter product but are not used to serve as any diagnostic resource to determine medical conditions or treatment options.
What is genetic testing?
Mainstream genetic testing for adults covers a wide range of conditions. These are typically categorized by the function they serve: 1 Diagnostic, predictive or presymptomatic. Patients who seek out these tests may already experience symptoms of a disease or, absent any symptoms, may know they have a family history of certain hereditary conditions. A genetic test can confirm or rule out an appropriate diagnosis. Examples of diseases that can be hereditary and confirmed by a genetic test include polycystic kidney disease (PKD) or hemochromatosis. Genetic testing can also reveal markers for many types of cancer, though it does not determine a certainty that the patient will develop that type of cancer. 2 Carrier. Though a person may never develop a condition or symptoms related to it, they may be a genetic carrier for that condition. A test that looks for genetic markers that indicate a person is a carrier of a hereditary disease can help them know whether they could pass or have already passed this gene down to a child if the other parent is also a carrier. 3 Pharmacogenomic. The study of genetics plays a major role in learning how the body metabolizes or reacts to certain medications. In some cases, a person’s genetic makeup can show whether a certain treatment will be effective or if it will cause an adverse reaction. This can help physicians target their treatment plan accordingly, which can improve the chances for successful outcomes for the patient’s health and recovery.
Why are genetic tests important?
Common Types of Genetic Testing for Adults. Because human DNA is so complex, the development of genetic tests is ongoing and new discoveries of how to apply testing to the diagnosis and treatment of disease are made frequently. Due to the still-incomplete understanding of the human genome, many of these tests remain in an experimental trial phase.
Can genetic testing reveal cancer?
Genetic testing can also reveal markers for many types of cancer, though it does not determine a certainty that the patient will develop that type of cancer. Carrier. Though a person may never develop a condition or symptoms related to it, they may be a genetic carrier for that condition.
Does Medicare cover genetic testing?
Medicare Advantage plans that offer extra benefits may extend the types of genetic tests covered, but these additional benefits vary from plan to plan. Medica re Part B may cover genetic testing when a recipient shows symptoms of medical conditions that have FDA-approved genetic tests developed for diagnosis.
Document Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
This LCD supplements but does not replace, modify or supersede existing Medicare applicable National Coverage Determinations (NCDs) or payment policy rules and regulations for BRCA1 and BRCA2 genetic testing services. Federal statute and subsequent Medicare regulations regarding provision and payment for medical services are lengthy.
Coverage Guidance
Notice: It is not appropriate to bill Medicare for services that are not covered (as described by this entire LCD) as if they are covered.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act, Section 1833 (e) states that no payment shall be made to any provider of services or other person under this part unless there has been furnished such information as may be necessary in order to determine the amounts due such provider or other person under this part for the period with respect to which the amounts are being paid or for any prior period..
Article Guidance
This Billing and Coding Article provides billing and coding guidance for Local Coverage Determination (LCD) L36499, BRCA1 and BRCA2 Genetic Testing. Please refer to the LCD for reasonable and necessary requirements.
ICD-10-CM Codes that Support Medical Necessity
It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted.
ICD-10-CM Codes that DO NOT Support Medical Necessity
All those not listed under the “ICD-10-CM Codes that Support Medical Necessity” section of this article.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
This First Coast Billing and Coding Article for Local Coverage Determination (LCD) L35698 CYP2C19, CYP2D6, CYP2C9, and VKORC1 Genetic Testing provides billing and coding guidance for frequency limitations as well as diagnosis limitations that support diagnosis to procedure code automated denials.
ICD-10-CM Codes that Support Medical Necessity
It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted.
ICD-10-CM Codes that DO NOT Support Medical Necessity
All those not listed under the “ICD-10 Codes that Support Medical Necessity” section of this article.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
General Information
CPT codes, descriptions and other data only are copyright 2021 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act, §1833 (e). Prohibits Medicare payment for any claim which lacks the necessary information to process the claim.
Article Guidance
The information in this article contains billing, coding or other guidelines that complement the Local Coverage Determination (LCD) for MolDX: NRAS Genetic Testing L35073. To report a NRAS Genetic Testing service, please submit the following claim information:
ICD-10-CM Codes that Support Medical Necessity
Although not specifically addressed in the ICD-10-CM Official Guidelines for Coding and Reporting 2016, when an encounter is for management of a complication associated with a neoplasm (NRAS testing for metastatic colon cancer), the complication (metastasis) is coded first, followed by the appropriate codes for the neoplasm.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act, Section 1833 (e) states that no payment shall be made to any provider of services or other person under this part unless there has been furnished such information as may be necessary in order to determine the amounts due such provider or other person under this part for the period with respect to which the amounts are being paid or for any prior period..
Article Guidance
This Billing and Coding Article provides billing and coding guidance for Local Coverage Determination (LCD) DL39063 Pharmacogenomics Testing. Please refer to the LCD for reasonable and necessary requirements.
ICD-10-CM Codes that Support Medical Necessity
It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted. The following ICD-10-CM code supports medical necessity and provides coverage for CPT code: 81220.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What is a NGS test?
Next Generation Sequencing (NGS) is one technique that can measure one or more genetic variations as a laboratory diagnostic test, such as when used as a companion in vitro diagnostic test.
Does Medicare cover myeloma?
Medicare does not have a National Coverage Determination (NCD) for MyPRS™ test for multiple myeloma gene expression profile. Local Coverage Determinations (LCDs)/Local Coverage Article (LCAs) exist and compliance with these policies is required where applicable. For specific LCDs/LCAs, refer to the table for MyPRS™ Test for Multiple Myeloma Gene Expression
Does Medicare have a national coverage determination?
Medicare does not have a National Coverage Determination (NCD) for PancraGEN®. Only one contractor has Local Coverage Determinations (LCDs) which address, i.e., Novitas Solutions, Inc., for the following states: AR, CO, DC, DE, LA, MD, MS, NJ, NM, OK, PA, and TX. Compliance with these LCDs is required where applicable. Refer to the LCD for Loss-of-Heterozygosity Based Topographic Genotyping with PathfinderTG® (L34864). This test is provided to Medicare beneficiaries throughout the United States by Interpace Diagnostics in Pittsburgh, PA.