(4) A policy filed with the office as a Medicare supplement policy must: (a) Have a definition of “Medicare eligible expense” that is not more restrictive than health care expenses of the kinds covered by Medicare or to the extent recognized as reasonable by Medicare.
Full Answer
Which is part of the minimum benefits required for Medicare supplements?
A Medicare supplement individual or group policy form shall not be delivered or issued for delivery unless the individual or group policy form can be expected, as estimated for the entire period for which rates are computed to provide coverage, to return to policyholders and certificate holders in the form of aggregated benefits (not including anticipated refunds or credits) …
What is a Medicare supplement insurance policy?
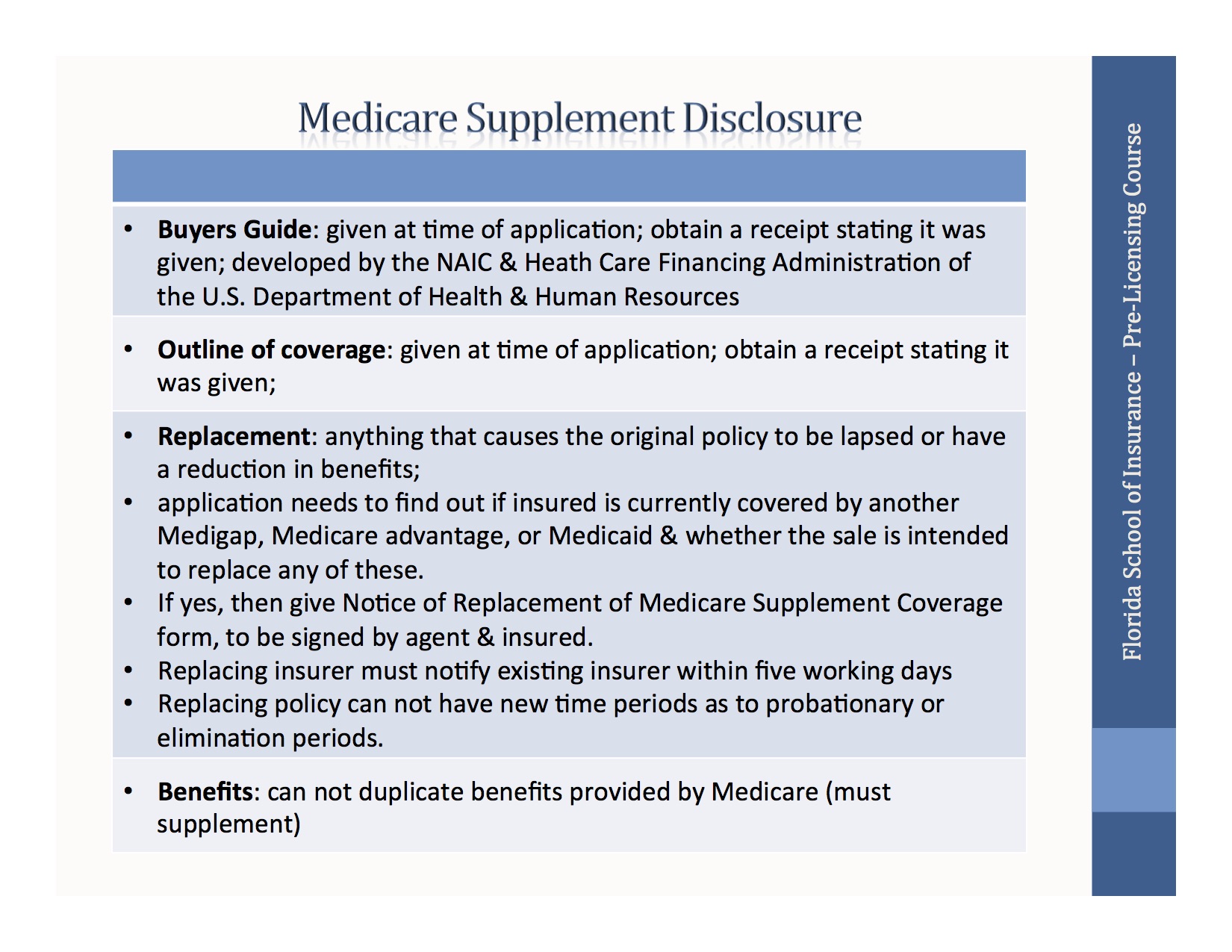
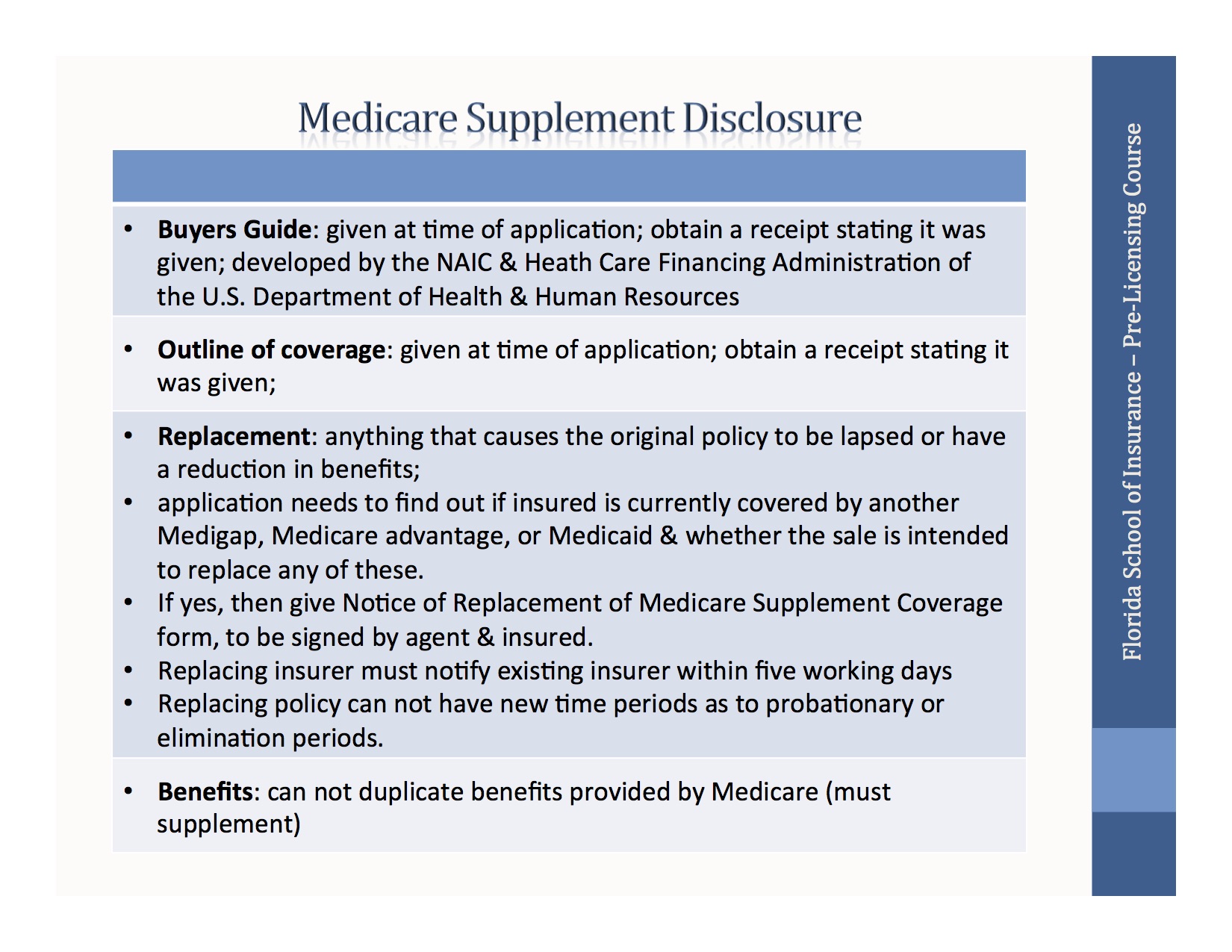
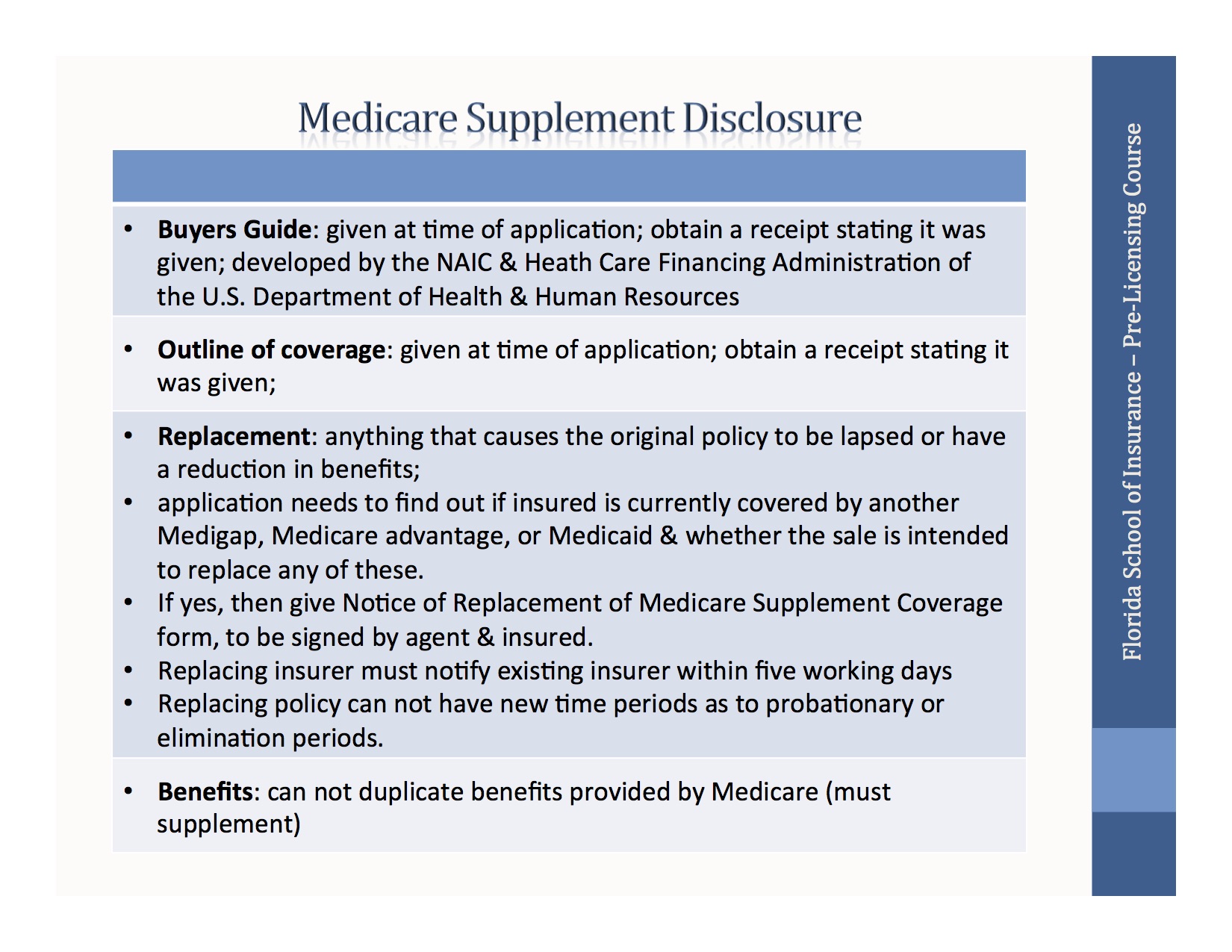
6.6.509 REQUIRED DISCLOSURE PROVISIONS (1) Medicare supplement policies and certificates must include a renewal or continuation provision. The language or specifications of the provision must be consistent with the type of contract to be issued. The provision must be appropriately captioned, must appear on the first page of the policy, and must include any reservation by the …
Are there any limitations on Medicare Supplement policies for pre-existing conditions?
Minimum benefit standards of medicare supplements: -expenses for 61-90 day in Medicare Part A -Coverage for Part A reserve days -100% part A expenses for hospitalization for 365 days over reserve days -3 pints of blood -coinsurance in part B subject to deductible -coverage of cost sharing for Part A hospice and Respite care
What is a Medicare select policy or Medicare select certificate?
No policy or certificate of Medicare Supplement insurance may be delivered in NC unless an outline of coverage is delivered to the applicant at the time application is made-outline of coverage-loss ratios Required Disclosures: ... Every Medicare SELECT policy must …
Which of the following must be included in a Medicare Supplement policy?
Medicare Supplement insurance Plan A covers 100% of four things: Medicare Part A coinsurance payments for inpatient hospital care up to an additional 365 days after Medicare benefits are used up. Medicare Part B copayment or coinsurance expenses. The first 3 pints of blood used in a medical procedure.
Which of the following must be included in a Medicare Supplement policy outline of coverage quizlet?
All Medicare supplement policies must provide certain core benefits, including coverage for Medicare Part A-eligible hospital expenses not covered by Medicare from the 61st day through the 90th day in any Medicare benefit period, the coinsurance amount of Medicare Part B-eligible expenses, and coverage under Medicare ...
What does a Medicare Supplement policy cover quizlet?
Also known as a Medigap Policy, is a health insurance policy sold by private insurance companies to fill in the coverage gaps in Original Medicare. The coverage gaps include deductibles and coinsurance requirements. The policies must follow federal and state laws.
What must a producer give an insured who purchased a Medicare Supplement policy at the time of application?
What must a producer give an insured who purchased a Medicare Supplement policy at the time of application? An outline of coverage (also called a policy summary) must be provided to a prospective buyer of a Medicare Supplement Policy at the time of application or policy delivery.
What is Medicare Supplement policies?
Medicare Supplement plans, also known as Medigap policies, are health insurance policies that limit the amount you'll pay for medical services once you are on Medicare. As you may know, both Medicare Part A and Part B have deductibles and other costs that you pay and don't have an out-of-pocket maximum.
Which of the following expenses are Medicare Supplement policies not designed to cover?
Medicare Supplement Plan B covers basic benefits plus Medicare Part A deductible for hospitalization. Neither Medicare Supplement Plan A nor Plan B covers skilled nursing facility care or at-home recovery care.
What is typically covered by supplemental plans quizlet?
What is typically covered by supplemental plans: copayments, coinsurance and deductibles.
Which type of care is not covered by Medicare quizlet?
Medicare Part A does not cover custodial or long-term care. Following is a breakdown of Part A SNF coverage, and the cost-sharing amounts that must be paid by the enrolled individual: -During the first 20 days of a benefit period, Medicare pays for all approved charges.
Which of the following is not covered by Medicare?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
What must the insurer provide to certificate holders when a group Medicare supplement insurance policy is terminated and not replaced?
If the Medicare supplement policy is terminated by the group policyholder and not replaced, an individual Medicare supplement policy must be offered to the certificateholders.
Who regulates Medicare Supplement plans?
Medicare Supplement plans are standardized and offer various benefits to help offset your healthcare cost. The California Department of Insurance (CDI) regulates Medicare Supplement policies underwritten by licensed insurance companies.
Which of the following is covered by Medicare Part B quizlet?
Part B helps cover medically-necessary services like doctors' services, outpatient care, durable medical equipment, home health services, and other medical services.
What is the core plan?
The benefits in Plan A, which is known as the core plan, must be contained in all other plans sold. Among the core benefits is coverage of Medicare Part A-eligible expenses for hospitalization, to the extent not covered by Medicare, from the 61st day through the 90th day in any Medicare benefit period.
How old do you have to be to qualify for Medicaid?
To qualify for Medicaid nursing home benefits, an individual must be at least 65 years old, blind, or disabled; be a U.S. citizen or permanent resident alien; need the type of care that is provided only in a nursing home; and meet certain asset and income tests.
What is Medicare Supplement Insurance?
Medicare supplement insurance fills the gaps in coverage left by Medicare, which provides hospital and medical expense benefits for persons aged 65 and older. All Medicare supplement policies must cover 100% of the Part A hospital coinsurance amount for each day used from.
How long does Medicare cover skilled nursing?
Medicare will cover treatment in a skilled nursing facility in full for the first 20 days. From the 21st to the 100th day, the patient must pay a daily co-payment. There are no Medicare benefits provided for treatment in a skilled nursing facility beyond 100 days. Medicare Part A covers.
What is Medicaid in the US?
Medicaid is a federal and state program designed to help provide needy persons, regardless of age, with medical coverage. A contract designed primarily to supplement reimbursement under Medicare for hospital, medical or surgical expenses is known as. A) an alternative benefits plan. B) a home health care plan.
What is intermediate care?
Intermediate care is provided under the supervision of a physician by registered nurses, licensed practical nurses, and nurse's aides. Intermediate care is provided in nursing homes for stable medical conditions that require daily, but not 24-hour, supervision. Tom is covered under Medicare Part A.
What is accelerated benefit?
Proceeds payable under a life insurance contract to a policyowner in anticipation of death or upon the occurrence of specified life-threatening conditions as defined by the policy are best described as: accelerated benefits. Producer commissions may NOT be paid to. licensed producers not appointed by an insurer.
Can a producer's license be suspended?
A producer's license may only be suspended or revoked if the producer. has been afforded a right to a hearing. Any advertisement that mentions a dollar amount, period of time for which any benefit is payable, cost of policy, policy benefit, or the loss for which the benefit is payable MUST disclose.
What is a producer in insurance?
When collecting insurance premiums from a client , a producer MUST. forward premiums to the insurer on a timely basis.