While Medicare is a federal health insurance program for seniors and disabled persons, Medicaid is a state and federal medical assistance program for financially needy persons of all ages. Both programs offer a variety of benefits, including physician visits and hospitalization, but only Medicaid provides long-term nursing home care.
Who runs the Medicare and Medicaid programs?
· The federal government runs the Medicare program. Each state runs its own Medicaid program. That’s why Medicare is basically the same all over the country, but Medicaid programs differ from state to state. The Centers for Medicare and Medicaid Services, part of the federal government, runs the Medicare program.
Is Medicare a state or federal program?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for …
What is Medicaid Medicaid?
· Medicare and Medicaid are U.S. government-sponsored programs designed to help cover healthcare costs for American citizens. Established in 1965 and funded by taxpayers, these two programs have...
What is the Centers for Medicare and Medicaid Services?
· Medicare Part A and Part B are provided by the federal government, and Medicare Part C and Part D, while federally governed, are provided by private insurance companies. Medicaid is a state government program that helps pay health care costs for people with limited income and resources, and different programs exist for specific populations.
Is Medicare federal program?
Medicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
Is Medicaid local or federal?
federalBACKGROUND: Medicaid is a federal entitlement program administered by states, with assistance from counties, that provides health and long-term care insurance to over 76 million low-income families and individuals, or one in five Americans.
What is federal Medicare Medicaid?
Medicare is a federal program that provides health coverage if you are 65+ or under 65 and have a disability, no matter your income. Medicaid is a state and federal program that provides health coverage if you have a very low income.
Is Medicare a federal program administered by states?
Medicare is a Federal Program with State Cooperation Our free comparison tool gives you a convenient way to find the private plans offered through Medicare Advantage, Part D prescription policies, and comprehensive care in Medicare Advantage.
Can you have Medicare and Medicaid?
Some Americans qualify for both Medicare and Medicaid, and when this happens, it usually means they don't have any out-of-pocket healthcare costs. Beneficiaries with Medicare and Medicaid are known as dual eligibles – and account for about 20 percent of Medicare beneficiaries (about 12.3 million people).
Who runs Medicare?
the Centers for Medicare & Medicaid ServicesMedicare is a federal program. It is basically the same everywhere in the United States and is run by the Centers for Medicare & Medicaid Services, an agency of the federal government.
Is Social Security federal or state?
federal governmentSocial Security is a program run by the federal government. The program works by using taxes paid into a trust fund to provide benefits to people who are eligible. You'll need a Social Security number when you apply for a job. Find how to apply for a Social Security number or to replace your Social Security card.
What came first Medicare or Medicaid?
On July 30, 1965, President Lyndon B. Johnson signed into law the Social Security Act Amendments, popularly known as the Medicare bill. It established Medicare, a health insurance program for the elderly, and Medicaid, a health insurance program for the poor.
Who is eligible for Medicaid?
Medicaid beneficiaries generally must be residents of the state in which they are receiving Medicaid. They must be either citizens of the United States or certain qualified non-citizens, such as lawful permanent residents. In addition, some eligibility groups are limited by age, or by pregnancy or parenting status.
What type of program is Medicare?
Medicare is the federal government program that provides health care coverage (health insurance) if you are 65+, under 65 and receiving Social Security Disability Insurance (SSDI) for a certain amount of time, or under 65 and with End-Stage Renal Disease (ESRD).
Is Medical federal or state?
Medi-Cal is a public health insurance program for low-income Californians. Medi-Cal—California's Medicaid program—is a state-federal program that offers free or low-cost health coverage to Californians with low family incomes.
What is the role of federal government in Medicare?
The federal government has played a major role in health care over the past half century from the establishment of Medicare and Medicaid in 1965—ensuring access to insurance coverage for a large portion of the U.S. population—to multiple pieces of legislation from the 1980s to early 2000s that protect individuals under ...
What is Medicare program?
The Medicare program is designed to give Medicare recipients multiple coverage options. It's composed of several different sub-parts, each of which provides insurance for a different type of healthcare service.
How is Medicare funded?
Medicare is funded: In part by the Medicare payroll tax (part of the Federal Insurance Contributions Act or FICA) In part by Medicare recipients’ premiums. In part by general federal taxes. The Medicare payroll taxes and premiums go into the Medicare Trust Fund.
What is the difference between medicaid and medicare?
Essentially, Medicare is for people who are over age 65 or have a disability, while Medicaid is for people with low incomes. Some people are eligible for both .
Why do people get Medicare?
Medicare recipients get Medicare because they paid for it through payroll taxes while they were working, and through monthly premiums once they’re enrolled.
How much will Medicare pay in 2021?
In 2021, the Part A premium for people who don't have enough work history is as high as $471 a month. 4 Very few Medicare beneficiaries pay a premium for Part A, though, as most people have a work history (or a spouse's work history) of at least ten years by the time they're eligible for Medicare.
Where do Medicare taxes go?
The Medicare payroll taxes and premiums go into the Medicare Trust Fund. Bills for healthcare services to Medicare recipients are paid from that fund. 11
How long do you have to be on Social Security to qualify for Medicare?
In most cases, you have to receive Social Security disability benefits for two years before you become eligible for Medicare (but there are exceptions for people with end-stage renal disease and amyotrophic lateral sclerosis). 2 . You’re eligible for Medicare if: You’re at least 65 years old.
Which pays first, Medicare or Medicaid?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second.
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
What is not covered by Medicare?
Offers benefits not normally covered by Medicare, like nursing home care and personal care services
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Does Medicare cover health care?
If you have Medicare and full Medicaid coverage, most of your health care costs are likely covered.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. . If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare.
Can you get medicaid if you have too much income?
Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid. The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid. In this case, you're eligible for Medicaid because you're considered "medically needy."
What is Medicare and Medicaid?
Medicare and Medicaid are U.S. government-sponsored programs designed to help cover healthcare costs for American citizens. Established in 1965 and funded by taxpayers, these two programs have similar-sounding names, which can trigger confusion about how they work and the coverage they provide.
How many parts does Medicare have?
Medicare has four parts that each cover different things—hospitalization, medically necessary services, supplemental coverage, and prescription drugs. The CARES Act extended the abilities of Medicare and Medicaid due to the COVID-19 pandemic.
What age does Medicare cover?
Medicare helps provide healthcare coverage to U.S. citizens who are 65 years of age or older, as well as people with certain disabilities. The four-part program includes:
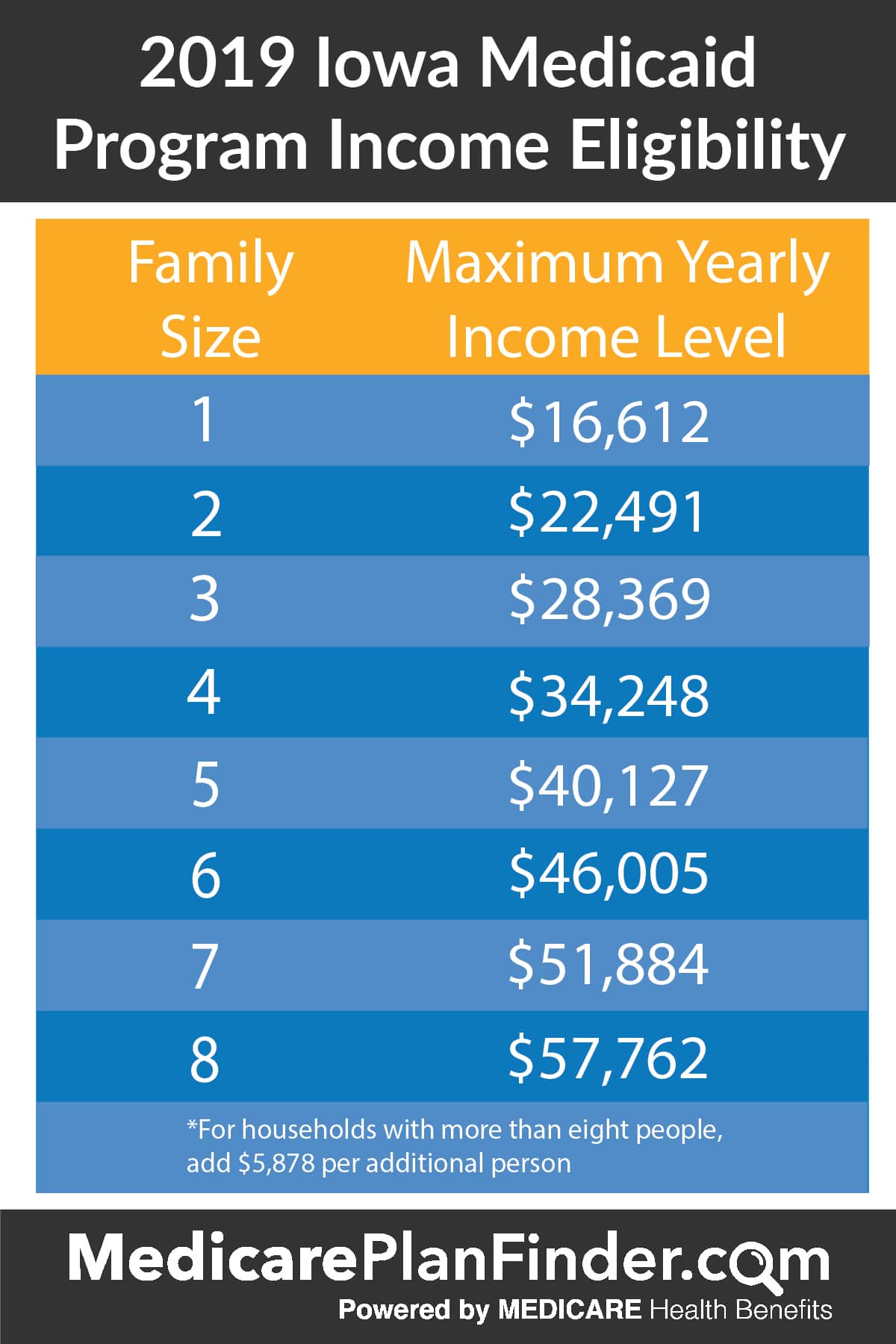
How much liquid assets do you need to get medicaid?
However, because the program is designed to help the poor, many states require Medicaid recipients to have no more than a few thousand dollars in liquid assets in order to participate. There are also income restrictions. For a state-by-state breakdown of eligibility requirements, visit Medicaid.gov and BenefitsCheckUp.org. 11
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy and durable medical equipment (DME). Part C premium. The Part C monthly premium varies by plan.
When does medicaid change?
When Medicaid recipients reach age 65, they remain eligible for Medicaid and also become eligible for Medicare. At that time, Medicaid coverage may change, based on the recipient's income. Higher-income individuals may find that Medicaid pays their Medicare Part B premiums. Lower-income individuals may continue to receive full benefits. 12
Does Medicare cover people over 65?
Medicare provides medical coverage for many people age 65 and older and those with a disability. Eligibility for Medicare has nothing to do with income level. Medicaid is designed for people with limited income and is often a program of last resort for those without access to other resources.
What is the difference between Medicare and Medicaid?
The Differences Between Medicare and Medicaid. The words “Medicare” and “Medicaid” are so much alike that it’s easy to get confused. To add to the confusion, both are government programs that help people pay for health care. But that’s where the similarities end. See below for more information about each program and how they compare.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
What is the blue circle on Medicare?
A blue Medicare circle and a white Medicaid circle emerge from the yellow circle. An orange Part D circle appears, then a blue line connects all of the outer circles and shrinks them into the yellow Medicare Advantage plan circle. A blue medical cross expands in the middle that reads DSNP.
What is Medicare Part D?
Medicare Part D is prescription drug coverage, and Part C (Medicare Advantage) is an all-in-one coverage option that combines Parts A, B and D, as well as other benefits that may include items like dental, vision, fitness and hearing. Medicare Part A and Part B coverage is standard, but Part C and Part D will vary based in terms ...
How old do you have to be to qualify for Medicare?
HOLLY: On the Medicare side, that means that you could’ve reached the magical age of 65 or that you can have a qualifying disability at ages 18 years all the way up to age 64.
Does Medicare cover copays?
Both Medicare and Medicaid may include premiums, deductibles, copays and coinsurance. For Medicare, how much you pay will vary based on when you enroll, what coverage options you select and what health services and items you use throughout the year. For Medicaid, the amount you pay depends on your income and the rules in your specific state. Additionally, some specific groups under Medicaid are exempt from many out-of-pocket costs.
Does medicaid pay out of pocket?
For Medicaid, the amount you pay depends on your income and the rules in your specific state. Additionally, some specific groups under Medicaid are exempt from many out-of-pocket costs. There are also four different Medicare Savings Programs, which are designed to help with the cost of Medicare.
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
How to apply for medicaid?
How to Apply. To apply for Medicare, contact your local Social Security Administration (SSA) office. To apply for Medicaid, contact your state’s Medicaid agency. Learn about the long-term care Medicaid application process. Prior to applying, one may wish to take a non-binding Medicaid eligibility test.
What is the CMS?
The Centers for Medicare and Medicaid Services, abbreviated as CMS, oversees both the Medicare and Medicaid programs. For the Medicaid program, CMS works with state agencies to administer the program in each state, and for the Medicare program, the Social Security Administration (SSA) is the agency through which persons apply.
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
What is dual eligible?
Definition: Dual Eligible. To be considered dually eligible, persons must be enrolled in Medicare Part A, which is hospital insurance, and / or Medicare Part B, which is medical insurance. As an alternative to Original Medicare (Part A and Part B), persons may opt for Medicare Part C, which is also known as Medicare Advantage.
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
How old do you have to be to qualify for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old. For persons who are disabled or have been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis), there is no age requirement. Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
What is Medicare for older people?
Medicare is the national health services program for older Americans. It has several parts designed to make a comprehensive healthcare system. It provides medical care, prescription drugs, and hospital care. The federal government has a strong legal responsibility when carrying out Medicare. It must keep a rule of medical necessity.
When did Medicare start to compete?
In effect, a competitive market of Medicare Advantage plans began when Congress authorized Medicare Part C in the 1990’s.
What is HMO in Medicare Advantage?
The below-itemized managed care types affect consumer choice in Medicare Advantage plans. HMO is the health maintenance organization. They feature prevention and wellness programs in addition to a network for medical services. They did not use outside resources.
What is Medicare Part C?
Medicare Part C – Medicare Advantage that include at least the coverage of Parts A and B, and many include Part D as well.
What does Medicare Supplement require?
States require a combination of comprehensive plans along with any limited option plans. The insurance companies can use medical underwriting to determine process, discriminate against applicants and reject applications.
What is CMS in healthcare?
Without a doubt, the massive undertaking to insure a diverse national population requires technical expertise and consistency. Essentially, the Center s for Medicare and Medicaid Services (CMS) hires several private contractors to process health claims and maintain records for large areas of the U.S.
Why did states turn down federal funds?
States turned down federal funds to expand coverage to their vulnerable residents. They declined although expansion would have reduced the numbers of uninsured residents and avoided the weight of unpaid bills that plague local hospitals and clinics.
What is the IFC for Medicare?
This interim final rule with comment period (IFC) gives individuals and entities that provide services to Medicare beneficiaries needed flexibilities to respond effectively to the serious public health threats posed by the spread of the 2019 Novel Coronavirus (COVID-19). Recognizing the urgency of this situation, and understanding that some pre-existing Medicare payment rules may inhibit innovative uses of technology and capacity that might otherwise be effective in the efforts to mitigate the impact of the pandemic on Medicare beneficiaries and the American public, we are changing Medicare payment rules during the Public Health Emergency (PHE) for the COVID-19 pandemic so that physicians and other practitioners, home health and hospice providers, inpatient rehabilitation facilities, rural health clinics (RHCs), and federally qualified health centers (FQHCs) are allowed broad flexibilities to furnish services using remote communications technology to avoid exposure risks to health care providers, patients, and the community. We are also altering the applicable payment policies to provide specimen collection fees for independent laboratories collecting specimens from beneficiaries who are homebound or inpatients (not in a hospital) for COVID-19 testing. We are also expanding, on an interim basis, the list of destinations for which Medicare covers ambulance transports under Medicare Part B. In addition, we are making programmatic changes to the Medicare Diabetes Prevention Program (MDPP) and the Comprehensive Care for Joint Replacement (CJR) Model in light of the PHE, and program-specific requirements for the Quality Payment Program to avoid inadvertently creating incentives to place cost considerations above patient safety. This IFC will modify the calculation of the 2021 and 2022 Part C and D Star Ratings to address the expected disruption to data collection and measure scores posed by the COVID-19 pandemic and also to avoid inadvertently creating incentives to place cost considerations above patient safety. This rule also amends the Medicaid home health regulations to allow other licensed practitioners to order home health services, for the period of this PHE for the COVID-19 pandemic in accordance with state scope of practice laws. We are also modifying our under arrangements policy during the PHE for the COVID-19 pandemic so that hospitals are allowed broader flexibilities to furnish inpatient services, including routine services outside the hospital.
How does telemedicine help Medicare?
Telemedicine, in particular has the potential to play a large role in enhancing the delivery of healthcare in the home, including the provision of information, education , and services provided via telecommunications systems. One of the benefits of telemedicine is its potential to minimize risk to clinicians and patients during an outbreak of an infectious disease, such as the PHE for the COVID-19 pandemic. Recently, we have been asked by stakeholders to provide more clarity on how hospices can leverage technology to keep clinicians and patients safe during the PHE for the COVID-19 pandemic.
What is home health?
Home health services include part-time or intermittent nursing, home health aide services, medical supplies, equipment, and appliances, and may include therapeutic services. Current Medicaid regulations require an individual's physician to order home health services as part of a written plan of care.
Does Medicare pay for telehealth?
[ 15] Starting on March 1, 2020, Medicare can pay for telehealth services, including office, hospital, and other visits furnished by physicians and other practitioners to patients located anywhere across the country including in a patient's place of residence. We have been asked by stakeholders to clarify whether this expansion applies to teaching physician services, including those furnished under the primary care exception. We believe that allowing Medicare payment for services billed by the teaching physician when the resident is furnishing services, including office/outpatient E/M services provided in primary care centers, via telehealth under direct supervision by interactive telecommunications technology would allow residents to furnish services remotely to patients who may need to be isolated for purposes of exposure risk based on presumed or confirmed COVID-19 infection, and as a result, would increase access to services for patients. To increase the capacity of teaching settings to respond to the PHE for the COVID-19 pandemic as more practitioners are increasingly being asked to assist with the COVID-19 response, we believe that, for telehealth services involving residents, the requirement that a teaching physician be present for key portions of the service can be met through virtual means. We also believe same is true for telehealth services furnished by the resident in primary care centers. The use of real-time, audio and video telecommunications technology allows for the teaching physician to interact with the resident through virtual means while the resident is furnishing services via telecommunications technology, and thus, in the circumstances of the PHE, would meet the requirement for teaching physician presence for office/outpatient E/M services furnished in primary care centers. Consequently, on an interim basis for the duration of the PHE for the COVID-19 pandemic, we are revising our regulations to specify that Medicare may make payment under the PFS for teaching physician services when a resident furnishes telehealth services to beneficiaries under direct supervision of the teaching physician which is provided by interactive telecommunications technology. Additionally, on an interim basis, for the duration of the PHE for the COVID-19 pandemic, Medicare may make payment under the PFS for services billed under the primary care exception by the teaching physician when a resident furnishes telehealth services to beneficiaries under the direct supervision of the teaching physician by interactive telecommunications technology. We also seek comment on our belief that direct supervision by interactive telecommunications technology is appropriate in the context of this PHE, as well as whether and how it balances risks that might be introduced for beneficiaries with reducing exposure risk and the increased spread of the disease, in the context of this PHE.