What is the Medicare Part D opioid overutilization policy?
This page contains information about Medicare Part D opioid overutilization policies including: Section 1860D-4 (c) (5) (A) of the Social Security Act permits Part D sponsors to establish drug management programs (DMPs) for beneficiaries who are at risk for misuse or abuse of frequently abused drugs (FADs).
What medications are not covered by Medicare Part D?
What Medications Are Not Covered by Part D? Medicare Part D is the prescription drug coverage arm of Medicare. Original Medicare focuses on inpatient hospital care and doctor visits under Part A and Part B, but it does not include any prescription drug coverage.
What is a drug management plan (DMP) for Part D?
Beginning January 1, 2022, all Part D sponsors are required to have a DMP, and to include beneficiaries with a history of opioid-related overdose in their DMP pursuant to the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities (SUPPORT) Act.
What is Medicare Part D prescription drug coverage?
Medicare offers prescription drug coverage (Part D) to everyone with Medicare. Medicare Part D plans are offered by private companies to help cover the cost of prescription drugs.
Are all Part D formularies the same?
Each plan can divide its tiers in different ways. Each tier costs a different amount. Generally, a drug in a lower tier will cost you less than a drug in a higher tier. A type of Medicare prescription drug coverage determination.
Do all Part D plans cover the same drugs?
Medicare drug coverage (Part D) helps you pay for both brand-name and generic drugs. Medicare drug plans are offered by insurance companies and other private companies approved by Medicare.
Which Medicare Part D plan covers OxyContin?
For all other Medicare prescription drug coverage, including coverage for the prescription drugs such as OxyContin you take at home, you'll need to enroll in Medicare Part D. You can get Part D coverage through: A stand-alone Medicare Prescription Drug Plan, which works with your Original Medicare coverage.
What drugs are excluded from Part D plans?
Drugs not covered under Medicare Part DWeight loss or weight gain drugs.Drugs for cosmetic purposes or hair growth.Fertility drugs.Drugs for sexual or erectile dysfunction.Over-the-counter drugs.
What is best Part D drug plan?
Best-rated Medicare Part D providersRankMedicare Part D providerMedicare star rating for Part D plans1Kaiser Permanente4.92UnitedHealthcare (AARP)3.93BlueCross BlueShield (Anthem)3.94Humana3.83 more rows•Mar 16, 2022
What are two options for Medicare consumers to get Part D prescription drug coverage assuming they meet all eligibility requirements )? Select 2?
There is no other way a Medicare consumer could get Part D prescription drug coverage. They could enroll in a Medicare Supplement Insurance Plan. They could enroll in a Medicare Advantage Plan or other Medicare health plan that includes prescription drug coverage.
Does Medicare cover Scrambler Therapy?
Is Scrambler Therapy Covered by Insurance? Based on what we have learned from the other universities around the country operating Scrambler programs, we anticipate that commercial insurers and Medicare will pay for the professional service fees charged by the physicians who provide the treatment.
What are Tier 1 Tier 2 and Tier 3 drugs?
There are typically three or four tiers: Tier 1: Least expensive drug options, often generic drugs. Tier 2: Higher price generic and lower-price brand-name drugs. Tier 3: Mainly higher price brand-name drugs.
Is Tramadol covered by Medicare?
Yes. 100% of Medicare prescription drug plans cover this drug.
Which of the following drug classes are excluded from coverage under Part D?
Drugs not covered under Medicare Part DWeight loss or weight gain drugs.Drugs for cosmetic purposes or hair growth.Fertility drugs.Drugs for sexual or erectile dysfunction.Over-the-counter drugs.
Which formulary restriction requires that you first use another drug before your prescribed medication can be approved for use?
Step Therapy In some cases, HealthTeam Advantage requires you to first try certain drugs to treat your medical condition before we will cover another drug for that condition.
Does Medicare Part D cover compound drugs?
Compound medications – Part D plans typically do not cover compounded medications. If you take a dose of a medication that is different from the standard dosage, that requires compounding, then typically you will pay the retail price for that medication.
When will Medicare Part D stop opioid overdose?
Effective January 1, 2019, CMS announced new strategies to further help Medicare Part D sponsors prevent and combat opioid overuse including additional safety alerts at the time of dispensing as a proactive step to engage both patients and prescribers about overdose risk and prevention.
When can Part D plans adopt DMPs?
As required by the Comprehensive Addiction and Recovery Act (CARA), in this final rule, CMS finalized the framework under which Part D plan sponsors may adopt drug management programs (DMPs) beginning January 1, 2019 for beneficiaries who are at-risk of misusing or abusing frequently abused drugs (FADs).
How long can you have opioids on Medicare?
First prescription fills for opioids. You may be limited to a 7-day supply or less if you haven’t recently taken opioids. Use of opioids and benzodiazepines at the same time.
What happens if a pharmacy doesn't fill a prescription?
If your pharmacy can’t fill your prescription as written, the pharmacist will give you a notice explaining how you or your doctor can call or write to your plan to ask for a coverage decision. If your health requires it, you can ask the plan for a fast coverage decision.
What is formulary exception?
A formulary exception is a drug plan's decision to cover a drug that's not on its drug list or to waive a coverage rule. A tiering exception is a drug plan's decision to charge a lower amount for a drug that's on its non-preferred drug tier.
Does Medicare cover opioid pain?
There also may be other pain treatment options available that Medicare doesn’t cover. Tell your doctor if you have a history of depression, substance abuse, childhood trauma or other health and/or personal issues that could make opioid use more dangerous for you. Never take more opioids than prescribed.
Do you have to talk to your doctor before filling a prescription?
In some cases, the Medicare drug plan or pharmacist may need to first talk to your doctor before the prescription can be filled. Your drug plan or pharmacist may do a safety review when you fill a prescription if you: Take potentially unsafe opioid amounts as determined by the drug plan or pharmacist. Take opioids with benzodiazepines like Xanax®, ...
Does Medicare cover prescription drugs?
In most cases, the prescription drugs you get in a Hospital outpatient setting, like an emergency department or during observation services , aren't covered by Medicare Part B (Medical Insurance). These are sometimes called "self-administered drugs" that you would normally take on your own. Your Medicare drug plan may cover these drugs under certain circumstances.
Does Medicare require prior authorization?
Your Medicare drug plan may require prior authorization for certain drugs. . In most cases, you must first try a certain, less expensive drug on the plan’s. A list of prescription drugs covered by a prescription drug plan or another insurance plan offering prescription drug benefits. Also called a drug list.
What is Medicare Part D?
Medicare Part D plans are offered by private companies to help cover the cost of prescription drugs. Everyone with Medicare can get this optional coverage to help lower their prescription drug costs. Medicare Part D generally covers both brand-name and generic prescription drugs at participating pharmacies.
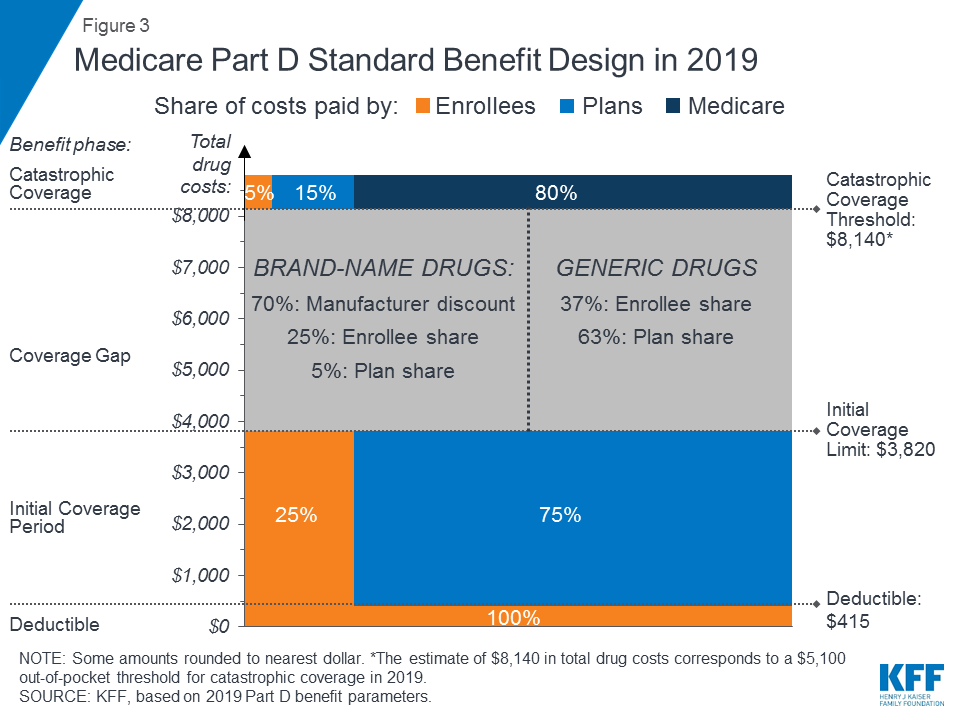
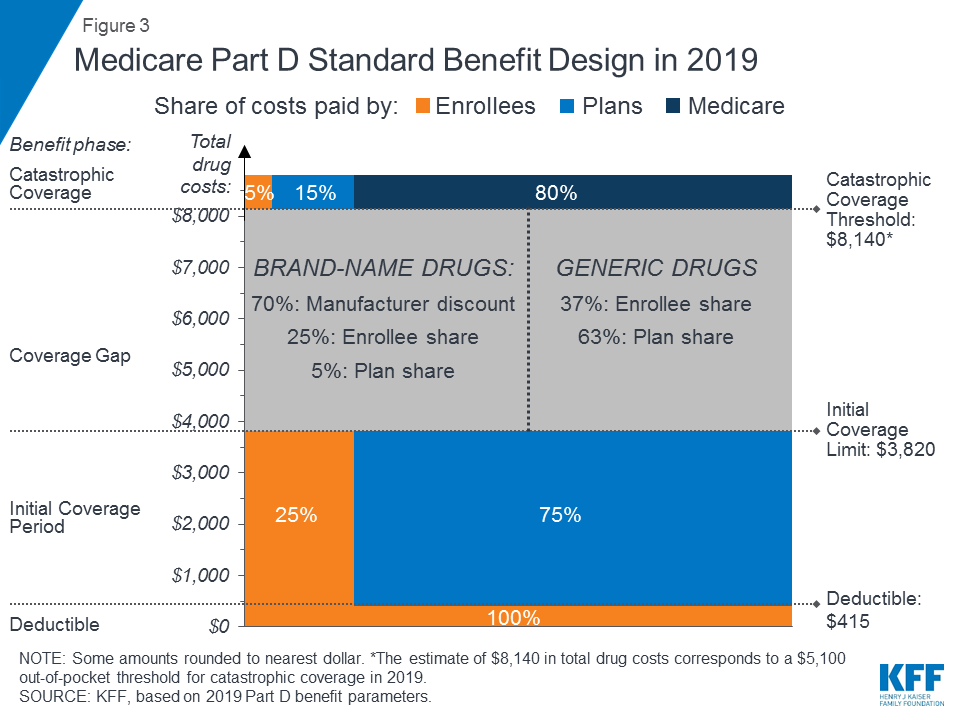
What is the gap in Medicare?
The Medicare Prescription Drug Coverage Gap (the “Doughnut Hole”) Most Medicare Part D plans have a coverage gap, sometimes called the “Doughnut Hole.”. This means that after you and your drug plan have spent a certain amount of money for covered drugs, you have to pay all costs out-of-pocket for the drugs, up to a yearly limit.
Is a discount card considered a prescription?
Note: Discount cards, doctor samples, free clinics, drug discount Web sites, and manufacturer’s pharmacy assistance programs are not considered prescription drug coverage and are not considered creditable coverage. Avoid the late-enrollment penalty. Join when you first become eligible.
Do you have to live in the service area of Medicare?
You must also live in the service area of the Medicare drug plan you want to join. Important Note for Medicare Beneficiaries with Employer or Union Coverage: If you have employer or union coverage, call your benefits administrator before you make any changes, or before you sign up for any other coverage.
Does Part D have a deductible?
Part D plans may have a monthly plan premium and a yearly deductible. These vary from plan to plan. You pay a portion of your drug costs, including a copayment or coinsurance. Costs vary depending on which drug plan you choose. Coverage options, including drug coverage, may vary from plan to plan.
Does Medicare cover generic drugs?
Whatever plan you choose, Medicare drug coverage will help you by covering brand-name and generic drugs at pharmacies that are convenient for you. Each Part D plan has a formulary – a list of medications the plan will cover. This list may also be referred to as a drug list, prescription drug list (PDL), or a covered medications list (CML).
What does "denial" mean in Part D?
You may also receive a denial from your Part D plan stating that your drug does not meet the FDA’s Drug Efficacy Study Implementation (DESI) standards. DESI evaluates the effectiveness drugs that had been previously approved on safety grounds alone.
Is a cold covered by Part D?
For example, a medicine for the relief of cold symptoms may be covered by Part D if prescribed to treat something other than a cold —such as shortness of breath from severe asthma—as long as it is approved by the U.S. Food and Drug Administration (FDA) for such treatment.
Does Medicare cover AIDS?
There are certain kinds of drugs that are excluded from Medicare coverage by law. Medicare does not cover: Note: Part D may cover drugs used to treat physical wasting caused by AIDS, cancer, or other diseases.
How to get prescription drug coverage
Find out how to get Medicare drug coverage. Learn about Medicare drug plans (Part D), Medicare Advantage Plans, more. Get the right Medicare drug plan for you.
What Medicare Part D drug plans cover
Overview of what Medicare drug plans cover. Learn about formularies, tiers of coverage, name brand and generic drug coverage. Official Medicare site.
How Part D works with other insurance
Learn about how Medicare Part D (drug coverage) works with other coverage, like employer or union health coverage.
Comparing Part D Prescription Drug Plans
Compare Part D prescription drug plans and enroll in the right plan for you. Learn how Medicaid and Medicare Part D work together so that eligible beneficiaries can save on their prescription drug costs.
Learn More About Medicare
Join our email series to receive your free Medicare guide and the latest information about Medicare and Medicare Advantage.
When will Part D coverage begin?
And if that should happen, you can’t get immediate coverage from Part D. Instead, you’d have to wait until the next annual open enrollment period (Oct. 15 to Dec. 7) and coverage wouldn’t begin until Jan. 1. Still, when you take no or very few medications, paying monthly premiums to a Part D drug plan can seem like a waste of money.
What happens if you don't enroll in Part D?
If you have no comparable drug coverage from elsewhere (such as from an employer, COBRA, retiree benefits or the Veterans Affairs health system) and if you don’t enroll in a Part D plan when you’re first eligible, you risk permanent late penalties when you do finally sign up.
Why do you pay for Part D insurance?
You pay premiums to protect yourself from the high costs of fire and accidents in the future, even if you never expect to make a claim. Part D plays a similar role: It’s there if and when you need it. The difference is that as you get older your chances of needing prescription drugs are far higher than the chances of totaling your car ...
What are the drugs not listed on a plan's formulary?
Drugs not listed on a plan's formulary. Drugs prescribed for anorexia, weight loss or weight gain. Drugs prescribed for fertility, erectile dysfunction, cosmetic purposes or hair growth. Prescription vitamins and minerals.
What is the deductible for Part D 2021?
In 2021, the annual deductible limit for Part D is $445. Copays are generally required each time you fill a prescription for a covered drug. Amounts can vary based on the plan’s formulary tiers as well as what pharmacy you use if the plan has network pharmacies.
What is the drug list in Medicare Advantage?
Medicare Part D and Medicare Advantage plans have a drug list (also called a formulary) that tells you what drugs are covered by a plan. Medicare sets standards for the types of drugs Part D plans must cover, but each plan chooses the specific brand name and generic drugs to include on its formulary.
How to save on prescription drug costs?
Order 90-day supplies. You may be able to save on prescription drug costs by ordering 90-day supplies. Use a preferred network pharmacy. Many plans offer cost savings if you fill your prescriptions at a pharmacy that's part of the plan's preferred network.
What is a B/D?
B/D – Medicare Part B or Medicare Part D Coverage Determination. Some drugs can be covered by either Medicare Part B (doctor and outpatient health care) or Medicare Part D (prescription drugs). The plan needs more information about how a drug will be used to make sure it's covered by the right part of Medicare.
What is the D coverage gap?
A note about the Part D coverage gap (donut hole) The Part D coverage gap—also known as the "donut hole"—opens when you and your plan have paid up to a certain limit for your drugs in the one year. When you're in this stage, you pay a bigger share of the costs for your prescriptions than before.
Do you have to pay a monthly premium for Medicare Part D?
Costs you could pay with Medicare Part D. With stand-alone Part D plans, you will pay a monthly premium and may also pay an annual deductible, copays and coinsurance. Some plans charge deductibles, some do not, but Medicare sets a maximum deductible amount each year.
