What is FFS Medicare?
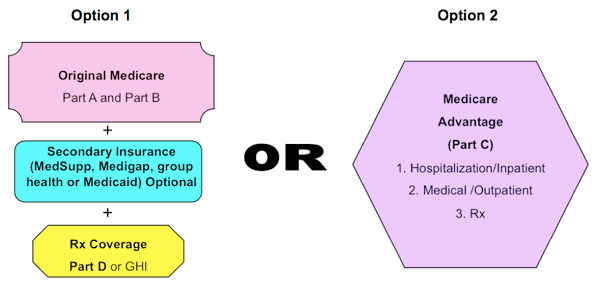
It is sometimes called Traditional Medicare or Fee-for-Service (FFS) Medicare. Under Original Medicare, the government pays directly for the health care services you receive. You can see any doctor and hospital that takes Medicare (and most do) anywhere in the country. You go directly to the doctor or hospital when you need care.
When should Medicare FFS testing with external trading partners begin?
Also in compliance with the published regulation (RIN 0938-AM50 of 45 CFR Part 162), Medicare FFS testing with external trading partners must begin in January of 2011. The CMS HETSHelp site provides information specific to the HIPAA Eligibility Transaction System (HETS) for 270/271 Medicare eligibility transactions.
What is Original Medicare or fee-for-service?
Most beneficiaries choose to receive their Parts A and B benefits through Original Medicare, the traditional fee-for-service program offered directly through the federal government. It is sometimes called Traditional Medicare or Fee-for-Service (FFS) Medicare.
What is Medicare fee-for-service compliance?
The Medicare Fee-for-Service Compliance programs prevent, reduce, and measure improper payments in FFS Medicare through medical review. We provide a number of programs to educate and support Medicare providers in understanding and applying Medicare FFS policies while reducing provider burden.
Is facial feminization surgery covered by Medicare?
Medicare does not cover certain cosmetic surgery procedures, such as laser hair removal and facial feminization surgery, because these are not considered medically necessary.
What is a Medicare FFS claim?
Medicare Fee-for-Service (FFS) Recovery Audit Contractors (RACs) review claims on a post-payment basis. The RACs detect and correct past improper payments so that CMS can implement actions that will prevent future improper payments in all 50 states. Read more about the Medicare FFS Recovery Audit Program.
What is Medicare Part B for?
Part B helps pay for covered medical services and items when they are medically necessary. Part B also covers some preventive services like exams, lab tests, and screening shots to help prevent, find, or manage a medical problem. Cost: If you have Part B, you pay a Part B premium each month.
What is Medicare Part C used for?
Medicare Part C covers the inpatient care typically covered by Medicare Part A. If you are a Medicare Part C subscriber and are admitted to the hospital, your Medicare Advantage plan must cover a semi-private room, general nursing care, meals, hospital supplies, and medications administered as part of inpatient care.
Is Medicare Part C fee-for-service?
A Medicare Private Fee-for-Service plan is a type of Medicare Advantage plan (Part C) administered by a private insurance company. The plan determines how much you must pay when you get care. Doctors decide whether to accept patients with PFFS plans.
What is Medicare fee-for-service vs managed care?
Under the FFS model, the state pays providers directly for each covered service received by a Medicaid beneficiary. Under managed care, the state pays a fee to a managed care plan for each person enrolled in the plan.
What is difference between Part A and Part B Medicare?
If you're wondering what Medicare Part A covers and what Part B covers: Medicare Part A generally helps pay your costs as a hospital inpatient. Medicare Part B may help pay for doctor visits, preventive services, lab tests, medical equipment and supplies, and more.
What is the difference between Part B and Part D Medicare?
Medicare Part B only covers certain medications for some health conditions, while Part D offers a wider range of prescription coverage. Part B drugs are often administered by a health care provider (i.e. vaccines, injections, infusions, nebulizers, etc.), or through medical equipment at home.
Who pays for Medicare Part A?
Most people receive Medicare Part A automatically when they turn age 65 and pay no monthly premiums. If you or your spouse haven't worked at least 40 quarters, you'll pay a monthly premium for Part A.
What's the difference between Medicare Part C and D?
Medicare Part C is an alternative to original Medicare. It must offer the same basic benefits as original Medicare, but some plans also offer additional benefits, such as vision and dental care. Medicare Part D, on the other hand, is a plan that people can enroll in to receive prescription drug coverage.
Does Medicare Part C replace A and B?
Part C (Medicare Advantage) Under Medicare Part C, you are covered for all Medicare parts A and B services. Most Medicare Advantage plans also cover you for prescription drugs, dental, vision, hearing services, and more.
Do I qualify for Medicare Part C?
You must be at least age 65 or older and a U.S. citizen or legal permanent resident for a minimum of 5 contiguous years. Disability. If you've received monthly Social Security or Railroad Retirement Board (RRB) disability benefits for 24 months, you're eligible for Original Medicare.
What Is The Medicare Shared Savings Program
What Is A Medicare Private-Fee-For-Service Plan? Should You Join A Medicare PFFS Plan?
D: Prescription Drug Plans
Medicare Part D went into effect on January 1, 2006. Anyone with Part A or B is eligible for Part D, which covers mostly self-administered drugs. It was made possible by the passage of the Medicare Modernization Act of 2003.
Provider Payment And Delivery Systems
States may offer Medicaid benefits on a fee-for-service basis, through managed care plans, or both. Under the FFS model, the state pays providers directly for each covered service received by a Medicaid beneficiary. Under managed care, the state pays a fee to a managed care plan for each person enrolled in the plan.
Mma Initiatives For Private Plans 2006
The 2003 MMA legislation increased payments to private plans for 2004-2005. It also created a new type of private planthe regional PPOand created special payment arrangements for this type of plan and for local plans. The payment arrangements for both plans are based on a comparison of benchmark prices and bids by plans for Parts A and B coverage.
What Is The Purpose Of The Medical Review Program
Medical reviews identify errors through claims analysis and/or medical record review activities. Contractors use this information to help ensure they provide proper Medicare payments . Contractors also provide education to help ensure future compliance.
Competitive Pricing For Private Plans: 1995
Beginning in 1995, CMS began a series of demonstration projects centered on competitive pricing as a method for paying private health plans in Medicare. Instead of payments based on costs in FFS Medicare, private plans would be paid on the basis of bids in local market areas.
Fee For Service Vs Value Added Model
Ready to see the difference a private plan makes? Call now to talk to a licensed insurance agent about your options or click Compare Plans to see the Medicare options available where you live. Your coverage matters. Let us help you find the right plan.
The Medicare FFS Approach
The purpose of this message is to clearly communicate the approach that Medicare Fee-For-Service (FFS) is taking to ensure compliance with the Health Insurance Portability and Accountability Act's (HIPAA's) new versions of the Accredited Standards Committee (ASC) X12 and the National Council for Prescription Drug Programs (NCPDP) Electronic Data Interchange (EDI) transactions..
CMS HETSHelp site
The CMS HETSHelp site provides information specific to the HIPAA Eligibility Transaction System (HETS) for 270/271 Medicare eligibility transactions. Please visit the HETSHelp site at: http://www.cms.hhs.gov/HETSHelp/ for details about the changes being made to HETS to support the X12 5010 standard.
What is Medicare Fee for Service Compliance?
The Medicare Fee-for-Service Compliance programs prevent, reduce, and measure improper payments in FFS Medicare through medical review. We provide a number of programs to educate and support Medicare providers in understanding and applying Medicare FFS policies while reducing provider burden.
Why is Medicare simplifying documentation requirements?
Medicare is simplifying documentation requirements so that you spend less time on paperwork, allowing you to focus more on your patients and less on confusing and time-consuming claims documentation. Learn about what we are doing.
What is a CBR in Medicare?
A CBR provides data on Medicare billing trends, allowing a health care provider to compare their billing practices to peers in the same state and across the nation. A CBR educates providers about Medicare’s coverage, coding, and billing rules and acts as a self-audit tool for providers.
What is national coverage?
National coverage decisions made by Medicare about whether something is covered. Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
Is Medicare Advantage the same as Original Medicare?
What's covered? Note. If you're in a Medicare Advantage Plan or other Medicare plan, your plan may have different rules. But, your plan must give you at least the same coverage as Original Medicare. Some services may only be covered in certain settings or for patients with certain conditions.
How much is Medicare reimbursement for 2020?
Reimbursements match similar in-person services, increasing from about $14-$41 to about $60-$137, retroactive to March 1, 2020. In addition, Medicare is temporarily waiving the audio-video requirement for many telehealth services during the COVID-19 public health emergency. Codes that have audio-only waivers during the public health emergency are ...
Does Medicare cover telehealth?
Telehealth codes covered by Medicare. Medicare added over one hundred CPT and HCPCS codes to the telehealth services list for the duration of the COVID-19 public health emergency. Telehealth visits billed to Medicare are paid at the same Medicare Fee-for-Service (FFS) rate as an in-person visit during the COVID-19 public health emergency.
What is Medicare Part A?
Medicare Part A (hospital insurance) covers inpatient care in a hospital, skilled nursing facility and religious non-medical health care institution.
What is facial feminization surgery?
Facial feminization surgery (FFS) is undertaken to reconstruct masculine facial features to present a feminine form. The objective is to soften the facial aspects that are commonly considered masculine such as the nasal shape and bone structure. Soft tissue in the face or neck may also be altered.
Is breast reconstruction covered by Medicare?
Additionally, breast reconstruction following the mastectomy of a breast cancer patient is covered.
Is facial feminization surgery covered by Medicare?
Coverage for Facial Feminization Surgery. If Medicare classifies a facial feminization procedure as an elective cosmetic surgery, it is unlikely to be covered.