Which part of Medicare pays for inpatient?
Part APart A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
What is covered by Medicare Part C?
What Does Medicare Part C Cover?Routine dental care including X-rays, exams, and dentures.Vision care including glasses and contacts.Hearing care including testing and hearing aids.Wellness programs and fitness center memberships.
Is Medicare Part A for inpatient only?
Medicare Part A (Hospital Insurance) covers inpatient hospital services. Generally, this means you pay a one-time deductible for all of your hospital services for the first 60 days you're in a hospital. Medicare Part B (Medical Insurance) covers most of your doctor services when you're an inpatient.
Which part of Medicare covers both inpatient and outpatient?
Part A provides inpatient/hospital coverage. Part B provides outpatient/medical coverage. Part C offers an alternate way to receive your Medicare benefits (see below for more information). Part D provides prescription drug coverage.
What is the difference between Medicare Part C and Part D?
Medicare part C is called "Medicare Advantage" and gives you additional coverage. Part D gives you prescription drug coverage.
What is Part D in Medicare explained?
Medicare Part D is a voluntary outpatient prescription drug benefit for people with Medicare, provided through private plans approved by the federal government.Oct 13, 2021
Does Medicare cover hospitals?
Medicare generally covers 100% of your medical expenses if you are admitted as a public patient in a public hospital. As a public patient, you generally won't be able to choose your own doctor or choose the day that you are admitted to hospital.Jun 24, 2021
What is Medicare inpatient only list?
What is the Medicare inpatient-only list? The Medicare inpatient-only list refers to procedures and services that CMS has identified as typically only provided in the inpatient setting and therefore not paid under OPPS.
What do Medicare Parts A and B cover?
Part A (Hospital Insurance): Helps cover inpatient care in hospitals, skilled nursing facility care, hospice care, and home health care. Part B (Medical Insurance): Helps cover: Services from doctors and other health care providers.
Is MA and Part C the same thing?
A Medicare Advantage Plan (like an HMO or PPO) is another Medicare health plan choice you may have as part of Medicare. Medicare Advantage Plans, sometimes called “Part C” or “MA Plans,” are offered by private companies approved by Medicare.
What's the difference between Medicare Part A and Part B?
Medicare Part A and Medicare Part B are two aspects of healthcare coverage the Centers for Medicare & Medicaid Services provide. Part A is hospital coverage, while Part B is more for doctor's visits and other aspects of outpatient medical care.
What is Medicare Part B also known as?
Medicare Part B (also known as medical insurance) is an insurance plan that covers medical services related to outpatient and doctor care.
What is national coverage?
National coverage decisions made by Medicare about whether something is covered. Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
Is Medicare Advantage the same as Original Medicare?
What's covered? Note. If you're in a Medicare Advantage Plan or other Medicare plan, your plan may have different rules. But, your plan must give you at least the same coverage as Original Medicare. Some services may only be covered in certain settings or for patients with certain conditions.
How does hospital status affect Medicare?
Inpatient or outpatient hospital status affects your costs. Your hospital status—whether you're an inpatient or an outpatient—affects how much you pay for hospital services (like X-rays, drugs, and lab tests ). Your hospital status may also affect whether Medicare will cover care you get in a skilled nursing facility ...
How long does an inpatient stay in the hospital?
Inpatient after your admission. Your inpatient hospital stay and all related outpatient services provided during the 3 days before your admission date. Your doctor services. You come to the ED with chest pain, and the hospital keeps you for 2 nights.
What is an ED in hospital?
You're in the Emergency Department (ED) (also known as the Emergency Room or "ER") and then you're formally admitted to the hospital with a doctor's order. Outpatient until you’re formally admitted as an inpatient based on your doctor’s order. Inpatient after your admission.
When is an inpatient admission appropriate?
An inpatient admission is generally appropriate when you’re expected to need 2 or more midnights of medically necessary hospital care. But, your doctor must order such admission and the hospital must formally admit you in order for you to become an inpatient.
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. , coinsurance. An amount you may be required to pay as your share of the cost for services after you pay any deductibles.
Is an outpatient an inpatient?
You're an outpatient if you're getting emergency department services, observation services, outpatient surgery, lab tests, or X-rays, or any other hospital services, and the doctor hasn't written an order to admit you to a hospital as an inpatient. In these cases, you're an outpatient even if you spend the night in the hospital.
Does Medicare cover skilled nursing?
Your hospital status may also affect whether Medicare will cover care you get in a skilled nursing facility (SNF) following your hospital stay. You're an inpatient starting when you're formally admitted to the hospital with a doctor's order. The day before you're discharged is your last inpatient day. You're an outpatient if you're getting ...
What is part A in rehabilitation?
Inpatient rehabilitation care. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.
What is the benefit period for Medicare?
benefit period. The way that Original Medicare measures your use of hospital and skilled nursing facility (SNF) services. A benefit period begins the day you're admitted as an inpatient in a hospital or SNF. The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row.
How long does it take to get into an inpatient rehab facility?
You’re admitted to an inpatient rehabilitation facility within 60 days of being discharged from a hospital.
Does Medicare cover private duty nursing?
Medicare doesn’t cover: Private duty nursing. A phone or television in your room. Personal items, like toothpaste, socks, or razors (except when a hospital provides them as part of your hospital admission pack). A private room, unless medically necessary.
Does Medicare cover outpatient care?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
What Can You Expect To Pay For An Approved Inpatient Surgery
Medicare Part A generally covers much of the cost related to your inpatient surgery and hospital stay. You may be responsible for a Medicare Part A deductible for each benefit period.
Is Medicare Part A Free At Age 65
Premium-free Part A coverage is available if you or your spouse paid Medicare taxes for a certain amount of time while working. You can receive this if:
Do You Have To Pay A Part A Premium
You may be wondering does Medicare Part A cover 100 percent? And while this is not the case, there are provisions in place to make Medicare affordable to beneficiaries.
Does Medicare Cover Inpatient Mental Health Treatment
You must have Medicare Part A to be covered for inpatient mental health treatment at a general or psychiatric hospital. Medicare will pay for most of your inpatient treatment services. However, you may still owe some out-of-pocket costs depending on your plan and the length of your stay.
Hospital Stay Coverage Under Medicare Advantage
You may choose to receive your Medicare Part A and Part B coverage through a local Medicare Advantage plan. Medicare Advantage plans are offered by private insurance companies that are approved by Medicare and cover at least the same level of benefits as Original Medicare Part A and Part B .
Hospital Observation Status And Medication Costs
Any prescription and over-the-counter drugs you receive in an outpatient setting arent covered by Part B. But if you have Medicare Part D , they may be covered in certain circumstances. If the drugs are covered, youll probably need to pay out of pocket and submit a claim to your drug plan for a refund.
What Medicare Part A Does Not Cover
While this part of Medicare covers stays in a nursing home, it will only do so if it is medically necessary. If you need non-medical long-term care, such as for chronic illness or disability, youâll have to consider other options like long-term care insurance.
Medicare Part A eligibility
If you’re age 65 or older or have certain disabilities, you’re likely eligible for Medicare, a form of government-sponsored medical insurance. Part A is paid via Medicare payroll taxes withheld from your paychecks over your working life.
How much is Medicare Part A?
The good news is that you typically don’t have to pay a monthly premium for Part A. That’s true so long as you or your spouse paid sufficient Medicare taxes over your lifetime.
Medicare Part A deductible
Aside from premiums, Medicare Part A recipients may also pay out-of-pocket costs, including a deductible and coinsurance .
How to sign up for Medicare Part A
Most people eligible for Medicare Part A and B are enrolled automatically.
Medicare Part A vs. Part B
Part A and Part B are both components of Original Medicare, but they cover different health care services.
Frequently Asked Questions
If you already have Medicare Part A but need Medicare Part B, there are forms you and your employer (if applicable) need to complete to enroll in Part B without having to pay penalties, according to Reese. If you missed your qualifying window, there’s a general enrollment period between Oct. 15 and Dec. 7.
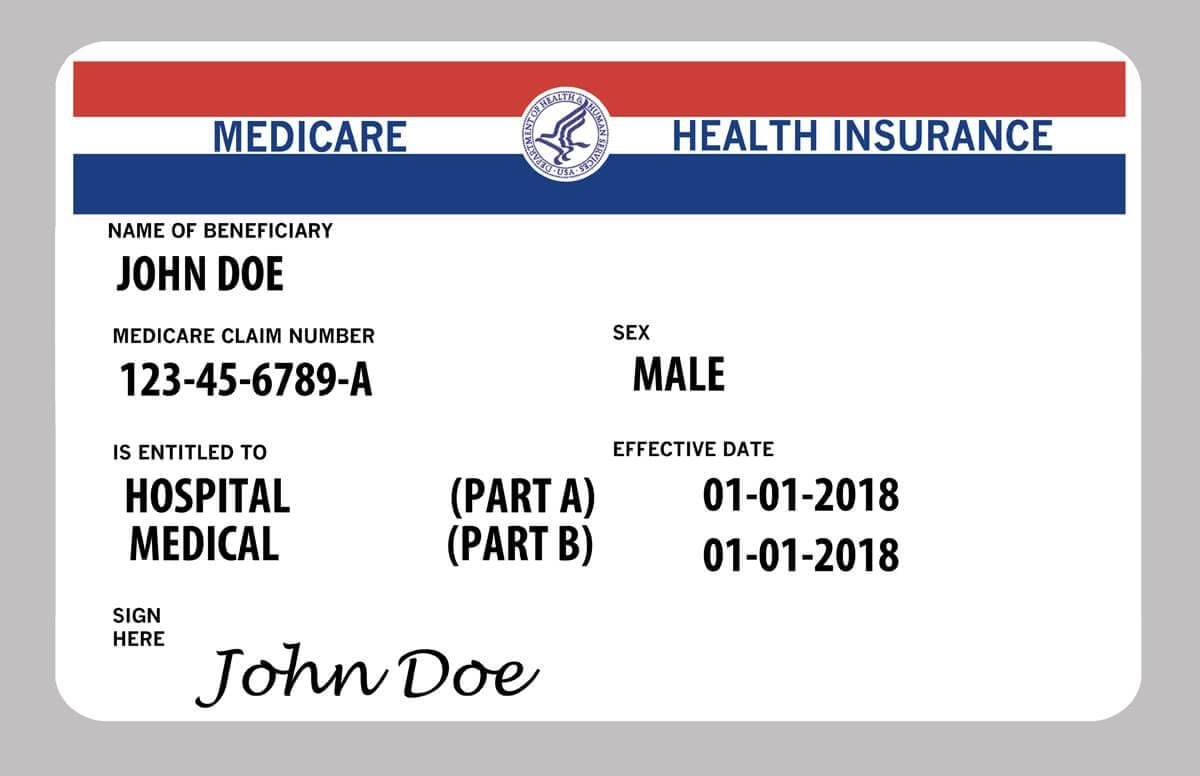
What is Medicare Part A?
Medicare Part A generally covers inpatient medical services. This includes stays in a hospital or nursing facility. It also pays for some home care and hospice. Find a Medicare Plan that Fits Your Needs Get a Free Medicare Plan Review. Get Started.
How much does Medicare pay for hospital stays?
Hospital stays. The amount covered depends on how long you're in the hospital. In 2019, for the first 60 days, you pay a deductible of $1,364 for each benefit period and Medicare pays the rest. After that, the longer you stay, the more you pay. You pay $341 per day for days 61 through 90.
What happens if you don't pay Medicare taxes?
But if neither you nor your spouse worked and paid Medicare taxes for 10 years, you will have to pay an additional monthly fee depending on how long you worked. If you enroll late, you will be penalized by paying a higher monthly amount. Medicare Part A pays some of the charges for: Hospital stays.
How much does Medicare pay for skilled nursing?
Medicare pays in full for the first 20 days. From the 21st to 100th day, you pay a co-pay of $170.50 per day in 2019. After that, you pay all the costs of your stay in a skilled nursing facility. Home health care.
How long does skilled nursing care last?
Medicare will cover the cost of skilled nursing care for a maximum of 100 days. Medicare pays in full for the first 20 days.
How many days does Medicare cover?
Original Medicare covers up to 90 days in a hospital per benefit period and offers an additional 60 days of coverage with a high coinsurance. These 60 reserve days are available to you only once during your lifetime. However, you can apply the days toward different hospital stays. For days 91 and beyond in the hospital, ...
Do hospitals pay for blood?
In most cases, the hospital gets blood from a blood bank at no charge, and you won’t have to pay for it or replace it. If the hospital has to buy blood for you, you must either pay the hospital costs for the first three units of blood you get in a calendar year or have the blood donated.
How much does Medicare cover inpatients?
Does Medicare Part A Cover 100 Percent? For a qualifying inpatient stay, Medicare Part A covers 100 percent of hospital-specific costs for the first 60 days of the stay — after you pay the deductible for that benefit period.
What is Medicare Part A?
Medicare Part A#N#Medicare Part A, also called "hospital insurance ," covers the care you receive while admitted to the hospital, skilled nursing facility, or other inpatient services. Medicare Part A is part of Original Medicare.#N#provides coverage to U.S. citizens age 65 and older for inpatient stays in hospitals and similar medical facilities.
What is Medicare Original?
Original Medicare is a fee-for-service health insurance program available to Americans aged 65 and older and some individuals with disabilities. Original Medicare is provided by the federal government and is made up of two parts: Part A (hospital insurance) and Part B (medical insurance). or other medical insurance may provide coverage.
How long does it take to pay coinsurance for Medicare?
After 60 days , you must pay coinsurance that Part A doesn’t cover. For hospital expenses covered by Part B, you have to pay 20 percent coinsurance after meeting your annual deductible. Part A and B are collectively known as Original Medicare and work hand-in-hand to help cover hospital stays.
How long does Medicare Part A and Part B last?
Your IEP begins three months before the month you turn 65. The IEP is open for a total of seven months and allows you to enroll in Medicare Part A and Part B.
Why is Medicare Part A called Medicare Part A?
Medicare Part A is commonly referred to as “hospital insurance” because its primary function is to help older adults manage the cost of hospital bills.
Does Medicare cover chemotherapy?
What does Medicare Part A cover and not cover based on your status as a patient? If, for example, you need chemotherapy, Part A will cover it if it’s administered as a part of an inpatient hospital stay; if it’s done on an outpatient basis, Part A won’t cover it (but Part B will).
