The CMS is the only rating entity that provides a separate rating for Aetna’s Medicare Part D plans. A.M. Best rates CVS Health corporation as a whole. The BBB rates Aetna, Inc., and Consumer Affairs rates CVS Pharmacy.
Full Answer
What is a Aetna Medicare network pharmacy?
We call them network pharmacies because we’ve contracted with them to provide prescription drugs to Aetna Medicare plan members. In most cases, your prescriptions are covered under our plan only if they’re filled either:
What is Aetna Medicare Part D?
What is Aetna Medicare Part D? Congress authorized Medicare Part D Prescription Drug Plans under the Medicare Prescription Drug, Improvement, and Modernization Act of 2003, making Medicare prescription drug coverage available to beneficiaries for the first time in 2006. Medicare prescription drug is available in one of two ways.
Does Medicare Part D have a pharmacy network?
Medicare Part D plans have a network of pharmacies. Usually you must use a network pharmacy for the plan to pay for your prescription. Different plans may have different pharmacy networks, so it's always best to check.
What are Aetna covered drugs?
Covered drugs are limited to those included in the plan’s drug formulary, which is a list of medications covered by the plan and details about how much the plan will cover. Formularies may vary by plan and location and may change at any time. Your Aetna Medicare plan will notify you if necessary.
See more
Is Walgreens a preferred pharmacy for Medicare?
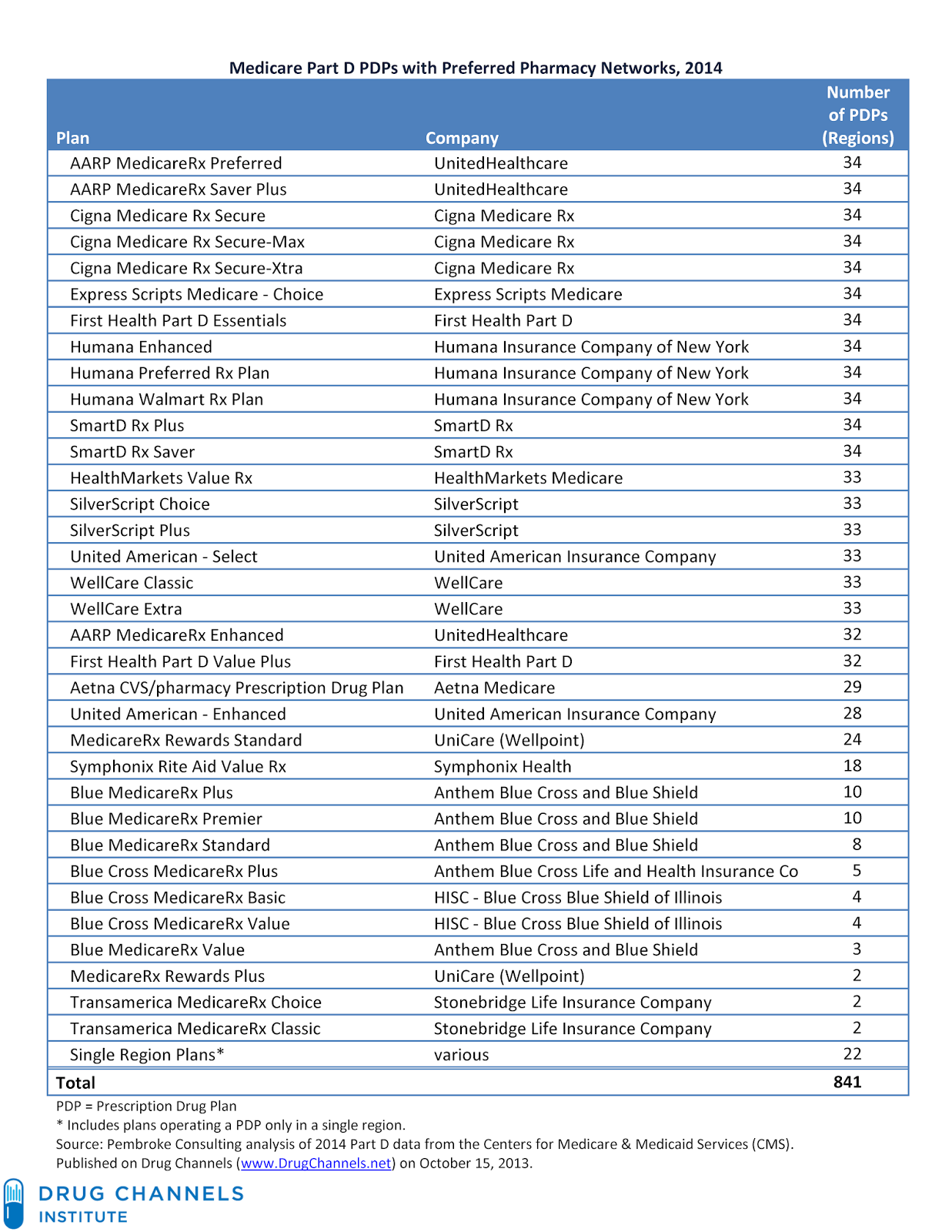
Walgreens will continue to be a part of preferred pharmacy networks with three national Medicare Part D plan sponsors: Humana. UnitedHealthcare.
Is CVS Caremark and SilverScript the same?
SilverScript is an affiliate of CVS Caremark. Your new plan through SilverScript will be the only prescription drug plan for Medicare-eligible Retirees of MPIHP.
Is Aetna and SilverScript the same?
SilverScript is a Medicare Prescription Drug Plan (PDP) owned by CVS Health. As Aetna is also owned by CVS Health, we are integrating our plans with SilverScript.
What is the preferred pharmacy for SilverScript?
SilverScript Preferred Pharmacies Walmart, CVS, Wegmans, Kroger, and Publix are a few of the most popular pharmacy choices. However, many local and independent pharmacies also accept SilverScript coverage.
Is Aetna is a CVS Health company that offers SilverScript Part D products?
Aetna is a CVS Health company that offers SilverScript Part D products. Mail order prescription drug services are not available for SilverScript PDP plans.
Is SilverScript owned by CVS or Aetna?
Since 2006, CVS has sold its individual PDPs through a wholly-owned subsidiary called SilverScript Insurance Company.
Is Aetna SilverScript a good plan?
All of Aetna's PDPs have a Medicare star quality rating of 3.5 out of five stars. CVS/Aetna's SilverScript Smart RX plan has the lowest average monthly premium in 2022, and CVS is one of four main providers of stand-alone Part D prescription drug plans in the United States.
Has SilverScript been bought by Aetna?
SilverScript and Aetna will continue to operate as separate organizations with separate pharmacy networks and formularies during the 2019 plan year. As our integration progresses, SilverScript & Aetna leaders will be reviewing all components of plan designs for future plan year offerings.
Is SilverScript changing to Aetna in 2021?
What is SilverScript? SilverScript is one of the largest providers offering Medicare Part D coverage in the United States, with plans in all 50 states. It became part of Aetna Medicare for the 2021 health plan year.
What is CVS SilverScript?
SilverScript Choice is a basic plan that offers comprehensive coverage. Enrolled beneficiaries can benefit from a $0-deductible on all covered drugs in most states and $0-copays for 90-day supplies of Tier 1 drugs nationwide when filled through the CVS Caremark Mail Service Pharmacy.
What is the most popular Medicare Part D plan?
Best-rated Medicare Part D providersRankMedicare Part D providerMedicare star rating for Part D plans1Kaiser Permanente4.92UnitedHealthcare (AARP)3.93BlueCross BlueShield (Anthem)3.94Humana3.83 more rows•Mar 16, 2022
What is the difference between standard and preferred pharmacy?
When your pharmacy is a 'Preferred Pharmacy', you get lower pricing and often are allowed to get 90 day supplies of your medications. When your pharmacy is a 'Standard Pharmacy' the pricing will be higher for you on each and every prescription. You also may not be allowed to get 90 day supplies of your medications.
Why do we call them network pharmacies?
We call them network pharmacies because we’ve contracted with them to provide prescription drugs to Aetna Medicare plan members. In most cases, your prescriptions are covered under our plan only if they’re filled either: By a network pharmacy. Through our mail‐order pharmacy service. Once you go to a pharmacy, you’re not required to keep using ...
How long does it take to get a prescription from mail order?
You should expect to get your prescription drugs 7 to 14 business days from the time the mail‐order pharmacy receives the order. If you don’t receive your prescription drug (s) within this time frame, please call us at the number on your ID card. You may have the option to sign up for automated mail‐order delivery.
Can I use the same pharmacy for my prescription?
Once you go to a pharmacy, you’re not required to keep using the same pharmacy to fill your prescriptions. You can switch to any of our other network pharmacies. We’ll fill prescriptions at non-network pharmacies under certain circumstances. See those circumstances in the Evidence of Coverage.
Find pharmacy information
We know it’s important to find a pharmacy that accepts your plan. Search our online directories to find a pharmacy near you:
Network Specialty Pharmacy
Some long-term health conditions - such as multiple sclerosis, rheumatoid arthritis or cancer - require special medicines. They need to be sent quickly, safely and securely. With a network specialty pharmacy*, you can get these drugs by mail - sent to your home, doctor's office or anywhere you choose. With free standard shipping, too.
Get extra support with your pharmacy coverage
Being an Aetna prescription drug plan member has its perks. Our support programs offer extra help to people who have diabetes.
Support for some complex health conditions
Treatment for certain chronic conditions often means taking a specialty drug. However, you don't have to do it alone. A nurse from the care management team can help you through your treatment.
More about your medications
See if a prescription drug is covered. You’ll need the name of your pharmacy plan.
Our URAC pharmacy accreditations
URAC is an independent, non-profit health care accrediting organization dedicated to promoting health care quality through accreditation, education, and measurement.
When did Medicare Part D start?
Congress authorized Medicare Part D Prescription Drug Plans under the Medicare Prescription Drug, Improvement, and Modernization Act of 2003, making Medicare prescription drug coverage available to beneficiaries for the first time in 2006. Medicare prescription drug is available in one of two ways. You can get Aetna Medicare Part D coverage ...
What is tiered formulary?
Some Aetna Medicare Prescription Drug Plans and Medicare Advantage Prescription Drug plans use a “tiered” formulary, which means that you pay less for certain types of medications, usually generics, than you do for brand-name medications.
Does Aetna cover prescription drugs?
Some things to know about Aetna Medicare plans that cover prescription drugs: Covered drugs are limited to those included in the plan’s drug formulary, which is a list of medications covered by the plan and details about how much the plan will cover. Formularies may vary by plan and location and may change at any time.
Does Aetna have a Medicare Advantage Plan?
An Aetna Medicare Advantage plan with prescription drug coverage gives you the flexibility of having all your Medicare benefits administered under one plan. Or, you can also get your Part D coverage through a stand-alone Medicare Part D Prescription Drug Plan that works alongside Original Medicare.
Does Aetna have a prescription drug plan?
Some Aetna Medicare plans with prescription drug coverage may include coverage above the minimum requirements .
Does Aetna require copayment?
Formularies may vary by plan and location and may change at any time. Your Aetna Medicare plan will notify you if necessary. You may be required to pay a copayment or coinsurance for your prescription drugs.
Check our drug list
Search our formulary for covered drugs and get the information you need. It shows the drugs we cover, the tier a drug is on, any limits or requirements and mail order availability. Generally, the lower the tier, the less you pay. Your Summary of Benefits tells you the drug costs for tiers.
Get our full drug list and more
See a complete list of our covered drugs and other important prescription drug information.
Find a drug by name
Search for a specific drug by name and see if generic equivalents are available. Enter your ZIP code to get started.
Much more than prescription coverage
You get coverage for most medicine plus resources to help you stay informed, save money and take your medicine as prescribed.
Is my medicine covered?
See your plan details for covered medicine and costs. Or visit our online formulary to find less-costly alternatives. Don’t see this information or need your plan name? Just ask your employer.
Retail pharmacy for occasional prescriptions
For medicine you need to take short terms, like antibiotics, you can visit any retail pharmacy. For the best price, choose a network pharmacy.
Home delivery pharmacy for long-term prescriptions
For medicine to treat conditions like high blood pressure, you can get your medicine safely mailed to you at no extra charge. And you may get up to a 90-day supply.*
Step 1: Sign up for a prescription plan
Review your plan materials to see covered medicines and costs, then sign up during open enrollment.
Step 2: Explore your member website
This is your place to find a pharmacy, compare costs, order medicine and learn about your plan.
Step 3: Save money with your plan
Use network pharmacies, compare costs and ask your doctor about lower-price options.