What are considered diabetic shoes?
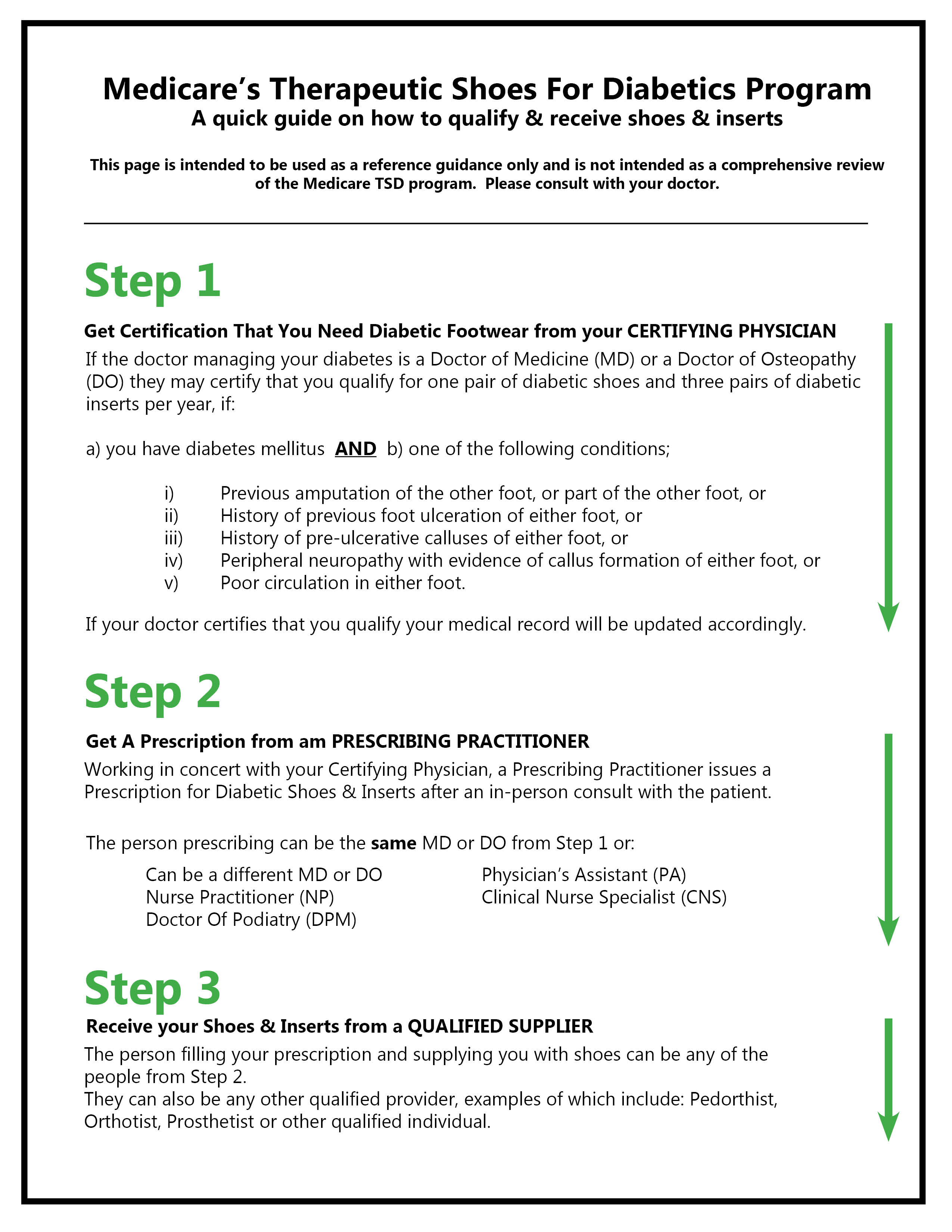
Do you need a prescription for diabetic shoes?
Can podiatrist prescribe diabetic shoes?
Does Medicare pay for SAS shoes?
What is the difference between a regular shoe and a diabetic shoe?
Does Social Security pay for diabetic shoes?
Does Medicare pay for toenail clipping for diabetics?
Are diabetic shoes considered durable medical equipment?
Does Medicare pay for shoe inserts?
What does SAS shoes stand for?
Does insurance cover diabetic shoes?
Are SAS shoes made of leather?
Who must certify your need for therapeutic shoes or inserts?
The doctor who treats your diabetes must certify your need for therapeutic shoes or inserts.
What are therapeutic shoes?
Therapeutic shoes & inserts 1 One pair of custom-molded shoes and inserts 2 One pair of extra-depth shoes
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B.
Does Medicare cover therapeutic shoes?
Medicare will only cover your therapeutic shoes if your doctors and suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare. If your doctors or suppliers aren't enrolled, Medicare won't pay the claims submitted by them. It's also important to ask your suppliers ...
Does Medicare cover custom molded shoes?
One pair of custom-molded shoes and inserts. One pair of extra-depth shoes. Medicare also covers: 2 additional pairs of inserts each calendar year for custom-molded shoes. 3 pairs of inserts each calendar year for extra-depth shoes. Medicare will cover shoe modifications instead of inserts.
Does Medicare cover shoe modifications?
Medicare will cover shoe modifications instead of inserts.
Do suppliers have to accept assignment for therapeutic shoes?
It's also important to ask your suppliers if they participate in Medicare before you get therapeutic shoes. If suppliers are participating suppliers, they must accept assignment. If suppliers are enrolled in Medicare but aren't "participating," they may choose not to accept assignment.
How many pairs of shoes can you get with Medicare?
Under Part B coverage and cost-sharing rules, you may be able to receive one pair of shoes each calendar year. If your shoes are custom-molded, Part B may also provide coverage for two more pairs of inserts. If you use extra-depth prescription shoes, then you may have coverage for three pairs of inserts.
Why do diabetics wear prescription shoes?
If you’re a diabetic and are experiencing pain or numbness in your legs and feet , it may be a sign that you need prescription shoes to help you manage your symptoms. If you’re struggling with other issues, such as recurring blisters, pre-ulcerative calluses, ulcers, foot deformity or below average circulation, your doctor may also recommend diabetic shoes to prevent these symptoms from worsening.
What are diabetic shoes made of?
Their exterior is often made of a supple leather or soft fabric material with foam padding across the top of the foot and around the collar of the shoe.
What is Medicare Part B?
Special shoes and inserts can help prevent these conditions, and Medicare Part B (Medical Insurance) coverage may provide patients with help covering the costs.
Why are inserts called therapeutic shoes?
These materials are also selected for their ability to reduce moisture, which can cause a bacterial infection. Because of their enhanced features , these shoes may also be called extra depth shoes or therapeutic shoes.
Why are shoes better for work?
Because maintaining mobility plays such a key role in managing diabetes, choosing the right kind of shoes is important .
Does Medicare cover diabetic shoes?
Though these shoes require a prescription, they are considered durable medical equipment in most cases. This means they fall under Medicare Part B coverage and cost-sharing rules.
How often does a diabetic foot ulcer occur?
Every 1.2 seconds someone with diabetes develops a diabetic foot ulcer. This can lead to tissue death, amputation, sepsis, and death.
Does Medicare cover shoe modifications?
Medicare also covers shoe modifications in place of inserts.
Do diabetic shoes have to be created equal?
All shoes are not created equal. To qualify as a diabetic shoe, certain standards must be met:
Who can prescribe therapeutic shoes?
In order to receive payment for therapeutic shoes and inserts, Medicare also requires: A podiatrist or other qualified doctor to prescribe the shoes. A doctor or other qualified professional, such as a pedorthist, orthotist, or prosthetist fits and provides the shoes.
What is a doctor who fits shoes?
A doctor or other qualified professional, such as a pedorthist, orthotist, or prosthetist fits and provides the shoes
How many pairs of inserts are there in a shoe?
1. One pair of depth-inlay shoes and three pairs of inserts. 2. One pair of custom-molded shoes (including inserts) and two additional pairs of inserts. Separate inserts may be covered under certain criteria.
What are the conditions that affect the foot?
2. Has one or more of the following conditions in one or both feet: history of partial or complete foot amputation. history of previous foot ulceration. history of preulcerative callus. nerve damage because of diabetes with signs of problems with calluses. poor circulation.
Does Medicare cover diabetic shoes?
Medicare Coverage of Therapeutic Footwear for People with Diabetes. Medicare provides coverage for depth-inlay shoes, custom-molded shoes, and shoe inserts for people with diabetes who qualify under Medicare Part B. Designed to prevent lower-limb ulcers and amputations in people who have diabetes, this Medicare benefit can prevent suffering ...
What doctor can prescribe diabetic shoes?
In order for diabetic shoes to qualify for coverage, a podiatrist or another kind of qualified doctor has to prescribe them. Additionally, a podiatrist, prosthetist, orthotist, pedorthist, or other qualified type of professional has to provide the therapeutic shoes.
Why do diabetic feet hurt?
Diabetics may suffer from diabetic neuropathy. This type of nerve damage may make feet vulnerable to injuries in a few different ways, according to the National Institutes of Health: Injuries may take longer to heal because of restricted blood flow.
How many pairs of inserts does Part B cover?
For custom-molded shoes, Part B may cover up to two pairs of inserts each year. For extra-depth shoes, Part B may cover up to three pairs of inserts each year.
Does Medicare cover shoe inserts?
Medicare may cover shoe modifications instead of inserts in some situations.
Can Medicare pay more than approved?
You will want to make sure your Medicare supplier accepts Medicare assignment, so you can avoid paying more than the Medicare-approved amount.
Can diabetics wear custom shoes?
The National Institute of Health, or NIH, recommends checking with a doctor about special diabetic shoes and/or shoe inserts. In some cases, diabetics may need custom-made shoes to provide extra protection.
What happens if your shoes don't fit in Medicare?
If the shoes do not fit, the Medicare Provider orders a different style/size/width. Once those shoes arrive, the Provider once again visits with the patient to fit the shoes and inserts and goes through the process again.
How often can you get diabetic shoes?
If you're satisfied with the options available, you can receive one pair of Diabetic Shoes and appropriate Inserts, once per calendar year.
Can you order diabetic shoes online?
Ordering Diabetic Shoes on-line can be a difficult process since there are hundreds of options to choose from. With so many options available it's very difficult to decide which is the best solution. It sure helps to have a Specialist to consult with, who understands the patient , their conditions, and the perfect shoes to match their needs.
Does Medicare require a thorough examination of the patient's feet?
The Medicare Provider, has to first visit with the patient (in person) and examine their feet. They document the Medical Necessity, provide a thorough examination, and measurement of the patient's feet.
Does Medicare charge for shoes?
Once the shoes and inserts arrive, the Medical Provider then meets with the patient again and fits them with the shoe that was ordered (including the inserts). If everything fits properly, the patient signs off on the documentation and the Medical Provider company then bills Medicare. There is typically no charge to the patient depending upon the Medicare insurance policy that they have.
What is a POD in Medicare?
Proof of delivery (POD) is a Supplier Standard and DMEPOS suppliers are required to maintain POD documentation in their files. Proof of delivery documentation must be made available to the Medicare contractor upon request. All services that do not have appropriate proof of delivery from the supplier shall be denied as not reasonable and necessary.
What does "gy" mean in Medicare?
GY - Item or service statutorily excluded or does not meet the definition of any Medicare benefi
What is custom molded shoe?
A custom molded shoe (A5501) is covered when the beneficiary has a foot deformity that cannot be accommodated by a depth shoe. The nature and severity of the deformity must be well documented in the supplier's records and available upon request. If a custom molded shoe is provided but the medical record does not document why that item is medically necessary, it will be denied as not reasonable and necessary.
Do DMEPOS require a WOPD?
For DMEPOS base items that require a WOPD, and also require separately billed associated options, accessories, and/or supplies, the supplier must have received a WOPD which lists the base item and which may list all the associated options, accessories, and/or supplies that are separately billed prior to the delivery of the items. In this scenario, if the supplier separately bills for associated options, accessories, and/or supplies without first receiving a completed and signed WOPD of the base item prior to delivery, the claim (s) shall be denied as not reasonable and necessary.
Can diabetic shoes be covered by separate inserts?
Separate inserts may be covered and dispensed independently of diabetic shoes if the supplier of the shoes verifi es in writing that the beneficiar y has appropriate footwear into which the insert can be placed. This footwear must meet the definitions found in this policy for depth shoes or custom-molded shoes.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.